Abstract
Purpose
Laparoscopic rectopexy has become one of the most advocated treatments for full-thickness rectal prolapse, offering good functional results compared with open surgery and resulting in less postoperative pain and faster convalescence. However, laparoscopic rectopexy can be technically demanding. Once having mastered dexterity, with robotic assistance, laparoscopic rectopexy can be performed faster. Moreover, it shortens the learning curve in simple laparoscopic tasks. This may lead to faster and safer laparoscopic surgery. Robot-assisted rectopexy has been proven safe and feasible; however, until now, no study has been performed comparing costs and time consumption in conventional laparoscopic rectopexy vs. robot-assisted rectopexy.
Methods
Our first 14 cases of robot-assisted laparoscopic rectopexy were reviewed and compared with 19 patients who underwent conventional laparoscopic rectopexy in the same period.
Results
Robot-assisted laparoscopic rectopexy did not show more complications. However, the average operating time was 39 minutes longer, and costs were -57.29 (or: $745.09) higher.
Conclusion
Robot-assisted laparoscopic rectopexy is a safe and feasible procedure but results in increased time and higher costs than conventional laparoscopy.
Similar content being viewed by others
Since Edmond Delorme first described a perineal mucosal-stripping procedure to treat rectal procidentia in 1899,1 controversy exists regarding the preferred surgical technique for the treatment of rectal prolapse. Not a single procedure has been considered a standard, because all treatment modalities show failures. In all studies, patient groups are heterogeneous and therefore incomparable, and, often, long-term recurrence has not been observed in adequate numbers. However, most authors agree that perineal procedures might be less invasive than abdominal procedures, offering successful treatment in frail elderly patients with extensive comorbidity.2-5
A transabdominal procedure is generally considered more effective in healthy patients6-8 and can be combined with uteropexy or colpopexy when necessary. Laparoscopic repair9-11 seems as effective as open surgery and results in faster convalescence and less postoperative pain.12-15
Therefore, this approach has been advocated by many authors as probably the preferred technique. Whether standard sigmoid resection should be performed to prevent constipation remains debatable.16-20 Division of the lateral ligaments should be avoided to prevent rectal dysfunction.21 Whether anterior rectopexy leads to better functional results than posterior rectopexy, and mesh repair results in better effect and fewer complications than suture repair, remains unclear.22
Laparoscopic rectopexy, irrespective of the technique used, can be technically demanding. Robotic assistance in laparoscopic surgery may shorten the operating time as well as the learning curve in simple laparoscopic tasks.23-26 Robot-assisted rectopexy has been proven safe and feasible,27,28 but until now, no study has been performed comparing costs and time consumption in conventional laparoscopic rectopexy vs. robot-assisted rectopexy.
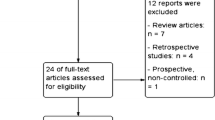
Patients and Methods
From January 1, 2004 through May 1, 2006, 33 patients underwent laparoscopic rectopexy for rectal procidentia. They were nonrandomly assigned to conventional (CR) or robot-assisted (RR) laparoscopic surgery, using the four-armed da Vinci® surgical system if available. The indication for rectopexy was full-thickness rectal prolapse in all cases. Exclusion criteria were: younger than aged 18 years, patients unfit to undergo laparoscopic surgery, or “hostile abdomen,-meaning patients with a medical history of extensive abdominal surgery, probably with multiple adhesions, which make them less accessible for laparoscopic surgery. Previous simple abdominal surgery was not considered a contraindication, nor was previous antiprolapse surgery. CR or RR was performed by the same team.
Procedure
In the first 11 cases, a laparoscopic Wells29 posterior sling procedure was performed. Since July 1, 2004, general policy in our department shifted toward performing a laparoscopic D’Hoore procedure10 to minimize postoperative constipation. This change in technique was used irrespectively of the use of CR vs. RR. In CR, a five-trocar technique was used. The rectosigmoid junction was retracted to the left and a peritoneal incision was made over the right side of the sacral promontory and extended in an inverted J-form along the rectum. The right hypogastric nerve was left undamaged while opening Denonvillier’s fascia in male patients or the rectovaginal septum in females. No lateral mobilization or lateral dissection was performed to maximally preserve rectal innervation. In Wells-procedure, a piece of polypropylene mesh (Dacron®) vascular prosthesis is stapled to the sacral promontory with the help of the Endopath® EMS (Ethicon Endo-Surgery, Norderstedt, Germany) and wrapped at two sides around the lifted rectum where it is fixed on the anterolateral side, using GORE-TEX® sutures. In females with coexisting vaginal vault prolapse, the top of the vagina is fixed to the Dacron mesh and the peritoneum is closed over the mesh. In D’Hoore’s rectopexy, a 3-cm ×-7-cm strip of Dacron® is fixed to the sacral promontory by using an endofascial stapler device (Endopath® EMS) and then sutured to the ventral aspect of the distal rectum. The posterior vaginal fornix is elevated and sutured to the anterior aspect of the mesh, closing the rectovaginal septum. The peritoneum is closed over the mesh.
