Abstract
Triple receptor-negative breast cancers (TNBCs) generally have poor prognoses because of the loss of therapeutic targets. As lysophosphatidic acid (LPA) receptor signaling has been shown to affect breast cancer initiation and progression, we try to evaluate the potential roles of LPA receptors in TNBCs. We examined mRNA and protein expressions of LPA receptors 1-3, using quantitative real-time PCR and immunohistochemical analyses in normal (n = 37), benign disease (n = 55), and breast cancer tissues (n = 82). Carcinomas expressed higher levels of LPA2 and LPA3 mRNAs (0.17 ± 0.070 and 0.05 ± 0.023, respectively) than did normal breast tissue (0.13 ± 0.072 and 0.02 ± 0.002, respectively). Enhanced immunohistochemical staining for LPA2 and LPA3 protein was also consistently observed in carcinomas. The LPA3 overexpression was associated with lymph node metastases, and absence of estrogen receptor, progesterone receptors, and human epidermal growth factor receptor 2 expression. TNBC tissues and cell lines showed the highest LPA3 expression compared with luminal-type A and B breast cancers. Suppression of LPA3 by shRNA did not influence cell growth in breast cancer cells. However, the migration and invasion of TNBC cells were significantly inhibited by LPA3-shRNA or inhibitor, which had no or less effect on normal and non-TNBC breast cells. In conclusion, our data indicated that the expression of LPA receptor 3 was increased in human TNBCs and is associated with tumor metastatic ability, and this implies that LPA3 is a potential therapeutic target for the treatment of TNBCs.
Similar content being viewed by others
Introduction
Breast cancer is the most commonly diagnosed cancer, and the leading cause of cancer-related deaths, in women worldwide [1]. Cases are usually classified by their expression of estrogen receptors (ER) progesterone receptors (PR), and human epidermal growth factor-2 receptors (HER2), which together predict treatment response and prognosis [2]. Although hormone receptor (HR)+ breast cancers have many effective treatment options, fewer targeted therapies are available for triple receptor-negative breast cancers (TNBCs). Currently, some progress has been made in classifying TNBCs into several distinct subtypes using gene expression profiling analyses, and some kinases and agents were identified as potential druggable targets [3, 4], but the therapeutic implications are yet to be elucidated [5]. Thus, characterization of novel molecular biomarkers is critically required for the treatment of TNBCs.
Lysophosphatidic acid (LPA) receptors are specific G protein-coupled receptors binding with LPA, which mediates a variety of biological processes, such as cell proliferation, migration, invasion and differentiation [6]. At least six LPA receptors (LPA1–6) are currently identified, and their emerging roles in tumorigenesis have been demonstrated both in vitro and in vivo [7]. In breast tissue, LPA1 and LPA2 are broadly expressed in either normal or abnormal mammary epithelial cells, whereas expression levels of LPA3–6 are more restricted or undetectable, which may account for the various biological effects of LPA [8–10]. Overexpression of LPA1 and LPA2 was readily observed in breast cancers with redundant mediation functions in multiple endogenous LPA responses, including cancer cell growth, metastasis, angiogenesis, and chemoresistance [8, 11–13]. In contrast, less is known about the role of LPA3 in breast cancer initiation and progression. Previous published data showed that LPA3 was higher expression in poorly differentiated breast cancers than well-differentiated tumors [14, 15], which suggests that LPA3 contributes to breast cancer progression.
Although the LPA receptors have been shown to affect breast cancer initiation and progression, the exact expression patterns and functions in TNBCs have not been fully examined. In the present study, we characterized the expression of LPA1–3 in human normal, benign, and malignant breast tissues and cell lines, and analyzed correlations with clinical and pathological findings to highlight the possible roles of LPA receptors in the development and treatment of TNBCs.
Materials and methods
Patients
Specimens of normal breast (n = 37), mammaries with benign disease (n = 55), and breast cancer (n = 82) were collected from the First Affiliated Hospital of Xi’an Jiaotong University. This study was approved by the IRB of Xi’an Jiaotong University School of Medicine. All tissues were pathologically examined. Written informed consent forms were obtained from all subjects, and all clinical investigation had been conducted according to the principles expressed in the Declaration of Helsinki.
