Abstract
Aim
The purpose of this review is to describe the use and definitions of the concepts of nurse-patient interaction and nurse-patient communication in nursing literature. Furthermore, empirical findings of nurse-patient communication research will be presented, and applied theories will be shown.
Method
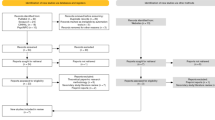
An integrative literature search was executed. The total number of relevant citations found was 97. The search results were reviewed, and key points were extracted in a standardized form. Extracts were then qualitatively summarized according to relevant aspects and categories for the review.
Results
The relation of interaction and communication is not clearly defined in nursing literature. Often the terms are used interchangeably or synonymously, and a clear theoretical definition is avoided or rather implicit. Symbolic interactionism and classic sender-receiver models were by far the most referred to models. Compared to the use of theories of adjacent sciences, the use of original nursing theories related to communication is rather infrequent. The articles that try to clarify the relation of both concepts see communication as a special or subtype of interaction.
The main intention of communication and interaction in the health setting is to influence the patient’s health status or state of well-being. Identified important structural factors of communication were: role allocation, different use of language and registers, and the nursing setting. The process of communication is often described with a phase model; communication often happens during other interventions and tasks. In general, influencing factors can be organized into the categories of provider variables, patient variables, environmental and situational variables.
Conclusion
The included citations all conclude that communication skills can be learned to a certain degree. Involvement of patients and their role in communication often is neglected by authors. Considering the mutual nature of communication, patients’ share in conversation should be taken more into consideration than it has been until now. Nursing science has to integrate its own theories of nursing care with theories of communication and interaction from other scientific disciplines like sociology.
Similar content being viewed by others
References
Aguilera DC (1967) Relationship between physical contact and verbal interaction between nurses and patients. J Psychiatr Nurs Ment Health Serv 5:5–21
Allen CI, Turner PS (1991) The effect of an intervention programme on interactions on a continuing care ward for older people. J Adv Nurs 16:1172–1177
Altschul A (1972) Patient-nurse interaction: A study of interaction patterns in acute psychiatric wards. Churchill Livingstone, Edinburgh
Anderson ND (1979) Human interaction for nurses. Superv Nurse 10(44):48–50
Aranda SK, Street AF (1999) Being authentic and being a chameleon: nurse-patient interaction revisited. Nurs Inq 6:75–82
Armstrong-Esther CA, Browne KD (1986) The influence of elderly patients’ mental impairment on nurse-patient interaction. J Adv Nurs 11:379–387
Barrere CC (2007) Discourse analysis of nurse-patient communication in a hospital setting: implications for staff development. J Nurses Staff 23:114–122 quiz 123–124
Berg L, Skott C, Danielson E (2007) Caring relationship in a context: fieldwork in a medical ward. Int J Nurs Pract 13:100–106
Bourhis RY, Roth S, MacQueen G (1989) Communication in the hospital setting: a survey of medical and everyday language use amongst patients, nurses and doctors. Soc Sci Med 28:339–346
Breeze JA, Repper J (1998) Struggling for control: the care experiences of, difficult’ patients in mental health services. J Adv Nurs 28:1301–1311
Brown JM (1997) Manipulativeness and dialogue. J Psychiatr Ment Health Nurs 4:137–144
Burgio LD, Allen-Burge R, Roth DL, Bourgeois MS, Dijkstra K, Gerstle J, Jackson E, Bankester L (2001) Come talk with me: improving communication between nursing assistants and nursing home residents during care routines. Gerontologist 41:449–460
