Abstract
Purpose
Lymphoproliferative disorders (LPDs) can develop in patients treated with methotrexate (MTX) and usually respond well to MTX withdrawal. Mucosa-associated lymphoid tissue (MALT) lymphoma is a relatively rare type of MTX-LPD. The development of MTX-LPD in the orbit has not been previously described. We here report a case of orbital MALT lymphoma that disappeared after MTX withdrawal in a patient treated with MTX for rheumatoid arthritis.
Case
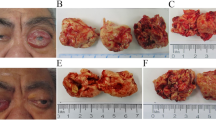
A 78-year-old woman who complained of swelling of the left upper eyelid had been treated with MTX for >8 years for rheumatoid arthritis. Slit-lamp examination revealed a temporal subconjunctival mass, salmon pink in color, in the left eye. Fundus photographs also suggested the presence of a temporal tumor in the left orbit. [18F]Fluorodeoxyglucose positron emission tomography-computed tomography revealed highly integrated lesions in the left inferotemporal orbit and a left external iliac lymph node, a left obturator lymph node, and an inguinal lymph node. Pathologic analysis of a tumor biopsy specimen showed small- and medium-sized lymphocytes positive for CD20, MIB-1, and bcl-2 and negative for CD10, CD3, bcl-1, IgG4, and EBV-ISH. On the basis of these findings, we diagnosed the tumor as MTX-induced MALT lymphoma. The subconjunctival and orbital masses disappeared gradually over 10 months after MTX withdrawal and did not recur within 2 years.
Conclusion
This case of orbital MTX-LPD suggests that the possibility of MTX-LPD should be considered even for ocular tumors in patients treated with MTX.






Similar content being viewed by others
References
Subcommittee on the Development of Guidelines for the Use of Methotrexate in the Treatment of Rheumatoid Arthritis. Medical guidelines for the use of methotrexate (MTX) in the management of rheumatoid arthritis [in Japanese, translated by author]. Tokyo, Japan: Yodosha; 2011.
Ellman MH, Hurwitz H, Thomas C, Kozloff M. Lymphoma developing in a patient with rheumatoid arthritis taking low dose weekly methotrexate. J Rheumatol. 1991;18:1741–3.
Jaffe ES, Harris NL, Stein H, Vardiman JW, editors. World Health Organization Classification of tumours: pathology & genetics of tumours of haematopoietic and lymphoid tissues. Paris: IARC Press; 2001.
Huwait H, Wang B, Shustik C, Michel RP. Composite cutaneous lymphoma in a patient with rheumatoid arthritis treated with methotrexate. Am J Dermatopathol. 2010;32:65–70.
Ichikawa A, Arakawa F, Kiyasu J, Sato K, Miyoshi H, Niino D, et al. Methotrexate/iatrogenic lymphoproliferative disorders in rheumatoid arthritis: histology, Epstein-Barr virus, and clonality are important predictors of disease progression and regression. Eur J Haematol. 2013;91:20–8.
Kikuchi K, Ishige T, Ide F, Ito Y, Saito I, Hoshino M, et al. Overexpression of activation-induced cytidine deaminase in MTX- and age-related Epstein-Barr virus-associated B-cell lymphoproliferative disorders of the head and neck. J Oncol. 2015;. doi:10.1155/2015/605750.
Felcht M, Booken N, Stroebel P, Goerdt S, Klemke CD. The value of molecular diagnostics in primary cutaneous B-cell lymphomas in the context of clinical findings, histology, and immunohistochemistry. J Am Acad Dermatol. 2011;64:135–43, 143.e1–4.
Goto H. Diagnosis and treatment of malignant ocular tumor. J Tokyo Med Univ. 2007;65:350–8.
Sumi T. Methotrexate (MTX)-associated lymphoproliferative disorders. J Otolaryngol Jpn. 2013;116:734–5.
Wolfe F, Michaud K. Lymphoma in rheumatoid arthritis: the effect of methotrexate and anti-tumor necrosis factor therapy in 18,572 patients. Arthritis Rheum. 2004;50:1740–51.
Kameda T, Dobashi H, Miyatake N, Inoo M, Onishi I, Kurata N, et al. Association of higher methotrexate dose with lymphoproliferative disease onset in rheumatoid arthritis patients. Arthritis Care Res (Hoboken). 2014;66:1302–9.
Salloum E, Cooper DL, Howe G, Lacy J, Tallini G, Crouch J, et al. Spontaneous regression of lymphoproliferative disorders in patients treated with methotrexate for rheumatoid arthritis and other rheumatic diseases. J Clin Oncol. 1996;14:1943–9.
Hoshida Y, Xu JX, Fujita S, Nakamichi I, Ikeda J, Tomita Y, et al. Lymphoproliferative disorders in rheumatoid arthritis: clinicopathological analysis of 76 cases in relation to methotrexate medication. J Rheumatol. 2007;34:322–31.
Ishitsuka K, Tamura K. Human T-cell leukaemia virus type I and adult T-cell leukaemia-lymphoma. Lancet Oncol. 2014;15:e517–26.
Fischbach W. Gastric MALT lymphoma: update on diagnosis and treatment. Best Practice Res Clin Gastroenterol. 2014;28:1069–77.
Verma V, Shen D, Sieving PC, Chan CC. The role of infectious agents in the etiology of ocular adnexal neoplasia. Surv Ophthalmol. 2008;53:312–31.
Suzuki Y, Tanaka C, Ozaki S, Hotta T. The lymphoproliferative disorder caused by methotrexate (MTX). Rheumatology. 2002;28:498–506.
Harada K, Murakami N, Kitaguchi M, Sekii S, Takahashi K, Yoshio K, et al. Localized ocular adnexal mucosa-associated lymphoid tissue lymphoma treated with radiation therapy: a long-term outcome in 86 patients with 104 treated eyes. Int J Radiat Oncol Biol Phys. 2014;88:650–4.
Swerdlow S, Campo E, Harris NL, Jaffe ES, Pileri SA, Stein H, editors. WHO classification of tumours of haematopoietic and lymphoid tissues. Paris: IARC Press; 2008.
Matsuo T, Ichimura K, Yoshino T. Spontaneous regression of bilateral conjunctival extranodal marginal zone B-cell lymphoma of mucosa-associated lymphoid tissue. J Clin Exp Hematol. 2007;47:79–81.
Kase S, Yamamoto T, Ishijima K, Noda M, Ishida S. Spontaneous regression of IgG4-related dacryoadenitis. Mod Rheumatol. 2013;23:1018–21.
Mariette X, Cazals-Hatem D, Warszawki J, Liote F, Balandraud N, Sibilia J. Lymphomas in rheumatoid arthritis patients treated with methotrexate: a 3-year prospective study in France. Blood. 2002;99:3909–15.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
Y. Kobayashi, None; K. Kimura, None; Y. Fujitsu, None; K. Shinkawa, None; H. Muta, None; K. Sonoda, None.
About this article
Cite this article
Kobayashi, Y., Kimura, K., Fujitsu, Y. et al. Methotrexate-associated orbital lymphoproliferative disorder in a patient with rheumatoid arthritis: a case report. Jpn J Ophthalmol 60, 212–218 (2016). https://doi.org/10.1007/s10384-016-0439-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10384-016-0439-z