Abstract
Background
Non-motor symptoms are increasingly recognized in Parkinson disease (PD) and include physical as well as psychological symptoms. A psychological condition that has been well studied in PD is psychosis. Cardiovascular autonomic dysfunction in PD can include a reversed or loss of blood pressure (BP) circadian rhythm, referred to as nocturnal non-dipping. The aim of this study was to determine the relationship between 24 h ambulatory blood pressure measurements (ABPM), i.e., absence or presence of nocturnal dipping, and psychosis scores in PD.
Methods
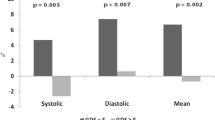
Twenty-one patiens with PD underwent 24 h ABPM using an autonomic protocol. A decrease in nocturnal mean arterial blood pressure of less than 10 % was defined as non-dipping. Patients were interviewed (including the brief psychiatric rating scale; BPRS) for the assessment of psychosis.
Results
Eleven patients were dippers and 10 were non-dippers. BPRS scores were higher in non-dippers, who, on average, met the criteria for psychosis (mean non-dipper BPRS: 34.3 ± 7.3 vs mean dipper BPRS: 27.5 ± 5.3; cutoff for “mildly ill” 31). There was a correlation between BPRS scores and non-dipping, indicating that those patients who had a blunted nocturnal fall in BP were more prone to psychotic symptoms (Pearson’s Correlation = 0.554, p = 0.009).
Conclusion
These results suggest that, among PD patients, a non-dipping circadian rhythm is associated with more severe symptoms of psychosis than is a dipping circadian rhythm. This association warrants further investigation.


Similar content being viewed by others
References
Jankovic J (2008) Parkinson’s disease: clinical features and diagnosis. JNNP 79(4):368–376
Antonini A, Barone P, Marconi R et al (2012) The progression of non-motor symptoms in Parkinson’s disease and their contribution to motor disability and quality of life. J Neurol 259(12):2621–2631
Stern MBS, Siderowf A (2011) Clinical features: motor and nonmotor. In: Schapira AH (ed) Parkinson’s Disease. Oxford University Press, New York
Hollister AS (1992) Orthostatic hypotension. Causes, evaluation, and management. West J Med 157(6):652–657
Senard JM, Chamontin B, Rascol A et al (1992) Ambulatory blood pressure in patients with Parkinson’s disease without and with orthostatic hypotension. Clin Auton Res 2(2):99–104
Pickering TG et al (2005) Recommendations for blood pressure measurement in humans and experimental animals. Part 1: blood pressure measurement in humans: a statement for professionals from the subcommittee of professional and public education of the American heart association council on high blood pressure research. Circulation 111(5):697–716
Foster RG (2010) A sense of time: body clocks, sleep and health. DMW 135(51–52):2601–2608
Fabbian F et al (2013) Dipper and non-dipper blood pressure 24-h patterns: circadian rhythm-dependent physiologic and pathophysiologic mechanisms. Chronobiol Int 30(1–2):17–30. doi:10.3109/07420528.2012.715872
Suh M, Barksdale DJ, Logan J (2013) Relationships among acculturative stress, sleep, and nondipping blood pressure in Korean American women. Clin Nurs Res 22(1):112–129
Mansoor GA (2002) Sleep actigraphy in hypertensive patients with the ‘non-dipper’ blood pressure profile. J Hum Hypertens 16(4):237–242
Clays E, Van Herck K, De Buyzere M et al (2012) Behavioural and psychosocial correlates of nondipping blood pressure pattern among middle-aged men and women at work. J Hum Hyperten 26(6):381–387
Hakamaki T, Rajala T, Lehtonen A (1998) Ambulatory 24-h blood pressure recordings in patients with Parkinson’s disease with or without fludrocortisone. Int J Clin Pharm Th I 36(7):367–369
Ejaz AA, Sekhon IS, Munjal S (2006) Characteristic findings on 24-h ambulatory blood pressure monitoring in a series of patients with Parkinson’s disease. Eur J Intern Med 17(6):417–420
Stuebner EVE, Low DA, Mathias CJ, Isenmann S, Haensch CA (2013) Twenty-four hour non-invasive ambulatory blood pressure and heart rate monitoring in Parkinson’s Disease. Front Neurol 4:49
Berger F (2014) Psychosis: MedlinePlus medical encyclopedia. http://www.nlm.nih.gov/medlineplus/ency/article/001553.htm. Retrieved 29 Jan 2015
Dolder CR, Furtek K, Lacro JP et al (2005) Antihypertensive medication adherence and blood pressure control in patients with psychotic disorders compared to persons without psychiatric illness. Psychosom 46(2):135–141
Galletly CA, Foley DL, Waterreus A et al (2012) Cardiometabolic risk factors in people with psychotic disorders: the second Australian national survey of psychosis. Australasian and N. Z. J Psychiatry 46(8):753–761
Poewe W (2003) Psychosis in Parkinson’s disease. Mov Disord 18(Suppl 6):S80–S87
Forsaa EB, Larsen JP, Wentzel-Larsen T (2010) A 12-year population-based study of psychosis in Parkinson disease. Arch Neurol 67(8):996–1001
Rabey JM (2009) Hallucinations and psychosis in Parkinson’s disease. Parkinsonism Relat Disord 15(Suppl 4):S105–S110
Klawans HL (1988) Psychiatric side effects during the treatment of Parkinson’s disease. J Neural Transm 27:117–122
West LJ, Janszen HH, Lester BK et al (1962) The psychosis of sleep deprivation. Ann N Y Acad Sci 13(96):66–70