Canales M (1997) Narrative interaction: creating a space for therapeutic communication. Issues Ment Health Nurs 18:477–494
Caris-Verhallen WM, Kerkstra A, Bensing JM (1997) The role of communication in nursing care for elderly people: a review of the literature. J Adv Nurs 25:915–933
Caris-Verhallen WM, Kerkstra A, van der Heijden PG, Bensing JM (1998) Nurse-elderly patient communication in home care and institutional care: an explorative study. Int J Nurs Stud 35:95–108
Caris-Verhallen WM, de Gruijter IM, Kerkstra A, Bensing JM (1999a) Factors related to nurse communication with elderly people. J Adv Nurs 30:1106–1117
Caris-Verhallen WM, Kerkstra A, Bensing JM (1999b) Non-verbal behaviour in nurse-elderly patient communication. J Adv Nurs 29:808–818
Carlson S (1972) Communication and social interaction in the aged. Nurs Clin North Am 7:269–279
Castledine G (2004) The importance of the nurse-patient relationship. Br J Nurs 13:231
Chatwin J (2008) Hidden dimensions: the analysis of interaction in nurse-patient encounters. Qual Prim Care 16:109–115
Cleary M, Edwards C (1999) ‘Something always comes up’: nurse-patient interaction in an acute psychiatric setting. J Psychiatr Ment Health Nurs 6:469–477
Cleary M, Edwards C, Meehan T (1999) Factors influencing nurse-patient interaction in the acute psychiatric setting: an exploratory investigation. Aust N Z J Ment Health Nurs 8:109–116
Cossette S, Cote JK, Pepin J, Ricard N, D’Aoust L (2006) A dimensional structure of nurse-patient interactions from a caring perspective: refinement of the Caring Nurse-Patient Interaction Scale (CNPI-Short Scale). J Adv Nurs 55:198–214
Darmann I (2000) Anforderungen der Berufswirklichkeit an die kommunikative Kompetenz von Pflegekräften. Pflege 13:219–225
Darmann I (2002) Bewegung als Interaktion – Systemisch-konstruktivistische Sichtweise von Bewegung und Konsequenzen für die Pflege. Pflege 15:181–186
Daubenmire MJ, Searles SS, Ashton CA (1978) A methodologic framework to study nurse-patient communication. Nurs Res 27:303–310
Davies P (1994) Non-verbal communication with patients. Br J Nurs 3:220–223
Dean M, Misra P, Kakkar DN, Kaur J (1982) Hospital interactions: communication by nursing personnel. Nurs J India 73:254–258
Diers D, Schmidt RL, McBride MA, Davis BL (1972) The effect of nursing interaction on patients in pain. Nurs Res 21:419–428
Dornheim J (2003) Verbesserung der kommunikativen Kompetenz von Pflegenden und Gepflegten. Projektbericht. http://www.bosch-stiftung.de
Edberg AK, Nordmark Sandgren A, Hallberg IR (1995) Initiating and terminating verbal interaction between nurses and severely demented patients regarded as vocally disruptive. J Psychiatr Ment Health Nurs 2:159–167
Flaskerud JH (1986) On ‘toward a theory of nursing action: skills and competency in nurse-patient interaction’. Nurs Res 35:250–252
Fosbinder D (1994) Patient perceptions of nursing care: an emerging theory of interpersonal competence. J Adv Nurs 20:1085–1093
Fry A (1994) Effective communication with people with visual disabilities. Nurs Times 90:42–43
Gastmans C (1998) Interpersonal relations in nursing: a philosophical-ethical analysis of the work of Hildegard E. Peplau. J Adv Nurs 28:1312–1319
Gilbert DA (1998) Relational message themes in nurses’ listening behavior during brief patient-nurse interactions. Sch Inq Nurs Pract 12:5–21
Goode ML (2004) Communication barriers when managing a patient with a wound. Br J Nurs 13:49–52
Graneheim UH, Norberg A, Jansson L (2001) Interaction relating to privacy, identity, autonomy and security. An observational study focusing on a woman with dementia and ‘behavioural disturbances’, and on her care providers. J Adv Nurs 36:256–265
Hansebo G, Kihlgren M (2002) Carers’ interactions with patients suffering from severe dementia: a difficult balance to facilitate mutual togetherness. J Clin Nurs 11:225–236
Harding KP (1987) Implications of social interaction. Nursing (Lond) 3:suppl 4–6
