Abstract
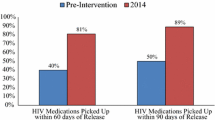
New York City (NYC) jails are the epicenter of an epidemic that overwhelmingly affects Black and Hispanic men and offer a significant opportunity for public health intervention. The NYC Department of Health and Mental Hygiene instituted population based approaches to identify the HIV-infected, initiate discharge planning at jail admission, and facilitate post-release linkages to primary care. Using a caring and supportive ‘warm transitions’ approach, transitional care services are integral to continuity of care. Since 2010, over three-quarters of known HIV-infected inmates admitted to jails received discharge plans; 74 % of those released were linked to primary care. The EnhanceLink initiative’s new Health Liaison, a lynchpin role, facilitated 250 court-led placements in medical alternatives to incarceration. Transitional care coordination programs are critical to facilitate continuity of care for people with chronic health conditions including the HIV-infected returning home from jail and for the public health of the communities to which they return.



Similar content being viewed by others
References
HIV/AIDS Annual Surveillance Statistics. New York: New York City Department of Health and Mental Hygiene, 2010. Available at: http://www.nyc.gov/html/doh/html/ah/hivtables.shtml. Accessed 18 Jan, 2012.
Drucker E. Plague of prisons: the epidemiology of mass incarceration in America. New York: The New Press; 2011.
Begier E, Bennani Y, Forgione L, et al. Undiagnosed HIV infection among New York City jail entrants, 2006: results of a blinded serosurvey. J Acquir Immune Defic Syndr. 2010;54:93–101.
Karpati A, Kerker B, Mostashari F, et al. Health disparities in New York City. New York: New York City Department of Health and Mental Hygiene; 2004.
Spaulding A, Stephenson B, Macalino G, Ruby W, Clarke JG, Flanigan TP. Human immunodeficiency virus in correctional facilities: a review. Clin Infect Dis. 2002;35(3):305–12.
Flanigan TP, Zaller N, Beckwith CG, et al. Testing for HIV, sexually transmitted infections, and viral hepatitis in jails: still a missed opportunity for public health and HIV prevention. J Acquir Immune Defic Syndr. 2010;55(Suppl 2):S78–83.
Conklin TJ, Lincoln T, Flanigan TP. A public health model to connect correctional health care with communities. Am J Public Health. 1998;88(8):1249–50.
HIV Epidemiology and Field Services Semiannual Report. New York: New York City Department of Health and Mental Hygiene, October 2010. Available at: http://home2.nyc.gov/html/doh/downloads/pdf/dires/2010_2nd_semi_rpt.pdf. Accessed 18 Jan, 2012.
Sackoff JE, Hanna DB, Pfeiffer MR, Torian LV. Causes of death among persons with AIDS in the era of highly active antiretroviral therapy: New York City. Ann Intern Med. 2006;145:397–406.
DOC Facilities Overview: New York Department of Corrections, 2011. Available at: http://www.nyc.gov/html/doc/html/about/facilities_overview.shtml. Accessed 31 Jan, 2012.
DOC Statistics. New York: New York Department of Corrections, 2001-2010. Available at: http://www.nyc.gov/html/doc/html/stats/doc_stats.shtml. Accessed 18 Jan, 2012.
Board of Corrections Health Care Minimum Standards, 2012. Available at: http://www.nyc.gov/html/boc/downloads/pdf/healthcare_standards.pdf. Accessed 18 Jan, 2012.
Mellow J, Belkin G, Greifinger RB, et al. Mapping the innovation of correctional health care service delivery in New York City. John Jay College of Criminal Justice, City University of New York; 2008. (See Page 85 for Health Passport) Available at: http://www.jjay.cuny.edu/NYCMappingHeathCare.pdf. Accessed 1 Oct, 2012.
Jordan A, Ouellet L. Enhancing linkages to primary care and services in jail settings initiative: transitional care coordination – from incarceration to the community. Emory University; Enhancelink policy brief; 2010. Available at: http://www.enhancelink.org/EnhanceLink/documents/Transitional_Care_Coordination--Fall2010.pdf. Accessed 25 Oct, 2012.
DuBois B, Miley KK. Social work: an empowering profession. Boston: Allyn and Bacon. 1992. p. 135–141.
