Abstract
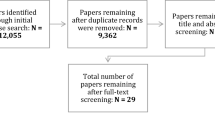
Although feedback has been identified as a key instructional feature in simulation based medical education (SBME), we remain uncertain as to the magnitude of its effectiveness and the mechanisms by which it may be effective. We employed a meta-analysis and critical narrative synthesis to examine the effectiveness of feedback for SBME procedural skills training and to examine how it works in this context. Our results demonstrate that feedback is moderately effective during procedural skills training in SBME, with a pooled effect size favoring feedback for skill outcomes of 0.74 (95 % CI 0.38–1.09; p < .001). Terminal feedback appears more effective than concurrent feedback for novice learners’ skill retention. Multiple sources of feedback, including instructor feedback, lead to short-term performance gains although data on long-term effects is lacking. The mechanism by which feedback may be operating is consistent with the guidance hypothesis, with more research needed to examine other mechanisms such as cognitive load theory and social development theory.





Similar content being viewed by others
References
Archer, J. C. (2010). State of the science in health professional education: Effective feedback. Medical Education, 44(1), 101–108.
Backstein, D., Agnidis, Z., Sadhu, R., & MacRae, H. (2005). Effectiveness of repeated video feedback in the acquisition of a surgical technical skill. Canadian Journal of Surgery, 48(3), 195–200.
Borenstein, M. (2009). Effect sizes for continuous data. In H. Cooper, L. V. Hedges, & J. C. Valentine (Eds.), The handbook of research synthesis and meta-analysis (2nd ed.). New York, NY, US: Russell Sage Foundation.
Byrne, A. J., Sellen, A. J., Jones, J. G., Aitkenhead, A. R., Hussain, S., Gilder, F., et al. (2002). Effect of videotape feedback on anaesthetists’ performance while managing simulated anaesthetic crises: A multicentre study. Anaesthesia, 57(2), 176–179.
Chang, J.-Y., Chang, G.-L., Chien, C.-J. C., Chung, K.-C., & Hsu, A.-T. (2007). Effectiveness of two forms of feedback on training of a joint mobilization skill by using a joint translation simulator. Physical Therapy, 87(4), 418–430.
Chang, S., Waid, E., Martinec, D. V., Zheng, B., & Swanstrom, L. L. (2008). Verbal communication improves laparoscopic team performance. Surgical Innovation, 15(2), 143–147.
Cohen, J. (1988). Statistical power analysis for the behavioral sciences (2nd ed.). Hillsdale, NJ: Lawrence Erlbaum.
Cook, D. A., Bordage, G., & Schmidt, H. G. (2008). Description, justification and clarification: A framework for classifying the purposes of research in medical education. Medical Education, 42(2), 128–133.
Cook, D. A., Brydges, R., Hamstra, S. J., Zendejas, B., Szostek, J. H., Wang, A. T., et al. (2012). Comparative effectiveness of technology-enhanced simulation versus other instructional methods: A systematic review and meta-analysis. Simulation in Healthcare: Journal of the Society for Simulation in Healthcare, 7(5), 308–320.
Cook, D. A., Hamstra, S. J., Brydges, R., Zendejas, B., Szostek, J. H., Wang, A. T., et al. (2013). Comparative effectiveness of instructional design features in simulation-based education: Systematic review and meta-analysis. Medical Teacher, 35(1), e867-98.
Cook, D. A., Hatala, R., Brydges, R., Zendejas, B., Szostek, J. H., Wang, A. T., et al. (2011). Technology-enhanced simulation for health professions education: A systematic review and meta-analysis. The Journal of the American Medical Association, 306(9), 978–988.
Day, T., Iles, N., & Griffiths, P. (2009). Effect of performance feedback on tracheal suctioning knowledge and skills: Randomized controlled trial. Journal of Advanced Nursing, 65(7), 1423–1431.
Dine, C. J., Gersh, R. E., Leary, M., Riegel, B. J., Bellini, L. M., & Abella, B. S. (2008). Improving cardiopulmonary resuscitation quality and resuscitation training by combining audiovisual feedback and debriefing*. Critical Care Medicine, 36(10), 2817–2822.