RNA isolation and quantitative real-time PCR
Tissues or cells were lysed in the Qiagen RLT lysis buffer (Qiagen, USA). RNA was extracted with an RNeasy mini kit (Qiagen, USA) and reverse transcribed by M-MLV reverse transcriptase (Invitrogen, USA). Quantitative real-time PCR was performed on a Bio-Rad iQ5 Real-Time PCR Detection System (Bio-Rad Laboratories, USA) with a SYBR Green I Master Mix (TAKARA, Japan). PCRs were performed in triplicate, and the relative gene expression was calculated against GAPDH. Primer pairs used in this study were as follows: GAPDH: F, 5′-GAAGGTGAAGGTCGGAGT-3′/R, 5′-GAAGATGGTGATGGGATTTC-3′; LPA1: F, 5′-AATCGAGAGGCACATTACGG-3′/R, 5′-GTTGAAAATGGCCCAGAAGA-3′; LPA2: F, 5′-TTGTCTTCCTGCTCATGGTG-3′/R, 5′-TCAGCATCTCGGCAAGAGTA-3′; LPA3: F, 5′-TGCTCATTTTGCTTGTCTGG-3′/R, 5′-GCCATACATGTCCTCGTCCT-3′.
Immunohistochemistry (IHC) analysis
Formalin-fixed paraffin-embedded sections (5 µm thick) of the normal breast, breast with benign diseases, and breast cancers were analyzed by IHC with the primary LPA1–3 antibody (1:100) and a biotin-conjugated secondary antibody. For IHC quantification, the sections were analyzed using Nikon TE2000-s microscope (Melville, USA). Four randomly selected areas were photographed at 40× magnification using a QimageRetiga 2000R camera (Surrey, Canada). The integral optical density (IOD) of immunoreactivity was calculated using the Image-Pro Plus image analysis software (Media Cybernetics, USA).
Cell lines and culture
The MCF-10A and MCF-7 cells were obtained from Sagene Inc., (Guangzhou, China), and the MCF-12A, T47D, MDA-MB-231, and MDA-MB-157 cells were obtained from ATCC (Manassas, USA). All cell lines were maintained in a humidified atmosphere at 37 °C with 5 % CO2. MCF-10A, MCF-12A, and MCF-7 cells were cultured in DMEM with glutamine, 10 % FBS (Gibco, USA), and 100 μg/mL penicillin/streptomycin (P/S). T47D were cultured in RPMI1640 with glutamine, 10 % FBS (Gibco), and 100 μg/mL P/S. MDA-MB-231 and MDA-MB-157 cultured in Leibovitz’s L-15 Medium (ATCC, USA) with 10 % FBS (Gibco) and 100 μg/mL P/S.
Western blot analyses
Western blot analyses were conducted using standard procedures, and proteins were detected using primary antibodies and fluorescent secondary antibodies (IRDye800CW-conjugated or IRDye680-conjugated anti-species IgG, Li-Cor Biosciences, Lincoln, NE, USA). The fluorescent signals were captured on an Odyssey Infrared Imaging System (Li-Cor Biosciences) with both 700- and 800-nm channels. Boxes were manually placed around each band of interest, and the software returned near-infrared fluorescent values of raw intensity with background subtraction (Odyssey 3.0 analytical software, Li-Cor Biosciences).
shRNA transfection
Six-well plates were seeded with 5 × 104 cells/well in 2 mL media 24 h before transfection; cells were 80–90 % confluent at transfection. Cells were transfected with LPA3 shRNA (100 pmol/well, Santa Cruz Biotechnology, USA) using Lipofectamine 2000 Reagent (Life Technologies, USA) according to the manufacturer’s instruction. After 48 h of transfection, cells were selected using puromycin for 2 weeks. Stable transductants were pooled.
MTT assays
Cells were seeded at a density of 5 × 103 cells/well in 96-well plates at a final volume of 180 µL in incubation, at 37 °C, with 5 % CO2. After different time incubation, 20 µL of 5 mg/mL solution of MTT (Sigma, MO, USA) in PBS was added to each well, and plates were then incubated for 4 h at 37 °C. Reaction crystals were then solubilized in 100 % dimethylsulfoxide (Sigma) 20 µL/well and shaken for 15 min. Absorbance of each well was measured on a multidetection microplate reader (BMG LABTECH, USA) at a wavelength of 570 nm.