Videnovic A, Golombek D (2012) Circadian and sleep disorders in Parkinson’s disease. Exp Neurol 243:45–56
Chaudhuri KR, Healy DG, Schapira AH (2006) National institute for clinical E. Non-motor symptoms of Parkinson’s disease: diagnosis and management. Lancet Neurol 5(3):235–245
Hughes AJ, Daniel SE, Kilford L et al (1992) Accuracy of clinical diagnosis of idiopathic Parkinson’s disease: a clinico-pathological study of 100 cases. JNNP 55(3):181–184
Movement disorder society task force on rating scales for Parkinson’s disease (2003) The Unified Parkinson’s disease rating scale (UPDRS): status and recommendations. Mov Disord 18(7):738–750
Goetz CG, Poewe W, Rascol O et al (2004) Movement disorder society task force report on the Hoehn and Yahr staging scale: status and recommendations. Mov Disord 19(9):1020–1028
Jenkinson C, Fitzpatrick R, Peto V et al (1997) The Parkinson’s disease questionnaire (PDQ-39): development and validation of a Parkinson’s disease summary index score. JAA 26(5):353–357
Goetz CG (2009) Scales to evaluate psychosis in Parkinson’s disease. Parkinsonism Relat Disord 15(S3):3
Leucht S, Kane JM, Kissling W et al (2005) Clinical implications of brief psychiatric rating scale scores. Br J Psychiatry 187:366–371
Kay SRF A, Opler LA (1967) The Positive and negative syndrome scale (PANNS) for schizophrenia. Schizophr Res 13(2):16
Schatz IJBR, Freeman RL, Jankovic J et al (1996) Consensus statement on the definition of orthostatic hypotension, pure autonomic failure and multiple system atrophy. Clin Auton Res 46(6):125–126
Mathias CJBR (2013) Clinical autonomic testing. In: Mathias CJBR (ed) Autonomic failure. A textbook of clinical disorders of autonomic nervous system 5. Oxford University Press, Oxford
Rogers G, Oosthuyse T (2000) A comparison of the indirect estimate of mean arterial pressure calculated by the conventional equation and calculated to compensate for a change in heart rate. Int J Sports Med 21(2):90–95
Fagard RH (2009) Dipping pattern of nocturnal blood pressure in patients with hypertension. Expert Rev Cardiovasc Ther 7(6):599–605
Tomlinson CL, Stowe R, Patel S et al (2010) Systematic review of levodopa dose equivalency reporting in Parkinson’s disease. Mov Disord 25(15):2649–2653
Cohen JW (1988) Statistical power analysis for the behavioral sciences, 2nd edn. Lawrence Erlbaum Associates, Hillsdale, NJ
Leucht S, Kane JM, Etschel E et al (2006) Linking the PANSS, BPRS, and CGI: clinical implications. ACNP 31(10):2318–2325
Rogers MW (1996) Disorders of posture, balance, and gait in Parkinson’s disease. Clin Geriatr Med 12(4):825–845
Rogers D, Lees AJ, Smith E et al (1987) Bradyphrenia in Parkinson’s disease and psychomotor retardation in depressive illness. An experimental study. Brain 110(Pt 3):761–776
Hawkes CH, Del Tredici K, Braak H (2010) A timeline for Parkinson’s disease. Parkinsonism Relat Disord 16(2):79–84
Asahina M et al (2012) Autonomic dysfunction in parkinsonian disorders: assessment and pathophysiology. J Neurol Neurosurg Psychiatry 84(6):674–680
Wulff K, Gatti S, Wettstein JG, Foster RG (2010) Sleep and circadian rhythm disruption in psychiatric and neurodegenerative disease. Nat Rev Neurosci 11(8):589–599
Goldstein DS, Pechnik S, Holmes C et al (2003) Association between supine hypertension and orthostatic hypotension in autonomic failure. Hypertension 42(2):136–142
Buysse DJ, Reynolds CF, Monk TH et al (1989) The pittsburgh sleep quality index: a new instrument for psychiatric practice and research. Psychiatry Res 28(2):193–213
Boulamery A, Simon N, Vidal J et al (2010) Effects of L-Dopa on circadian rhythms of 6-OHDA striatal lesioned rats: a radiotelemetric study. Chronobiol Int 27(2):251–264
Pritchett D, Wulff K, Oliver PL et al (2012) Evaluating the links between schizophrenia and sleep and circadian rhythm disruption. J Neural Transm 119(10):1061–1075
Dauer W, Przedborski S (2003) Parkinson’s disease: mechanisms and models. Neuron 39(6):889–909
Vernier P, Moret F, Callier S et al (2004) The degeneration of dopamine neurons in Parkinson’s disease: insights from embryology and evolution of the mesostriatocortical system. Ann N Y Acad Sci 1035:231–249
Seeman P, Weinshenker D, Quirion R et al (2005) Dopamine supersensitivity correlates with D2High states, implying many paths to psychosis. Proc Natl Acad Sci USA 102(9):3513–3518
Acknowledgments
CAH conceived the initial idea to the project, CAH, ES, DAL and CJM managed the ethics committee application, ES, EV, DAL and CAH contributed to the Conception, Organization and Execution of the Research project, ES and EV performed all testing, CAH, CJM, DAL and SI supervised the project. ES, EV, DAL and CAH contributed to the Review and Critique of the Statistical Analysis, ES drafted the original version of the manuscript, DAL, EV, CJM, SI and CAH contributed the Review and Critique of the Manuscript. All authors contributed extensively to the work presented in this paper.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Stuebner, E., Vichayanrat, E., Low, D.A. et al. Non-dipping nocturnal blood pressure and psychosis parameters in Parkinson disease. Clin Auton Res 25, 109–116 (2015). https://doi.org/10.1007/s10286-015-0270-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10286-015-0270-5