In RR, the same procedure is performed by using the four-armed da Vinci® surgical system (Intuitive Surgical Inc., Sunnyvale, CA). The patient is positioned in a French steep Trendelenburg position. The four-armed robotic cart is positioned between the legs of the patient. Port placement is similar to that in CR, using a 12-mm robotic camera port in the infra-umbilical position and three 7-mm robotic ports controlled by the surgeon from behind the console. Another 12-mm trocar is placed suprapubically to allow the assistant to retract the bladder and use the EMS stapler to fix the mesh to the promontory. Dissection and fixation is done as described in CR.
Measurements
Discharge criteria were identical for all patients. Patients resumed oral feeding within 24 hours if tolerated. They were discharged two days after surgery if sufficiently recovered and normal defecation had occurred. Laxatives were given when indicated. Accessory laboratory and radiologic examinations were only performed on indication. Primary end points were procedure time, hospital stay, and costs. Costs were calculated by using costs for hospital admission and treatment, material costs during surgery, salary costs (wages per hour for attending surgeons, anesthesiologists, residents and nurses, multiplied by the time spent in the operating room). Secondary end points were morbidity and mortality.
Statistical analysis was performed by using SPSS® 12 (SPSS Inc., Chicago, IL). Pearson chi-squared test was used to compare nominal data between groups. A Mann-Whitney U nonparametric test for two independent samples was used to compare age, time, and costs. P ≤-.05 was defined as being statistically significant.
Results
Preoperative Characteristics
Thirty-three patients (22 females) with symptomatic full-thickness rectal prolapse were nonrandomly assigned to undergo CR or RR. In the CR group, 19 patients were included; 7 underwent a Wells-procedure and 12 a D’Hoore’s rectopexy. In the RR group, a Wells-rectopexy was performed in four patients and a D’Hoore’s procedure in ten patients. Preoperative characteristics are listed in Tables 1 and 2. In the D’Hoore’s rectopexy group, eight patients had undergone previous uterus extirpation vs. none in the Wells rectopexy group.
Operative and Postoperative Characteristics
Preoperative and postoperative complication rates were similar in the CR and RR groups, and also in the D’Hoore’s and Wells rectopexy group. However, average operation time is longer in robotic-assisted rectopexy (152 vs. 113 minutes) compared with conventional laparoscopy. D’Hoore’s rectopexy is faster than Wells-procedure (122 vs. 162 minutes). When comparing the costs of the procedures, it is clear that RR is more expensive than CR, both in salary and robot-associated costs, leading to higher total costs (-3,672.84 vs. -3,115.55, or $4,910.55 vs. $4,165.46) compared with CR (P--.012). When comparing Wells-procedure vs. D’Hoore’s rectopexy, the salary costs are higher in Wells-procedure (-555.12 vs. -417.27, or $742.19 vs. $557.89; P--.039), but the total costs remain unchanged (-3,446.61 vs. -3,431.32, or $4,608.08 vs. $4,587.64; P--.62).
Postoperative constipation was defined as the inability to pass stool more than five days after surgery. Postoperative incontinence was measured using the Parks-Browning classification for fecal incontinence. Grade 1 is full continence. Grade 2 is incontinence to flatus, Grade 3 is incontinence to liquid stool, and Grade 4 is incontinence to solid stool. Operative and postoperative characteristics are shown in Tables 1 and 2.