Cell migration and invasion Assays
Migration and invasion assays were conducted using transwell plates with 8-μm pore size membranes (Corning Inc., USA) as described previously [16]. After incubation for 4 h (for migration assays) or 24 h (for invasion assays), cells remaining in the upper side of the filter were removed with cotton swabs. The cells attached on the lower surface were fixed and stained using crystal violet and washed with water. Cells were counted with five high power fields per membrane, and results were presented as the mean number of cells migrated per field per membrane. All experiments were conducted in triplicate.
Statistical analyses
Continuous variables were summarized as means with standard deviations (SD) across the healthy control, benign disease, and cancer groups. One-way ANOVA was used to test the overall difference, and Student’s t test was used to test the pairwise difference across disease statuses. Correlation between two different groups was tested by Pearson’s correlation coefficient. P < 0.05 was considered significant. All analyses were performed using SPSS software version 19.0 (IBM, USA).
Results
Expression patterns of LPA1–3 in breast tissues
We evaluated mRNA expression of LPA1–3 in normal, benign, and malignant breast epithelium; mRNA levels were quantified against GAPDH. As shown in Fig. 1a, breast tissues predominantly expressed LPA1 and LPA2, whereas LPA3 expression was weakly but detectable in all specimens. Similar levels of LPA1 mRNA were detected in normal, benign, and carcinoma tissues (0.11 ± 0.058 vs. 0.13 ± 0.044 vs. 0.13 ± 0.034, P = 0.789; Fig. 1b). However, LPA2 mRNA levels in breast cancers were significantly higher than that in normal tissue (0.17 ± 0.070 vs. 0.13 ± 0.072, P = 0.0002; Fig. 1c). Although low levels of LPA3 were observed in all breast tissues, the cancer tissues exhibited a greater expression of LPA3 than did normal (0.05 ± 0.023 vs. 0.02 ± 0.002, P < 0.001) or benign-disease tissues (0.05 ± 0.023 vs. 0.03 ± 0.002, P < 0.001) (Fig. 1d). Notably, LPA3 expression was also greater in benign-disease tissue than in normal tissue (0.03 ± 0.002 vs. 0.02 ± 0.002, P = 0.009; Fig. 1d).
mRNA expression of LPA receptor 1-3 in breast tissues. a To determine whether the samples expressed LPA receptors, quantitative real-time PCR was performed by LPA1, LPA2, and LPA3 primers. The relative gene expression was calculated against GAPDH. b The relative LPA1 mRNA expression in normal breast epithelium, mammary with benign disease, and malignant tissues. c The relative LPA2 mRNA expression in normal breast epithelium, mammary with benign disease, and malignant tissues. d The relative LPA3 mRNA expression in normal breast epithelium, mammary with benign disease, and malignant tissues. ***P < 0.001
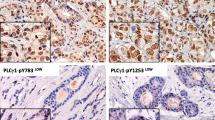
We also immunohistochemically evaluated expression of LPA receptor proteins in the same specimens (Fig. 2a). LPA1–3 was detectable in the cell membrane and cytoplasm in most specimens (113/119 of LPA1, 116/119 of LPA2, and 110/119 of LPA3). As with the mRNA expression, enhanced staining for LPA2 and LPA3 protein was clearly detected in carcinomas in comparison with normal epithelium or benign-disease tissues (Fig. 2c, d), whereas LPA1 expression did not differ significantly between different groups (Fig. 2b). Protein immunoreactivity significant correlated with relative mRNA expression (r = 0.592, P < 0.001).
Relationship between LPA1–3 mRNA expression and clinical parameters in breast cancer patients
Relationships between LPA1–3 mRNA expression and clinical or pathological findings in 82 cases are presented in Table 1. LPA1 expression did not correlate with any clinical parameters. Higher expression of LPA2 was seen in postmenopausal patients (P < 0.05). The higher-stage tumors tended to express less LPA2, but not significantly (P = 0.095). The expression of LPA3 was associated with hormonal receptor status and lymph node metastases. ER−, PR−, or Her2− tumors were more likely to express excess LPA3 than positive ones. Moreover, patients with lymph node metastases presented with higher LPA3 expression than patients without metastases (P < 0.05).
Higher expression of LPA3 in TNBC tissues and cell lines
As LPA3 expression in carcinomas strongly correlated with HR status, we subsequently analyzed the distributions of LPA3 among different tumor immunophenotypes. Breast cancer patients were classified as luminal A, luminal B, and TNBC, based on their expression of ER, PR, Her2, and ki-67 [17]. LPA3 expression differed significantly among tumors with different immunophenotypes (P < 0.001; Fig. 3a). The highest LPA3 protein level was demonstrated in the TNBCs whereas similar expressions were found between luminal A and luminal B carcinomas.