Domuracki, K. J., Moule, C. J., Owen, H., Kostandoff, G., & Plummer, J. L. (2009). Learning on a simulator does transfer to clinical practice. Resuscitation, 80(3), 346–349.
Dunphy, B., & Dunphy, S. (2003). Assisted performance and the Zone of Proximal Development (ZPD); a potential framework for providing surgical education. Australian Journal of Educational & Developmental Psychology, 3, 48–58.
Ende, J. (1983). Feedback in clinical medical education. The Journal of the American Medical Association, 250, 777–781.
Enebo, B., & Sherwood, D. (2005). Experience and practice organization in learning a simulated high-velocity low-amplitude task. Journal of Manipulative and Physiological Therapeutics, 28(1), 33–43.
Gerling, G. J., & Thomas, G. W. (2003). Effect of augmented visual performance feedback on the effectiveness of clinical breast examination training with a dynamically configurable breast model. In Systems, man and cybernetics, 2003. IEEE international conference on, 3, 2095–2100 vol. 3.
Gurusamy, K., Aggarwal, R., Palanivelu, L., & Davidson, B. R. (2008). Systematic review of randomized controlled trials on the effectiveness of virtual reality training for laparoscopic surgery. British Journal of Surgery, 95(9), 1088–1097.
Higgins, E. T. (1997). Beyond pleasure and pain. The American Psychologist, 52(12), 1280–1300.
Higgins, J. P. T., Thompson, S. G., Deeks, J. J., & Altman, D. G. (2003). Measuring inconsistency in meta-analyses. British Medical Journal, 327(7414), 557–560. (Clinical research ed.).
Hunter, J., & Schmidt, F. (2004). Methods of meta-analysis: Correcting error and bias in research findings. Thousand Oaks, CA: Sage.
Issenberg, S. B., McGaghie, W. C., Petrusa, E. R., Lee Gordon, D., & Scalese, R. J. (2005). Features and uses of high-fidelity medical simulations that lead to effective learning: A BEME systematic review. Medical Teacher, 27(1), 10–28.
Kahol, K., French, J., McDaniel, T., Panchanathan, S., & Smith, M. (2007). Augmented virtual reality for laparoscopic surgical tool training. In Proceedings of the 12th international conference on human–computer interaction: Applications and services, pp. 459–467.
Kirkpatrick, D. L., & Kirkpatrick, J. D. (2009). Evaluating training programs (3rd ed.). San Francisco: Berrett-Koehler.
Kluger, A. N., & DeNisi, A. (1996). The effects of feedback interventions on performance: A historical review, a meta-analysis, and a preliminary feedback intervention theory. Psychological Bulletin, 119(2), 254–284.
Kovacs, G., Bullock, G., Ackroyd-Stolarz, S., Cain, E., & Petrie, D. (2000). A randomized controlled trial on the effect of educational interventions in promoting airway management skill maintenance. Annals of Emergency Medicine, 36(4), 301–309.
Kruglikova, I., Grantcharov, T. P., Drewes, A. M., & Funch-Jensen, P. (2010). The impact of constructive feedback on training in gastrointestinal endoscopy using high-fidelity virtual-reality simulation: A randomised controlled trial. Gut, 59(2), 181–185.
Lazarski, M. P., Susarla, S. M., Bennett, N. L., & Seldin, E. B. (2007). How do feedback and instructions affect the performance of a simulated surgical task? Journal of Oral and Maxillofacial Surgery, 65(6), 1155–1161.
Ma, I. W. Y., Brindle, M. E., Ronksley, P. E., Lorenzetti, D. L., Sauve, R. S., & Ghali, W. A. (2011). Use of simulation-based education to improve outcomes of central venous catheterization: A systematic review and meta-analysis. Academic Medicine, 86(9), 1137–1147.
McGaghie, W. C., Issenberg, S. B., Petrusa, E. R., & Scalese, R. J. (2010). A critical review of simulation-based medical education research: 2003–2009. Medical Education, 44(1), 50–63.
Moher, D., Liberati, A., Tetzlaff, J., Altman, D. G., PRISMA Group. (2009, October). Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. Journal of Clinical Epidemiology, 62, 1006–1012.
