Abstract
Purpose
Perfusion assessment by monitoring the transport of a tracer bolus depends critically on conversion of signal intensity into tracer concentration. Two main assumptions are generally applied for this conversion; (1) contrast agent relaxivity is identical in blood and tissue, (2) change in signal intensity depends only on the primary relaxation effect. The purpose of the study was to assess the validity and influence of these assumptions.
Materials and methods
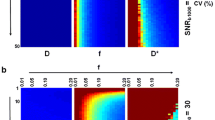
Blood and cerebral tissue relaxivities r1, r2, and r2* for gadodiamide were measured in four pigs at 1.5 T. Gadolinium concentration was determined by inductively coupled plasma atomic emission spectroscopy. Influence of the relaxivities, secondary relaxation effects and choice of singular value decomposition (SVD) regularization threshold was studied by simulations.
Results
In vivo relaxivities relative to blood concentration [in s−1 mM−1 for blood, gray matter (GM), white matter (WM)] were for r1 (2.614 ± 1.061, 0.010 ± 0.001, 0.004 ± 0.002), r2 (5.088 ± 0.952, 0.091 ± 0.008, 0.059 ± 0.014), and r2* (13.292 ± 3.928, 1.696 ± 0.157, 0.910 ± 0.139). Although substantial, by a nonparametric test for paired samples, the differences were not statistically significant. The GM to WM blood volume ratio was estimated to 2.6 ± 0.9 by r1, 1.6 ± 0.3 by r2, and 1.9 ± 0.2 by r2*. Secondary relaxation was found to reduce the tissue blood flow, as did the SVD regularization threshold.
Conclusion
Contrast agent relaxivity is not identical in blood and tissue leading to substantial errors. Further errors are introduced by secondary relaxation effects and the SVD regularization.







Similar content being viewed by others
References
Meier P, Zierler KL (1954) On the theory of the indicator-dilution method for measurement of blood flow and volume. J Appl Physiol 6:731–744
Zierler KL (1965) Equations for measuring blood flow by external monitoring of radioisotopes. Circ Res 16:309–321
Belliveau JW, Rosen BR, Kantor HL, Rzedzian RR, Kennedy DN, McKinstry RC, Vevea JM, Cohen MS, Pykett IL, Brady TJ (1990) Functional cerebral imaging by susceptibility-contrast NMR. Magn Reson Med 14:538–546
Larson KB, Perman WH, Perlmutter JS, Gado MH, Ollinger JM, Zierler K (1994) Tracer-kinetic analysis for measuring regional cerebral blood flow by dynamic nuclear magnetic resonance imaging. J Theor Biol 170:1–14
Villringer A, Rosen BR, Belliveau JW, Ackerman JL, Lauffer RB, Buxton RB, Chao YS, Wedeen VJ, Brady TJ (1988) Dynamic imaging with lanthanide chelates in normal brain: contrast due to magnetic susceptibility effects. Magn Reson Med 6:164–174
Larsson HB, Hansen AE, Berg HK, Rostrup E, Haraldseth O (2008) Dynamic contrast-enhanced quantitative perfusion measurement of the brain using T1-weighted MRI at 3T. J Magn Reson Imaging 27:754–762
Young GS, Setayesh K (2009) Spin-echo echo-planar perfusion MR imaging in the differential diagnosis of solitary enhancing brain lesions: distinguishing solitary metastases from primary glioma. AJNR Am J Neuroradiol 30:575–577
Knutsson L, Stahlberg F, Wirestam R (2010) Absolute quantification of perfusion using dynamic susceptibility contrast MRI: pitfalls and possibilities. Magn Reson Mater Phys 23:1–21
Rempp KA, Brix G, Wenz F, Becker CR, Guckel F, Lorenz WJ (1994) Quantification of regional cerebral blood flow and volume with dynamic susceptibility contrast-enhanced MR imaging. Radiology 193:637–641
Ostergaard L, Weisskoff RM, Chesler DA, Gyldensted C, Rosen BR (1996) High resolution measurement of cerebral blood flow using intravascular tracer bolus passages. Part I: mathematical approach and statistical analysis. Magn Reson Med 36:715–725
Jonsson O, Morell A, Zemgulis V, Lundstrom E, Tovedal T, Einarsson GM, Thelin S, Ahlstrom H, Bjornerud A, Lennmyr F (2011) Minimal safe arterial blood flow during selective antegrade cerebral perfusion at 20 degrees centigrade. Ann Thorac Surg 91:1198–1205
Van Wagoner M, Worah D (1993) Gadodiamide injection. First human experience with the nonionic magnetic resonance imaging enhancement agent. Invest Radiol 28(Suppl 1):S44–S48
Deichmann R, Haase A (1992) Quantification of T1 values by SNAPSHOT-FLASH NMR imaging. J Magn Reson 96:5
Kuppusamy K, Lin W, Cizek GR, Haacke EM (1996) In vivo regional cerebral blood volume: quantitative assessment with 3D T1-weighted pre- and postcontrast MR imaging. Radiology 201:106–112
Lin W, Celik A, Paczynski RP (1999) Regional cerebral blood volume: a comparison of the dynamic imaging and the steady state methods. J Magn Reson Imaging 9:44–52
Newman GC, Delucia-Deranja E, Tudorica A, Hospod FE, Patlak CS (2003) Cerebral blood volume measurements by T*2-weighted MRI and contrast infusion. Magn Reson Med 50:844–855