High expression of LPA3 in TNBCs. a The relative LPA3 mRNA expression in breast cancer tissues from luminal A, luminal B and TNBC patients. b The relative LPA3 mRNA expression in six different breast cell lines was determined by quantitative real-time PCR. The results are presented as the mean ± SD against GAPDH obtained in three independent experiments. c Western blots were used to detect protein levels of LPA3 in six breast cell lines. Quantification of protein was presented as the mean ± SD of fluorescent values obtained in three independent experiments. †Compared to normal mammary cells, P < 0.05; ‡compared to normal mammary cells or non-TNBC cells, P < 0.001
To confirm the expression profiles of LPA3 in TNBCs, we further detected the mRNA and protein levels of LPA3 in normal mammary epithelial cells and breast cancer cell lines with different molecular phenotypes. As expected, breast cancer cell lines (MCF-7, T47D, MDA-MB-231, and MDA-MB-157) expressed more LPA3 than normal immortal cells (MCF-10A and MCF-12A), and the highest expression of LPA3 was detected in the TNBC cells (MDA-MB-231 and MDA-MB-157) (Fig. 3b, c).
Inhibition of LPA3 by shRNA decreased migration and invasion of TNBC cells
To further analyze the role of LPA3 in breast tumorigenesis, we conducted cell proliferation, migration, and invasion assays of LPA3- and control-shRNA-transfected breast epithelial cells, including normal immortal cells MCF-10A, luminal cells MCF-7, and TNBC cells MDA-MB-231. LPA3 was effectively down-regulated by shRNA in all three cell lines (Fig. 4a). Cell proliferation tested by MTT showed that suppression of LPA3 did not influence cell growth in all three cell lines (Fig. 4b). However, cells with LPA3-shRNA migrated significantly less than controls in MDA-MB-231 cells (Fig. 4c). Although LPA3-shRNA also reduced migration of MCF-7 cells, the inhibitory capacity was weaker than in MDA-MB-231 cells (Fig. 4c). We also assessed the effect of LPA3 knockdown on cellular invasion and revealed LPA3 loss significantly decreased invasion of MDA-MB-231 cells, but had less or no effect on MCF-10A and MCF-7 cells (Fig. 4d).
Inhibition of LPA3 decreased migration and invasion of TNBC cells. a Expression of LPA3 was decreased by shRNA. MCF-10A, MCF-7, and MDA-MB-231 cells were transfected with control and LPA3 shRNA. Forty-eight hours later, cell lysates were analyzed by Western blots with anti-LPA3 antibody. b The effect of LPA3 on breast cancer cells growth, as measured using the MTT assay. The results are presented as the mean ± SD of fold increased to initiation obtained in 3 independent experiments. c, d Cell transwell assays were conducted to investigate the role of LPA3 on breast cancer cells migration (c) and invasion (d). The results are presented as the mean ± SD of cell number obtained in three independent experiments. **P < 0.01; ***P < 0.001
Ki16425 dose-dependently suppressed migration and invasion of TNBC cells
We used Ki16425, an antagonist for LPA1 and LPA3, to confirm the critical roles of LPA3 in TNBC cells. We first showed that pre-treating MDA-MB-231 cells with Ki16425 did not influence cell viability (Fig. 5a). We then evaluated the effects of Ki16425 on migration and invasion of TNBC cells, using transwell assays. As shown in Fig. 5b, c, Ki16425 suppressed migration and invasion of MDA-MB-231 cells in a dose-dependent manner.
Inactivated LPA3 by Ki16425 suppressed migration and invasion of TNBC cells. a MDA-MB-231 cells were treated with indicated concentrations of Ki16428 for 1 h, and then cell viability was measured using the MTT assay. The results are presented as the mean ± SD of fold increased to initiation obtained in 3 independent experiments. b, c Migration (b) and invasion (c) of MDA-MB-231 cells were inhibited by ki16425. MDA-MB-231 cells were pretreated with indicated concentrations of ki16425 for 1 h and then transferred to collagen- or matrigel-coated transwell chambers for migration and invasion experiments, respectively. *P < 0.05; **P < 0.01; ***P < 0.001
Discussion
LPA receptors are expressed by normal mammary epithelial cells, with aberrant expression occurring during breast cancer initiation and progression [18]. In the present study, we found abnormal expression of LPA receptors in mammary carcinomas, and that LPA2 and LPA3 expression was enhanced in breast cancer compared with normal breast and benign-disease tissues, although the expression level of LPA1 was not significantly different between each subgroup. Particularly, we also showed significantly increased LPA3 expression in the TNBCs compared with other immunophenotype tumors. Subsequently, function analysis revealed that inhibition of LPA3 by shRNA or antagonist dramatically suppressed the migration and invasion ability of TNBC cells, but had no or less effect on normal or luminal-type cancer cells, which suggests a role for LPA3 in the pathophysiology of TNBCs.
