Abstract
Purpose
We previously reported that analysis of histologically normal intestinal epithelium for spectral slope, a marker for aberrations in nanoscale tissue architecture, had outstanding accuracy in identifying field carcinogenesis in preclinical colorectal cancer models. In this study, we assessed the translatability of spectral slope analysis to human colorectal cancer screening.
Methods
Subjects (n = 127) undergoing colonoscopy had spectral slope determined from two endoscopically normal midtransverse colonic biopsies using four-dimensional elastic light-scattering fingerprinting and correlated with clinical findings.
Results
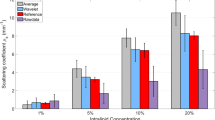
Four-dimensional elastic light-scattering fingerprinting analysis showed the submicron particles size progressively shifted toward larger sizes in subjects harboring neoplasia. There was a corresponding decrease in spectral slope values from the endoscopically normal mucosa in subjects harboring adenomas (n = 41) and advanced adenomas (n = 10), compared to neoplasia-free subjects (P ≤ 0.00001). These factors did not appear to be confounded by either age or adenoma location. For detecting advanced adenomas, spectral slope had a negative and positive predictive value of 95 percent and 50 percent respectively.
Conclusions
We demonstrate, for the first time, that spectral slope in “normal” mucosa can accurately risk-stratify patients for colonic neoplasia. This proof of concept study serves to underscore the promise of four-dimensional elastic light-scattering fingerprinting analysis for colorectal cancer screening.




Similar content being viewed by others
References
Jemal A, Siegel R, Ward E, Murray T, Xu J, Thun MJ. Cancer statistics, 2007. CA Cancer J Clin 2007;57:43–66.
Winawer S, Fletcher R, Rex D, et al. Colorectal cancer screening and surveillance: clinical guidelines and rationale. Update based on new evidence. Gastroenterology 2003;124:544–60.
Braakhuis BJ, Tabor MP, Kummer JA, Leemans CR, Brakenhoff RH. A genetic explanation of Slaughter's concept of field cancerization: evidence and clinical implications. Cancer Res 2003;63:1727–30.
Chen L, Hao C, Chiu Y, et al. Alteration of gene expression in normal-appearing colon mucosa of APCmin mice and human cancer patients. Cancer Res 2004;64:3694–700.
Imperiale TF, Wagner DR, Lin CY, Larkin GN, Rogge JD, Ransohoff DF. Risk of advanced proximal neoplasms in asymptomatic adults according to the distal colorectal findings. N Engl J Med 2000;343:169–74.
Schoenfeld P, Shad J, Ormseth E, et al. Military Colorectal Cancer Screening Trials Group. Predictive value of diminutive colonic adenoma trial: the PREDICT trial. Clin Gastroenterol Hepatol 2003;1:195–201.
Regueiro CR. AGA Future Trends Committee report: Colorectal cancer: a qualitative review of emerging screening and diagnostic technologies. Gastroenterology 2005;129:1083–103.
Backman V, Wallace MB, Perelman LT, et al. Detection of preinvasive cancer cells. Nature 2000;406:35–6.
Backman V, Gopal V, Kalashnikov M, et al. Measuring cellular structure at submicrometer scale with light scattering spectroscopy. EEE J Sel Top Quantum Electron 2001;7:887–93.
Roy HK, Liu Y, Wali RK, et al. Four-dimensional elastic light-scattering fingerprints as preneoplastic markers in the rat model of colon carcinogenesis. Gastroenterology 2004;126:1071–81, 948.
Roy HK, Iversen P, Hart J, et al. Down-regulation of SNAIL suppresses MIN mouse tumorigenesis: modulation of apoptosis, proliferation, and fractal dimension. Mol Cancer Ther 2004;3:1159–65.
Roy HK, Kim YL, Wali RK, et al. Spectral markers in preneoplastic intestinal mucosa: an accurate predictor of tumor risk in the MIN mouse. Cancer Epidemiol Biomarkers Prev 2005;14:1639–45.
van Rijn JC, Reitsma JB, Stoker J, Bossuyt PM, van Deventer SJ, Dekker E. Polyp miss rate determined by tandem colonoscopy: a systematic review. Am J Gastroenterol 2006;101:343–50.
Takayama T, Katsuki S, Takahashi Y, et al. Aberrant crypt foci of the colon as precursors of adenoma and cancer. N Engl J Med 1998;339:1277–84.
Bernstein C, Bernstein H, Garewal H, et al. A bile acid-induced apoptosis assay for colon cancer risk and associated quality control studies. Cancer Res 1999;59:2353–7.
Anti M, Marra G, Armelao F, et al. Rectal epithelial cell proliferation patterns as predictors of adenomatous colorectal polyp recurrence. Gut 1993;34:525–30.
Cui H, Cruz-Correa M, Giardiello FM, et al. Loss of IGF2 imprinting: a potential marker of colorectal cancer risk. Science 2003;299:1753–5.
Zisman A, Nickolov A, Brand R, Gorchow A, Roy H. Associations between the age at diagnosis and location of colorectal cancer and the use of alcohol and tobacco: implications for screening. Arch Intern Med 2006;166:629–34.
Polley A, Mulholland F, Pin C, et al. Proteomic analysis reveals field-wide changes in protein expression in the morphologically normal mucosa of patients with colorectal neoplasia. Cancer Res 2006;66:6553–62.
Imperiale TF, Ransohoff DF, Itzkowitz SH, Turnbull BA, Ross ME. Fecal DNA vs. fecal occult blood for colorectal-cancer screening in an average-risk population. N Engl J Med 2004;351:2704–14.
Acknowledgments
The authors thank Drs. Eric Elton, Jonathan Horwitz, Mick Meiselman, Yolandra Johnson, Sonali Master, and Eric Cohen for their assistance in patient recruitment and Ms. Beth Parker for assistance.
Author information
Authors and Affiliations
Corresponding author
Additional information
Drs. Roy, Goldberg, and Backman are cofounders and stock holders in American BioOptics.
This work was supported by research grants from the National Institutes of Health (U01CA111257, R01CA112315, R01CA128641, R01CA109861, R42CA130508 and R01EB003682), National Science Foundation (CBET-0733868), and Coulter Foundation.
Read meeting of The American Society of Colon and Rectal Surgeons, Seattle, Washington, June 3 to 7, 2006.
About this article
Cite this article
Roy, H.K., Turzhitsky, V., Kim, Y.L. et al. Spectral Slope from the Endoscopically-Normal Mucosa Predicts Concurrent Colonic Neoplasia: A Pilot Ex-Vivo Clinical Study. Dis Colon Rectum 51, 1381–1386 (2008). https://doi.org/10.1007/s10350-008-9384-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10350-008-9384-3