Heineken J (1998) Patient silence is not necessarily client satisfaction: communication problems in home care nursing. Home Healthc Nurse 16:115–120
Hewison A (1995a) Nurses’ power in interactions with patients. J Adv Nurs 21:75–82
Hewison A (1995b) Power of language in a ward for the care of older people. Nurs Times 91:32–33
Hollinger LM, Buschmann MB (1993) Factors influencing the perception of touch by elderly nursing home residents and their health caregivers. Int J Nurs Stud 30:445–461
Jones A (2003) Nurses talking to patients: exploring conversation analysis as a means of researching nurse-patient communication. Int J Nurs Stud 40:609–618
Jones DC, van Amelsvoort Jones GM (1986) Communication patterns between nursing staff and the ethnic elderly in a long-term care facility. J Adv Nurs 11:265–272
Kaakinen J, Shapiro E, Gayle BM (2001) Strategies for working with elderly clients: a qualitative analysis of elderly client/nurse practitioner communication. J Am Acad Nurse Pract 13:325–329
Kettunen T, Poskiparta M, Gerlander M (2002) Nurse-patient power relationship: preliminary evidence of patients’ power messages. Patient Educ Couns 47:101–113
Klein ER (2005) Effective communication with patients. Pa Nurse 60:14–15
Koeniger-Donohue R (2007) Nurse practitioner-client interaction as resource exchange: the nurse’s view (NP-client interaction). J Clin Nurs 16:1050–1060
Larsson G, Starrin B (1990) Patient-nurse interactions: relationships between person characteristics, empathy, content of communication, and patients’ emotional reactions. Scand J Caring Sci 4:129–135
Lein C, Wills CE (2007) Using patient-centered interviewing skills to manage complex patient encounters in primary care. J Am Acad Nurse Pract 19:215–220
Lomax B (1997) Learning to understand a patient’s silence. Nurs Times 93:48–49
Loveridge CE, Heineken J (1988) Confirming interactions. J Gerontol Nurs 14:27–30
Luhmann N (1993) Das Recht der Gesellschaft. Suhrkamp, Frankfurt am Main
Mallett J (1999) Difficulties of filming interactions. Nurs Times 95:49
Martin LL, Barkan H (1989) Clinical communication strategies of nurse practitioners with patients. J Am Acad Nurse Pract 1:77–83
Mathews JJ (1983) The communication process in clinical settings. Soc Sci Med 17:1371–1378
May C (1990) Research on nurse-patient relationships: problems of theory, problems of practice. J Adv Nurs 15:307–315
McCann K, McKenna HP (1993) An examination of touch between nurses and elderly patients in a continuing care setting in Northern Ireland. J Adv Nurs 18:838–846
McCutcheon HH, Pincombe J (2001) Intuition: an important tool in the practice of nursing. J Adv Nurs 35:342–348
Millard L, Hallett C, Luker K (2006) Nurse-patient interaction and decision-making in care: patient involvement in community nursing. J Adv Nurs 55:142–150
Moore E, Kuipers L (1992) Behavioural correlates of expressed emotion in staff-patient interactions. Soc Psychiatry Psychiatr Epidemiol 27:298–303
Moreira AS, Rodrigues AR, Coler MS (1997) A model for analysis of the nurse-patient interactive process (MAIP). J Psychiatr Ment Health Nurs 4:303–306
Nordby H (2006) Nurse-patient communication: language mastery and concept possession. Nurs Inq 13:64–72
Nordby H (2007) Meaning and normativity in nurse-patient interaction. Nurs Philos 8:16–27
O’Kelly G (1998) Countertransference in the nurse-patient relationship: a review of the literature. J Adv Nurs 28:391–397
Oliver S, Redfern SJ (1991) Interpersonal communication between nurses and elderly patients: refinement of an observation schedule. J Adv Nurs 16:30–38
Park E, Song M (2005) Communication barriers perceived by older patients and nurses. Int J Nurs Stud 42:159–166
Parsons T (1968) Einige theoretische Betrachtungen zum Bereich der Medizinsoziologie. In: Parsons T (ed) Sozialstruktur und Persönlichkeit. Klotz, Frankfurt am Main, pp 408–449
Routasalo P (1999) Physical touch in nursing studies: a literature review. J Adv Nurs 30:843–850
Routasalo P, Isola A (1998) Touching by skilled nurses in elderly nursing care. Scand J Caring Sci 12:170–178