Expression and function of LPA1 in the breast cancer have been studied extensively. Overexpression of LPA1 is readily observed in breast cancer cells [19]. Manipulation of LPA1 level or function could alter the survival and metastatic ability of breast cancer cells both in vitro and in vivo [11, 12, 14, 20, 21]. However, in our present research, LPA1 expression levels did not differ significantly between normal and malignant breast tissues. This inconsistency may result from tumor heterogeneity. In breast cancer, LPA1 is expressed in many cancer cell lines, but at various levels. It is most likely that LPA1 higher expressed in more aggressive cell lines, such as MDA-MB-231, and lower in less aggressive breast cancer cells, such as MCF-7 [10, 13, 20, 22, 23]. In accord with cell lines, LPA1 mRNA was significantly more abundant in advanced stages of breast cancer compared with noninvasive stage breast tumors [24]. Moreover, accumulating evidence indicates that the LPA1 contributes to the metastatic capability of breast cancers. Higher LPA1 expression is significantly related to positive node and bone metastases [11, 12], which implies that LPA1 affects breast cancer progression. However, some clinical studies found no major expression pattern for the LPA1 between breast cancer patients and normal controls [8, 25], which suggests that LPA1 has no role in breast cancer initiation.
From an evolutionary perspective, tumors can be as genetically and epigenetically heterogeneous cell populations, although most human tumors are monoclonal outgrowths descending from single progenitor cells [26, 27]. As tumor progression, genetic and epigenetic alterations occur in progeny cells. However, changes in LPA1 expression as they affect breast cancer initiation and progression are barely understood and require additional exploration.
Although the expression and functions of LPA2 have been the subject of fewer studies, increased LPA2 expression has been reported in invasive breast carcinoma [8, 14]. Transgenic mice that overexpress LPA2 showed higher incidence of mammary tumors with early onset than mice that overexpress LPA1, which implicates LPA2 in the initiation of breast cancer [14]. In vitro studies, LPA2 has been verified to regulate LPA-induced breast cancer cells proliferation and migration through Erk or RhoA pathway [23, 28]. Recently, a literature also reported LPA2 involved in LPA-induced IL-6 and IL-8 expression, which promoted colony formation and cell survival of TNBCs [29]. Together with our findings that LPA2 is more highly expressed in breast cancer patients, these combined data validate LPA2 as a potential therapeutic target for drug development and evaluation in breast cancer.
As with LPA2, little is known about the expression patterns of LPA3 in breast cancers. Until recently, Nikolay et al. indicated that LPA3 was higher expressed in human breast cancers, and most interesting LPA3 overexpression was associated with absence of ER and PR [30], which suggests a function of LPA3 in HR− carcinomas. Our studies confirmed that LPA3 was overexpression in ER−/PR−/Her2− tumor cells and tissues when compared with normal breast epithelium and luminal-type cancers. Inhibition of LPA3 significantly decreased migration and invasion of TNBC cells but did not affect other immunotype breast cancers, reflecting on dominant metastatic roles of LPA3 in TNBCs.
Cancer metastasis is a complex biological event of multiple steps, one of which is epithelial to mesenchymal transition (EMT), a prelude to increased cellular motility and plasticity, which thereby enables cellular invasion [31, 32]. Initial evidence for a possible role of LPA and its receptors in EMT was derived from experiments in hepatocellular carcinoma and ovarian cancer by showing a proline-rich tyrosine kinase 2 (PYK2) or periostin (alias osteoblast-specific factor-2)-induced EMT, upon LPA treatment [33, 34]. In the breast cancer, Jahn et al. [35] demonstrated that LPA1 is up-regulated in cells that underwent EMT and consequently led to an increased responsiveness to LPA after EMT. These results imply that the LPA receptors contribute to cell EMT. The roles of different LPA receptors in EMT clearly merit wider investigation.