Morris, S. B., & DeShon, R. P. (2002). Combining effect size estimates in meta-analysis with repeated measures and independent-groups designs. Psychological Methods, 7(1), 105–125.
Moulton, C., Tabak, D., Kneebone, R., Nestel, D., MacRae, H., & LeBlanc, V. R. (2009). Teaching communication skills using the integrated procedural performance instrument (IPPI): A randomized controlled trial. American Journal of Surgery, 197(1), 113–118.
O’Connor, A., Schwaitzberg, S. D., & Cao, C. G. L. (2007). How much feedback is necessary for learning to suture? Surgical Endoscopy, 22(7), 1614–1619.
Passiment, M., Sacks, H., & Huang, G. (2011). Medical simulation in medical education: Results of an AAMC Survey (pp. 1–48). Washington, DC: Association of American Medical Colleges.
Pawson, R., Greenhalgh, T., Harvey, G., & Walshe, K. (2005). Realist review—A new method of systematic review designed for complex policy interventions. Journal of Health Services Research & Policy, 10(Suppl 1), 21–34.
Porte, M. C., Xeroulis, G., Reznick, R. K., & Dubrowski, A. (2007). Verbal feedback from an expert is more effective than self-accessed feedback about motion efficiency in learning new surgical skills. American Journal of Surgery, 193(1), 105–110.
Pugh, C. M., Srivastava, S., Shavelson, R., Walker, D., Cotner, T., Scarloss, B., et al. (2001). The effect of simulator use on learning and self-assessment: The case of Stanford University’s E-Pelvis simulator. Studies in Health Technology and Informatics, 81, 396–400.
Quinn, F., Keogh, P., McDonald, A., & Hussey, D. (2003). A study comparing the effectiveness of conventional training and virtual reality simulation in the skills acquisition of junior dental students. European Journal of Dental Education : Official Journal of the Association for Dental Education in Europe, 7(4), 164–169.
Rafiq, A., Tamariz, F., Boanca, C., Lavrentyev, V., & Merrell, R. C. (2008). Objective assessment of training surgical skills using simulated tissue interface with real-time feedback. Journal of Surgical Education, 65(4), 270–274.
Reed, D. A., Cook, D. A., Beckman, T. J., Levine, R. B., Kern, D. E., & Wright, S. M. (2007). Association between funding and quality of published medical education research. The Journal of the American Medical Association, 298(9), 1002–1009.
Rissanen, M. J., Kume, N., Kuroda, Y., Kuroda, T., Yoshimura, K., & Yoshihara, H. (2008). Asynchronous teaching of psychomotor skills through VR annotations: Evaluation in digital rectal examination. Studies in Health Technology and Informatics, 132, 411–416.
Roediger, H. L., & Butler, A. C. (2011). The critical role of retrieval practice in long-term retention. Trends in Cognitive Sciences, 15(1), 20–27.
Rosser, J. C, Jr, Colsant, B. J., Lynch, P. J., Herman, B., Klonsky, J., & Young, S. M. (2006). The use of a “hybrid” trainer in an established laparoscopic skills program. Journal of the Society of Laparoendoscopic Surgeons, 10(1), 4.
Scaringe, J. (2002). The effects of augmented sensory feedback precision on the acquisition and retention of a simulated chiropractic task. Journal of Manipulative and Physiological Therapeutics, 25(1), 34–41.
Schmidt, R., & Lee, T. (2011). Motor control and learning: A behavioral emphasis (5th ed.). Champaign: Human Kinetics.
Shute, V. (2008). Focus on formative feedback. Review of Educational Research, 78, 153–189.
Spooner, B. B., Fallaha, J. F., Kocierz, L., Smith, C. M., Smith, S. C. L., & Perkins, G. D. (2007). An evaluation of objective feedback in basic life support (BLS) training. Resuscitation, 73(3), 417–424.
Stefanidis, D., Korndorffer, J. R, Jr, Heniford, B. T., & Scott, D. J. (2007). Limited feedback and video tutorials optimize learning and resource utilization during laparoscopic simulator training. Surgery, 142(2), 202–206.