Ruan J, Lambert VA (2008) Differences in perceived communication barriers among nurses and elderly patients in China. Nurs Health Sci 10:110–116
Ruesch J, Bateson G (1995) Kommunikation: Die soziale Matrix der Psychiatrie. Carl Auer, Heidelberg
Rundell S (1991) A study of nurse-patient interaction in a high dependency unit. Intensive Care Nurs 7:171–178
Salyer J, Stuart BJ (1985) Nurse-patient interaction in the intensive care unit. Heart Lung 14:20–24
Sarvimäki A (1988) Nursing care as a moral, practical, communicative and creative activity. J Adv Nurs 13:462–467
Scheiner R, Knipfer E (2006) Miteinander reden: Wege zu einer gelingenden Kommunikation in der Pflege. Pflege Z 59:Suppl. 2–8
Schiereck S (2000) Soziale Interaktion zwischen Pflegekräften und PatientInnen im Organisationsverlauf einer Nursing Development Unit. Pflege 13:234–241
Schröck R (2003) Interaktionen zwischen Pflegenden und Patienten – Eine klassische Studie in der akuten Psychiatrie. Pflege 16:17–25
Shattell M (2004) Nurse-patient interaction: a review of the literature. J Clin Nurs 13:714–722
Sheldon LK, Barrett R, Ellington L (2006) Difficult communication in nursing. J Nurs Scholarsh 38:141–147
Smith-Stoner M (1999) Language - as important as documentation! Home Healthc Nurse 17:350–352
Spiers JA (2002) The interpersonal contexts of negotiating care in home care nurse-patient interactions. Qual Health Res 12:1033–1057
Sumner J (2001) Caring in nursing: a different interpretation. J Adv Nurs 35:926–932
Tacke D (1999) Pflege von Menschen mit Aphasie – Eine Literaturstudie. Pflege 12:95–100
Tuckett AG (2005) The care encounter: pondering caring, honest communication and control. Int J Nurs Pract 11:77–84
Tuckett AG (2007) Stepping across the line: information sharing, truth telling, and the role of the personal carer in the Australian nursing home. Qual Health Res 17:489–500
Turnock C (1991) Communicating with patients in ICU. Nurs Stand 5:38–40
Usher K, Monkley D (2001) Effective communication in an intensive care setting: nurses’ stories. Contemp Nurse 10:91–101
van Maanen H (2002) Die Entwicklung einer Pflegefachsprache aus einer pflegewissenschaftlichen Perspektive: Das Warum und Wozu. Pflege 15:198–207
Vivian BG, Wilcox JR (2000) Compliance communication in home health care: a mutually reciprocal process. Qual Health Res 10:103–116
Walther S (2003) Sprache und Kommunikation in der Pflege. Forschungsarbeiten und Publikationen zur mündlichen und schriftlichen Kommunikation in der Pflege: Eine kommentierte Bibliographie. Gilles und Francke, Duisburg
Watson J (2005) Commentary on Shattell M (2004) Nurse-patient interaction: a review of the literature. Journal of Clinical Nursing 13:714–722 J Clin Nurs 14:530–532
Westin L, Danielson E (2007) Encounters in Swedish nursing homes: a hermeneutic study of residents’ experiences. J Adv Nurs 60:172–180
Wikström BM (2003) Health professionals’ experience of paintings as a conversation instrument: a communication strategy at a nursing home in Sweden. Appl Nurs Res 16:184–188
Williams A (2001) A literature review on the concept of intimacy in nursing. J Adv Nurs 33:660–667
Williams CA, Gossett MT (2001) Nursing communication – advocacy for the patient or physician? Clin Nurs Res 10:332–340
Williams KN, Ilten TB, Bower H (2005a) Meeting communication needs: topics of talk in the nursing home. J Psychosoc Nurs Ment Health Serv 43:38–45
Williams K, Kemper S, Hummert ML (2005b) Enhancing communication with older adults: overcoming elderspeak. J Psychosoc Nurs Ment Health Serv 43:12–16
Acknowledgements
This project was supported by the German Research Foundation (Ref.: BE 1153/2-1).
Conflict of interest
The authors disclose any relevant associations that might pose a conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Fleischer, S., Berg, A., Zimmermann, M. et al. Nurse-patient interaction and communication: A systematic literature review. J Public Health 17, 339–353 (2009). https://doi.org/10.1007/s10389-008-0238-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10389-008-0238-1