Discussion
Robotic assistance in advanced laparoscopy leads to high-definition stereoscopic vision and intuitive tremor-filtrated movement of instruments, potentially attributing to safety and feasibility. In this study, we compared conventional laparoscopic vs. robot-assisted rectopexy. Statistical analysis showed that preoperative characteristics, admissions, and complication rates were similar between both groups, suggesting robot-assisted laparoscopic rectopexy is safe and feasible. However, the group size is limited, making it impossible to show a statistically significant decrease in complication rate. A follow-up study assessing functional results and complications is being performed, and results are expected soon. If robotic assistance does lead to a lower complication rate or better functional results, this could result in higher cost-effectiveness.
Robotic assistance in laparoscopic rectopexy results in a significantly increased operating time of 39 minutes. Increased time consumption in robot-assisted advanced laparoscopy was described previously30-32 in contrast to the beneficial effect of robotic assistance on time consumption in the performance of laparoscopic excercises.23,24,26 Probably, part of this increase in time is caused by the relatively laborious effort to change robotic instruments and to the limited experience with robotic surgery at this moment.
The use of robotic assistance leads to increased salary costs (caused by increased time consumption) and increased material costs, which results in a total increase of -57.29 (or $745.09) compared with CR. Along with the increasing experience with robotic surgery, the time needed to perform the operation is expected to decrease, resulting in diminished salary costs. Whether material costs will decrease in time remains unclear.
The Wells-procedure seemed more time consuming than the slightly less complex modified-D’Hoore’s rectopexy. However, because the Wells-rectopexy was performed before July 1, 2004, whereas D’Hoore’s rectopexy was performed after this date, the decreased operating time also might partly be a result of the proficiency curve. We did not find a statistically significant decreased number of patients with postoperative constipation performing D’Hoore’s rectopexy compared with Wells-rectopexy, as might have been expected.22
Conclusions
Robotic assistance in laparoscopic rectopexy is a safe and feasible procedure but leads to a longer operating time and higher costs compared with conventional laparoscopy. Although robotic assistance has excellent vision and intuitive manipulation of instruments during surgery, this study did not show objective arguments to support the routine use of robotic assistance at this time. A follow-up study that assesses functional results and recurrences after robot-assisted vs. conventional laparoscopic rectopexy is being conducted, and results are expected in a few months. Further prospective comparative trials are needed to assess the role of robotic assistance in laparoscopic surgery.
References
Rose SM. Classic articles in colonic and rectal surgery. Edmond Delorme 1847-929. Dis Colon Rectum 1985;28:544-3.
Williams JG, Rothenberger DA, Madoff RD, Goldberg SM. Treatment of rectal prolapse in the elderly by perineal rectosigmoidectomy. Dis Colon Rectum 1992;35:830-.
Lasheen AE, Khalifa S, El Askry SM, Elzeftawy AA. Closed rectopexy with transanal resection for complete rectal prolapse in adults. J Gastrointest Surg 2005;9:980-.
Watkins BP, Landercasper J, Belzer GE, et al. Long-term follow-up of the modified Delorme procedure for rectal prolapse. Arch Surg 2003;138:498–502.
Altemeier WA, Giuseffi J, Hoxworth P. Treatment of extensive prolapse of the rectum in aged or debilitated patients. AMA Arch Surg 1952;65:72–80.
Chow PK, Ho YH. Abdominal resection rectopexy versus Delorme’s procedure for rectal prolapse: comparison of clinical and physiological outcomes. Int J Colorectal Dis 1996;11:201-
Penninckx F, D’Hoore A, Sohier S, Kerremans R. Abdominal resection rectopexy versus Delorme’s procedure for rectal prolapse: a predictable outcome. Int J Colorectal Dis 1997;12:49–50
Steele SR, Goetz LH, Minami S, Madoff RD, Mellgren AF, Parker SC. Management of recurrent rectal prolapse: surgical approach influences outcome. Dis Colon Rectum 2006;49:440-.
Zittel TT, K Manncke K, Haug S, et al. Functional results after laparoscopic rectopexy for rectal prolapse. J Gastrointest Surg 2000;4:632-1.
D’Hoore A, Cadoni R, Penninckx F. Long-term outcome of laparoscopic ventral rectopexy for total rectal prolapse. Br J Surg 2004;91:1500-.
Rose J, Schneider C, Scheidbach H, et al. Laparoscopic treatment of rectal prolapse: experience gained in a prospective multicentre trial. Langenbeck’s Arch Surg 002;387:130-.