As a receptor for LPA, LPA3 can promote cancer progression. However, the downstream pathways of LPA3 are rarely elucidated. Currently, evidences indicated that Yes-associated protein (YAP), a transcriptional factor of Hippo pathway, is a critical downstream mediatio of LPA3 in ovarian cancer [36]. Thus, we invested the expression correlation between LPA3 and YAP protein and found that tumors with overexpression of LPA3 exhibited week YAP staining (data not shown). As YAP functions as a breast tumor suppressor [37], LPA3-YAP pathway may involved in initiation and progression of breast cancers. Interesting, another study revealed that loss of YAP expression is associated with estrogen and PR negativity in breast carcinomas [38]. Besides, in transgenic mice model, the ER, PR, and Her2 were significantly decreased in LPA3 overexpression mice when compared to wild-type mice [14]. All together, LPA3, YAP, and hormonal receptors may interact in TNBC pathophysiology. However, the exact mechanism is unclear and requires further study.
References
Jemal A, Bray F, Center MM, Ferlay J, Ward E, Forman D. Global cancer statistics. CA Cancer J Clin. 2011;61(2):69–90. doi:10.3322/caac.20107.
Poage GM, Hartman ZC, Brown PH. Revealing targeted therapeutic opportunities in triple-negative breast cancers: a new strategy. Cell Cycle. 2013;12(17):2705–6. doi:10.4161/cc.25871.
Lehmann BD, Bauer JA, Chen X, Sanders ME, Chakravarthy AB, Shyr Y, et al. Identification of human triple-negative breast cancer subtypes and preclinical models for selection of targeted therapies. J Clin Investig. 2011;121(7):2750–67. doi:10.1172/JCI45014.
Speers C, Tsimelzon A, Sexton K, Herrick AM, Gutierrez C, Culhane A, et al. Identification of novel kinase targets for the treatment of estrogen receptor-negative breast cancer. Clin Cancer Res. 2009;15(20):6327–40. doi:10.1158/1078-0432.CCR-09-1107.
Mohamed A, Krajewski K, Cakar B, Ma CX. Targeted therapy for breast cancer. Am J Pathol. 2013;183(4):1096–112. doi:10.1016/j.ajpath.2013.07.005.
Gotoh M, Fujiwara Y, Yue J, Liu J, Lee S, Fells J, et al. Controlling cancer through the autotaxin-lysophosphatidic acid receptor axis. Biochem Soc Trans. 2012;40(1):31–6. doi:10.1042/BST20110608.
Willier S, Butt E, Grunewald TG. Lysophosphatidic acid (LPA) signalling in cell migration and cancer invasion: a focussed review and analysis of LPA receptor gene expression on the basis of more than 1700 cancer microarrays. Biol Cell. 2013;105(8):317–33. doi:10.1111/boc.201300011.
Kitayama J, Shida D, Sako A, Ishikawa M, Hama K, Aoki J, et al. Over-expression of lysophosphatidic acid receptor-2 in human invasive ductal carcinoma. Breast Cancer Res. 2004;6(6):R640–6. doi:10.1186/bcr935.
Wu J, Mukherjee A, Lebman DA, Fang X. Lysophosphatidic acid-induced p21Waf1 expression mediates the cytostatic response of breast and ovarian cancer cells to TGFbeta. Mol Cancer Res. 2011;9(11):1562–70. doi:10.1158/1541-7786.MCR-11-0340.
Hama K, Aoki J, Fukaya M, Kishi Y, Sakai T, Suzuki R, et al. Lysophosphatidic acid and autotaxin stimulate cell motility of neoplastic and non-neoplastic cells through LPA1. J Biol Chem. 2004;279(17):17634–9. doi:10.1074/jbc.M313927200.
David M, Ribeiro J, Descotes F, Serre CM, Barbier M, Murone M, et al. Targeting lysophosphatidic acid receptor type 1 with Debio 0719 inhibits spontaneous metastasis dissemination of breast cancer cells independently of cell proliferation and angiogenesis. Int J Oncol. 2012;40(4):1133–41. doi:10.3892/ijo.2011.1309.