Ito H, Kanno I, Kato C, Sasaki T, Ishii K, Ouchi Y, Iida A, Okazawa H, Hayashida K, Tsuyuguchi N, Kuwabara Y, Senda M (2004) Database of normal human cerebral blood flow, cerebral blood volume, cerebral oxygen extraction fraction and cerebral metabolic rate of oxygen measured by positron emission tomography with 15O-labelled carbon dioxide or water, carbon monoxide and oxygen: a multicentre study in Japan. Eur J Nucl Med Mol Imaging 31:635–643
Morell A, Ahlstrom H, Schoenberg SO, Abildgaard A, Bock M, Bjornerud A (2008) Quantitative renal cortical perfusion in human subjects with magnetic resonance imaging using iron-oxide nanoparticles: influence of T1 shortening. Acta Radiol 49:955–962
Bjornerud A, Emblem KE (2010) A fully automated method for quantitative cerebral hemodynamic analysis using DSC–MRI. J Cereb Blood Flow Metab 30:1066–1078
Calamante F, Connelly A, van Osch MJ (2009) Nonlinear DeltaR*2 effects in perfusion quantification using bolus-tracking MRI. Magn Reson Med 61:486–492
Calamante F, Gadian DG, Connelly A (2000) Delay and dispersion effects in dynamic susceptibility contrast MRI: simulations using singular value decomposition. Magn Reson Med 44:466–473
Rohrer M, Bauer H, Mintorovitch J, Requardt M, Weinmann HJ (2005) Comparison of magnetic properties of MRI contrast media solutions at different magnetic field strengths. Invest Radiol 40:715–724
Knutsson L, Stahlberg F, Wirestam R (2004) Aspects on the accuracy of cerebral perfusion parameters obtained by dynamic susceptibility contrast MRI: a simulation study. Magn Reson Imaging 22:789–798
Liu HL, Pu Y, Liu Y, Nickerson L, Andrews T, Fox PT, Gao JH (1999) Cerebral blood flow measurement by dynamic contrast MRI using singular value decomposition with an adaptive threshold. Magn Reson Med 42:167–172
Murase K, Shinohara M, Yamazaki Y (2001) Accuracy of deconvolution analysis based on singular value decomposition for quantification of cerebral blood flow using dynamic susceptibility contrast-enhanced magnetic resonance imaging. Phys Med Biol 46:3147–3159
Calamante F, Vonken EJ, van Osch MJ (2007) Contrast agent concentration measurements affecting quantification of bolus-tracking perfusion MRI. Magn Reson Med 58:544–553
Knutsson L, Stahlberg F, Wirestam R, van Osch MJ (2013) Effects of blood DeltaR2* non-linearity on absolute perfusion quantification using DSC–MRI: comparison with Xe-133 SPECT. Magn Reson Imaging 31:651–655
van Osch MJ, Vonken EJ, Viergever MA, van der Grond J, Bakker CJ (2003) Measuring the arterial input function with gradient echo sequences. Magn Reson Med 49:1067–1076
Kiselev VG (2001) On the theoretical basis of perfusion measurements by dynamic susceptibility contrast MRI. Magn Reson Med 46:1113–1122
Simonsen CZ, Ostergaard L, Smith DF, Vestergaard-Poulsen P, Gyldensted C (2000) Comparison of gradient- and spin-echo imaging: CBF, CBV, and MTT measurements by bolus tracking. J Magn Reson Imaging 12:411–416
Boxerman JL, Hamberg LM, Rosen BR, Weisskoff RM (1995) MR contrast due to intravascular magnetic susceptibility perturbations. Magn Reson Med 34:555–566
Bjornerud A, Johansson LO, Ahlstrom HK (2002) Renal T(*)(2) perfusion using an iron oxide nanoparticle contrast agent–influence of T(1) relaxation on the first-pass response. Magn Reson Med 47:298–304
Kjolby BF, Ostergaard L, Kiselev VG (2006) Theoretical model of intravascular paramagnetic tracers effect on tissue relaxation. Magn Reson Med 56:187–197
Newman GC, Hospod FE, Patlak CS, Fain SE, Pulfer KA, Cook TD, O’Sullivan F (2006) Experimental estimates of the constants relating signal change to contrast concentration for cerebral blood volume by T2* MRI. J Cereb Blood Flow Metab 26:760–770
Johnson KM, Tao JZ, Kennan RP, Gore JC (2000) Intravascular susceptibility agent effects on tissue transverse relaxation rates in vivo. Magn Reson Med 44:909–914
Morkenborg J, Taagehoj JF, Vaever PN, Frokiaer J, Djurhuus JC, Stodkilde-Jorgensen H (1998) In vivo measurement of T1 and T2 relaxivity in the kidney cortex of the pig-based on a two-compartment steady-state model. Magn Reson Imaging 16:933–942
Pedersen M, Klarhofer M, Christensen S, Ouallet JC, Ostergaard L, Dousset V, Moonen C (2004) Quantitative cerebral perfusion using the PRESTO acquisition scheme. J Magn Reson Imaging 20:930–940
Acknowledgments
This work was supported by the Swedish Research Council; grants K2013-64x-08268-26-3 and 621-2011-4423. Håkan Pettersson is acknowledged for the preparation of the figures.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Morell, A., Lennmyr, F., Jonsson, O. et al. Influence of blood/tissue differences in contrast agent relaxivity on tracer-based MR perfusion measurements. Magn Reson Mater Phy 28, 135–147 (2015). https://doi.org/10.1007/s10334-014-0452-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10334-014-0452-5