Solomon MJ, Young CJ, Eyers AA, Roberts RA. Randomized clinical trial of laparoscopic versus open abdominal rectopexy for rectal prolapse. Br J Surg 2002;89:35-
Kairaluoma MV, Viljakka MT, Kellokumpu IH. Open vs. laparoscopic surgery for rectal prolapse: a case-controlled study assessing short-term outcome. Dis Colon Rectum 2003;46:353-0
Purkayastha S, Tekkis P, Athanasiou T, et al. A comparison of open vs. laparoscopic abdominal rectopexy for full-thickness rectal prolapse: a meta-analysis. Dis Colon Rectum 2005;48:1930-0.
Kariv Y, Delaney CP, Casillas S, et al. Long-term outcome after laparoscopic and open surgery for rectal prolapse: a case-controlled study. Surg Endosc 2006;20:35–42.
Benoist S, Taffinder N, Gould S, Chang A, Darzi A. Functional results two years after laparoscopic rectopexy. Am J Surg 2001;182:168-3
Heah SM, Hartley JE, Hurley J, Duthie GS, Monson JR. Laparoscopic suture rectopexy without resection is effective treatment for full-thickness rectal prolapse. Dis Colon Rectum 2000;43:638-3.
Lechaux JP, Atienza P, Goasguen N, Lechaux D, Bars I. Prosthetic rectopexy to the pelvic floor and sigmoidectomy for rectal prolapse. Am J Surg 2001;182:465-
Basse L, Billesbolle P, Kehlet H. Early recovery after abdominal rectopexy with multimodal rehabilitation. Dis Colon Rectum 2002;45:195-.
Ashari LH, Lumley JW, Stevenson AR, Stitz RW. Laparoscopically-assisted resection rectopexy for rectal prolapse: ten year’s experience. Dis Colon Rectum 2005;48:982-.
Scaglia M, Fasth S, Hallgren T, Nordgren S, Oresland T, Hulten L. Abdominal rectopexy for rectal prolapse. Influence of surgical technique on functional outcome. Dis Colon Rectum 1994;37:805-3.
Schiedeck TH, Schwandner O, Scheele J, Farke S, Bruch HP. Rectal prolapse: which surgical option is appropriate? Langenbecks Arch Surg 2005;390:8–14.
Yohannes P, Rotariu P, Pinto P, Smith AD, Lee BR. Comparison of robotic versus laparoscopic skills: is there a difference in the learning curve? Urology 2002;60:39–45.
Hernandez JD, Bann SD, Munz Y, et al. Qualitative and quantitative analysis of the learning curve of a simulated surgical task on the da Vinci system. Surg Endosc 2004;18:372-.
Sarle R, Tewari A, Shrivastava A, Peabody J, Menon M. Surgical robotics and laparoscopic drills. J Endourol 2004;18:63-
Heemskerk J, Zandbergen RH, Maessen JG, Greve JW, Bouvy ND. Advantages of advanced laparoscopic systems. Surg Endosc 2006;20:730-.
Munz Y, Moorthy K, Kudchadkar R, et al. Robotic assisted rectopexy. Am J Surg 2004;187:88–92.
Ayav A, Bresler L, Hubert J, Brunaud L, Boissel P. Robotic-assisted pelvic organ prolapse surgery. Surg Endosc 2005;19:1200-.
Himpens J, Cadiere GB, Bruyns J, Vertruyen M. Laparoscopic rectopexy according to Wells. Surg Endosc 1999;13:139-1.
Heemskerk J, van Dam R, van Gemert WG, et al. Robot-assisted versus conventional laparoscopic Nissen fundoplication. A comparative retrospective study on costs and time consumption. SLEPT 2007;17:1–4
Morino M, Pellegrino L, Giaccone C, Garonne C, Rebecchi F. Randomized clinical trial of robot-assisted versus laparoscopic Nissen fundoplication. Br J Surg 2006;93:553-
Morino M, Beninca G, Giraudo G, Del Genio GM, Rebecchi F, Garrone C. Robot-assisted vs. laparoscopic adrenalectomy: a prospective randomized controlled trial. Surg Endosc 2004;18:1742-
Acknowledgement
The authors thank Mrs. Karin Baeten for assistance.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Heemskerk, J., de Hoog, D.E.N.M., van Gemert, W.G. et al. Robot-Assisted vs. Conventional Laparoscopic Rectopexy for Rectal Prolapse: A Comparative Study on Costs and Time. Dis Colon Rectum 50, 1825–1830 (2007). https://doi.org/10.1007/s10350-007-9017-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10350-007-9017-2