Whitaker W, Lemons FD. Turning the game around: NYC can help. New York: NYC Commission on Human Rights; 2011.
Laraque F. HIV Care coordination program in NYC: an evidence based intervention. NYC Department of Health and Mental Hygiene; 2009. Available at: http://www.nyc.gov/html/doh/downloads/pdf/ah/ah-hiv-care-cord-program-nyc.pdf. Accessed 25 Oct, 2012.
Zimmerman GL, Olsen CG, Bosworth DO. A ‘stages of change’ approach to helping patients change behavior. Am Fam Physician. 2000;61(5):1409–16.
Gardner EM, McLees MP, Steiner JF, del Rio C, Burman WJ. The spectrum of engagement in HIV care and its relevance to test-and-treat strategies for prevention of HIV infection. Clin Infect Dis. 2011;52(6):793–800.
Draine J, Ahuja D, Altice FL, et al. Strategies to enhance linkages between care for HIV/AIDS in jail and community settings. AIDS Care. 2011;23(3):366–77.
Booker CA, Flygare CT, Solomon L, Ball SW, Pustell MR, Bazerman LB, Simon-Levine D, Teixeira PA, Cruzado-Quinones J, Kling RN, Spaulding A, et al. Linkage to HIV care for jail detainees: findings from detention to the first 30 days after release. AIDS Behav. doi:10.1007/s10461-012-0354-3.
Jaffer M, Kimura C, Venters H. Improving medical care for patients with HIV in New York City jails. J Correct Health Care. 2012;00:1–5.
Nelson M, Trone J. Why planning for release matters. Vera Institute of Justice. 2000. p. 1–8.
Chen NE, Meyer JP, Avery AK, et al. Adherence to HIV treatment and care among previously homeless jail detainees. AIDS Behav. 2011. p. 1–13.
Nunn A, Cornwall A, Fu J, Bazerman L, Loewenthal H, Beckwith C. Linking HIV-positive jail inmates to treatment, care, and social services after release: results from a qualitative assessment of the COMPASS program. J Urban Health. 2010;87(6):954–68.
Nemcek MA, Sabatier R. State of evaluation: community health workers. Public Health Nurs. 2003;20(4):260–70.
Freudenberg N, Moseley J, Labriola M, Daniels J, Murrill C. Comparison of health and social characteristics of people leaving New York City jails by age, gender, and race/ethnicity: implications for public health interventions. Public Health Rep. 2007;122:733–43.
Meyer JP, Chen NE, Springer SA. HIV treatment in the criminal justice system: critical knowledge and intervention gaps. AIDS Res Treat. 2011;2011:1–13.
Beckwith CG, Zaller ND, Fu JJ, Montague BT, Rich JD. Opportunities to diagnose, treat, and prevent HIV in the criminal justice system. J Acquir Immune Defic Syndr. 2010;55(Suppl 1):S49–55.
Gardner LI, Metsch LR, Anderson-Mahoney P, et al. Efficacy of a brief case management intervention to link recently diagnosed HIV-infected persons to care. AIDS. 2005;19:423–31.
Acknowledgments
The authors gratefully acknowledge Thomas Frieden, Thomas Farley, Fabienne Laraque, Beau Mitts, Amanda Parsons, Anthony Santella, Jonathan Santos Ramos, and the Correctional Health Services leadership team for their vision and leadership; Sam Amirfar, Robin Cagey, Joanna Eavey, Traciah John, Tatiana Tikhonko, and the DOHMH HIV Surveillance and Research unit for their contributions to this study; Press Canady, Allison Dansby, Brenda Ortiz-Rivera, Cheryl Moorehead, the Rikers Island Transitional Consortium, and our dedicated staff for making a difference every day. This publication was made possible by a Grant through the U.S. Department of Health and Human Services (DHHS), Health Resources and Services Administration, HIV Bureau. The content of this publication does not necessarily reflect the views or policies of DHHS. Responsibility for the content of this report rests solely with the named authors.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Jordan, A.O., Cohen, L.R., Harriman, G. et al. Transitional Care Coordination in New York City Jails: Facilitating Linkages to Care for People with HIV Returning Home from Rikers Island. AIDS Behav 17 (Suppl 2), 212–219 (2013). https://doi.org/10.1007/s10461-012-0352-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10461-012-0352-5