Abstract
Background
For prevention of surgical site infections, the current guidelines of Center of Disease Control recommend the maintenance of therapeutic levels of prophylactic antimicrobial agents throughout operations and, at most, for a few hours after incision closure. However, in literature supporting these recommendations, most reports have described combinations of various types of surgical procedures. Consequently, the optimal duration of prophylactic antimicrobial administration in esophagectomy with three-field lymph node dissection has not been fully addressed.
Methods
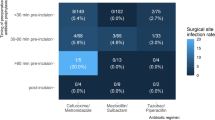
We randomly assigned 257 patients with esophageal cancer who underwent esophagectomy with three-field lymph node dissection into two groups and analyzed the incidences of surgical site and remote infections. Antimicrobial administration began 30 min before the skin incision was made and repeated every 3 h during the procedure in the short-course administration group, whereas additional administration was postoperatively continued the day after operation in the prolonged administration group.
Results
Among the 128/129 patients in the short-course/prolonged administration group, surgical site infections occurred in 26.5 %/24.0 % (p = 0.64), anastomotic leakage in 11.7 %/15.5 % (p = 0.37), and incisional surgical site infections in 14.8 %/8.5 % patients, respectively (p = 0.11). Remote infections occurred in 11.7 %/11.6 % (p = 0.86) patients, respectively, and the median postoperative hospital stay was 14 days (p = 0.86) in both groups.
Conclusions
In esophagectomy with three-field lymph node dissection, short-course antimicrobial administration was sufficient for the prevention of postoperative infectious events.

Similar content being viewed by others
References
Stone HH, Hooper CA, Kolb LD, Geheber CE, Dawkins EJ. Antibiotic prophylaxis in gastric, biliary and colonic surgery. Ann Surg. 1976;184:443–52.
Lewis RT, Allan CM, Goodall RG, Marien B, Park M, Lloyd-Smith W, Wiegand FM. Cefamandole in gastroduodenal surgery: a controlled, prospective, randomized, double-blind study. Can J Surg. 1982;25:561–3.
Nichols RL, Webb WR, Jones JW, Smith JW, LoCicero J 3rd. Efficacy of antibiotic prophylaxis in high risk gastroduodenal operations. Am J Surg. 1982;143:94–8.
Mangram AJ, Horan TC, Pearson ML, Silver LC, Jarvis WR. Guideline for prevention of surgical site infection, centers for disease control and prevention (CDC) Hospital Infection Control Practices Advisory Committee. Am J Infect Control. 1999;1999(27):97–132.
Bratzler DW, Houck PM. Antimicrobial prophylaxis for surgery: an advisory statement from the National Surgical Infection Prevention Project. Clin Infect Dis. 2004;38:1706–15.
Müller JM, Erasmi M, Stelzner M, Zieren U, Pichlmaier H. Surgical therapy of oesophageal carcinoma. Br J Surg. 1990;77:845–57.
Fujita T, Daiko H. Early enteral nutrition reduces the rate of life-threatening complications after thoracic esophagectomy in patients with esophageal cancer. Eur Surg Res. 2012;48:79–84.
Uemura Y, Ishida Y, Suzuki Y, Yanaga K. Impact of mupirocin for radical esophagectomy. J Infect Chemother. 2006;12:257–63.
Daiko H, Nishimura M. A pilot study of the technical and oncologic feasibility of thoracoscopic esophagectomy with extended lymph node dissection in the prone position for clinical stage I thoracic esophageal carcinoma. Surg Endosc. 2012;26:673–80.
Classen DC, Evans RS, Pestotnik SL, Horn SD, Menlove RL, Burke JP. The timing of prophylactic administration of antibiotics and the risk of surgical-wound infection. N Engl J Med. 1992;326:281–6.
Neoral C, Horakova M, Aujesky R, Chudacek J, Hanulik V, Chroma M, Kolar M. Infectious complications after esophagectomy. Surg Infect. 2012;13:159–62.
Culver DH, Horan TC, Gaynes RP, Martone WJ, Jarvis WR, Emori TG, Banerjee SN, Edwards JR. Surgical wound infection rates by wound class, operative procedure, and patient risk index. National Nosocomial Infections Surveillance Systems. Am J Med. 1991;91:152S–7S.
Nichols RL, Smith JW, Muzik AC, Love EJ, McSwain NE, Timberlake G, Flint LM. Prevention antibiotic use in traumatic thoracic injuries requiring closed tube thoracostomy. Chest. 1994;106:1493–8.
Uchiyama K, Takifuji K, Tani M, Ueno M, Kawai M, Ozawa S, Yamaue H. Prevention of postoperative infections by administration of antimicrobial agents immediately before surgery for patients with gastrointestinal cancers. Hepatogastroenterology. 2007;54:1487–93.
Zhang CD, Zeng YJ, Li Z, Chen J, Li HW, Zhang JK, Dai DQ. Extended antimicrobial prophylaxis after gastric cancer surgery: a systematic review and meta-analysis. World J Gastroenterol. 2013;19:2104–9.
Acknowledgments
We greatly appreciate the critical discussion of our manuscript provided by members of the Division of Esophageal Surgery. We also appreciate the review and discussion of the study provided by members of the Division of Gastrointestinal Oncology.
Ethical Statement
Our work conforms to the guidelines set forth in the Helsinki Declaration of 1975, as revised in 2000, concerning Human and Animal Rights, and that we followed the policy concerning Informed Consent.
Conflict of Interest
Takeo Fujita and Hiroyuki Daiko declare that they have no conflict of interest.
Human rights statement and informed consent
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation and with the Helsinki Declaration of 1964 and later versions. Informed consent or substitute for it was obtained from all patients for being included in the study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Fujita, T., Daiko, H. Optimal duration of prophylactic antimicrobial administration and risk of postoperative infectious events in thoracic esophagectomy with three-field lymph node dissection: short-course versus prolonged antimicrobial administration. Esophagus 12, 38–43 (2015). https://doi.org/10.1007/s10388-014-0451-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10388-014-0451-7