Sutherland, L. M., Middleton, P. F., Anthony, A., Hamdorf, J., Cregan, P., Scott, D., et al. (2006). Surgical simulation: A systematic review. Annals of Surgery, 243(3), 291–300.
van Merrienboer, J. J. G., & Sweller, J. (2010). Cognitive load theory in health professional education: Design principles and strategies. Medical Education, 44(1), 85–93.
Van Merriënboer, J. J. G., & Sweller, J. (2005). Cognitive load theory and complex learning: Recent developments and future directions. Educational Psychology Review, 17(2), 147–177.
Van Sickle, K. R., Gallagher, A. G., & Smith, C. D. (2007). The effect of escalating feedback on the acquisition of psychomotor skills for laparoscopy. Surgical Endoscopy, 21(2), 220–224.
Veloski, J., Boex, J. R., Grasberger, M. J., Evans, A., & Wolfson, D. B. (2006). Systematic review of the literature on assessment, feedback and physicians’ clinical performance: BEME Guide No. 7. Medical Teacher, 28(2), 117–128.
Vygotsky, L. (1978). Mind in society: The development of higher mental processes. In M. Cole, V. John-Steiner, S. Scribner, & E. Souberman (Eds.), (14th ed.). Harvard University Press.
Walsh, C. M., Ling, S. C., Wang, C. S., & Carnahan, H. (2009). Concurrent versus terminal feedback: It may be better to wait. Academic Medicine : Journal of the Association of American Medical Colleges, 84(10 Suppl), S54–S57.
Watling, C., Driessen, E., van der Vleuten, C. P. M., Vanstone, M., & Lingard, L. (2012). Understanding responses to feedback: The potential and limitations of regulatory focus theory. Medical Education, 46(6), 593–603.
Wierinck, E., Puttemans, V., Swinnen, S., & van Steenberghe, D. (2005). Effect of augmented visual feedback from a virtual reality simulation system on manual dexterity training. European Journal of Dental Education: Official Journal of the Association for Dental Education in Europe, 9(1), 10–16.
Wierinck, E., Puttemans, V., & van Steenberghe, D. (2006a). Effect of reducing frequency of augmented feedback on manual dexterity training and its retention. Journal of Dentistry, 34(9), 641–647.
Wierinck, E., Puttemans, V., & van Steenberghe, D. (2006b). Effect of tutorial input in addition to augmented feedback on manual dexterity training and its retention. European Journal of Dental Education: Official Journal of the Association for Dental Education in Europe, 10(1), 24–31.
Wulf, G., & Shea, C. (2004). Understanding the role of augmented feedback: The good, the bad, and the ugly. In A. Williams & N. Hodges (Eds.), Skill acquisition in sport: Research, theory and practice (1st ed., pp. 121–144). London: Routledge.
Wulf, G., Shea, C., & Lewthwaite, R. (2010). Motor skill learning and performance: A review of influential factors. Medical Education, 44(1), 75–84.
Xeroulis, G. J., Park, J., Moulton, C. A., Reznick, R. K., LeBlanc, V., & Dubrowski, A. (2007). Teaching suturing and knot-tying skills to medical students: A randomized controlled study comparing computer-based video instruction and (concurrent and summary) expert feedback. Surgery, 141(4), 442–449.
Yasukawa, Y. (2009). The effectiveness of cavity preparation training using a virtual reality simulation system with or without feedback. Kōkūbyō Gakkai zasshi. The Journal of the Stomatological Society, Japan, 76(2), 73–80.
Zendejas, B., Brydges, R., Wang, A. T., & Cook, D. A. (2013). Patient outcomes in simulation-based medical education: A systematic review. Journal of General Internal Medicine. doi:10.1007/s11606-012-2264-5
Acknowledgments
The authors thank Patricia Erwin, Jason Szostek, and Amy Wang for their assistance with literature searching, abstract reviewing and data extraction. This work was supported by intramural funds, including an award from the Division of General Internal Medicine, Mayo Clinic.
Conflicts of interest
No relevant conflicts of interest for any of the authors. There was no industry relationship with this work.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Hatala, R., Cook, D.A., Zendejas, B. et al. Feedback for simulation-based procedural skills training: a meta-analysis and critical narrative synthesis. Adv in Health Sci Educ 19, 251–272 (2014). https://doi.org/10.1007/s10459-013-9462-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10459-013-9462-8