Boucharaba A, Serre CM, Guglielmi J, Bordet JC, Clezardin P, Peyruchaud O. The type 1 lysophosphatidic acid receptor is a target for therapy in bone metastases. Proc Natl Acad Sci USA. 2006;103(25):9643–8. doi:10.1073/pnas.0600979103.
Samadi N, Bekele RT, Goping IS, Schang LM, Brindley DN. Lysophosphatidate induces chemo-resistance by releasing breast cancer cells from taxol-induced mitotic arrest. PLoS One. 2011;6(5):e20608. doi:10.1371/journal.pone.0020608.
Liu S, Umezu-Goto M, Murph M, Lu Y, Liu W, Zhang F, et al. Expression of autotaxin and lysophosphatidic acid receptors increases mammary tumorigenesis, invasion, and metastases. Cancer Cell. 2009;15(6):539–50. doi:10.1016/j.ccr.2009.03.027.
Popnikolov NK, Dalwadi BH, Thomas JD, Johannes GJ, Imagawa WT. Association of autotaxin and lysophosphatidic acid receptor 3 with aggressiveness of human breast carcinoma. Tumour Biol. 2012;33(6):2237–43. doi:10.1007/s13277-012-0485-1.
Sengupta S, Xiao YJ, Xu Y. A novel laminin-induced LPA autocrine loop in the migration of ovarian cancer cells. FASEB J. 2003;17(11):1570–2. doi:10.1096/fj.02-1145fje.
Sorlie T, Perou CM, Tibshirani R, Aas T, Geisler S, Johnsen H, et al. Gene expression patterns of breast carcinomas distinguish tumor subclasses with clinical implications. Proc Natl Acad Sci USA. 2001;98(19):10869–74. doi:10.1073/pnas.191367098.
Panupinthu N, Lee HY, Mills GB. Lysophosphatidic acid production and action: critical new players in breast cancer initiation and progression. Br J Cancer. 2010;102(6):941–6. doi:10.1038/sj.bjc.6605588.
Witt AE, Hines LM, Collins NL, Hu YH, Gunawardane RN, Moreira D, et al. Functional proteomics approach to investigate the biological activities of cDNAs implicated in breast cancer. J Proteome Res. 2006;5(3):599–610. doi:10.1021/Pr050395i.
Goetzl EJ, Dolezalova H, Kong Y, Zeng L. Dual mechanisms for lysophospholipid induction of proliferation of human breast carcinoma cells. Cancer Res. 1999;59(18):4732–7.
Hama K, Aoki J, Fukaya M, Kishi Y, Sakai T, Suzuki R. Lysophosphatidic acid and autotaxin stimulate cell motility of neoplastic and non-neoplastic cells through LPA(1). J Biol Chem. 2004;279(17):17634–9. doi:10.1074/jbc.M313927200.
Swamydas M, Nguyen D, Allen LD, Eddy J, Dreau D. Progranulin stimulated by LPA promotes the migration of aggressive breast cancer cells. Cell Commun Adhes. 2011;18(6):119–30. doi:10.3109/15419061.2011.641042.
Chen M, Towers LN, O’Connor KL. LPA2 (EDG4) mediates Rho-dependent chemotaxis with lower efficacy than LPA1 (EDG2) in breast carcinoma cells. Am J Physiol Cell Physiol. 2007;292(5):C1927–33. doi:10.1152/ajpcell.00400.2006.
Li TT, Alemayehu M, Aziziyeh AI, Pape C, Pampillo M, Postovit LM, et al. Beta-arrestin/Ral signaling regulates lysophosphatidic acid-mediated migration and invasion of human breast tumor cells. Mol Cancer Res. 2009;7(7):1064–77. doi:10.1158/1541-7786.MCR-08-0578.
Murph MM, Nguyen GH, Radhakrishna H, Mills GB. Sharpening the edges of understanding the structure/function of the LPA1 receptor: expression in cancer and mechanisms of regulation. BBA Mol Cell Biol Lipids. 2008;1781(9):547–57. doi:10.1016/j.bbalip.2008.04.007.
Grunewald TG, Herbst SM, Heinze J, Burdach S. Understanding tumor heterogeneity as functional compartments—superorganisms revisited. J Transl Med. 2011;9:79. doi:10.1186/1479-5876-9-79.
Merlo LM, Pepper JW, Reid BJ, Maley CC. Cancer as an evolutionary and ecological process. Nat Rev Cancer. 2006;6(12):924–35. doi:10.1038/nrc2013.
Wu JH, Mukherjee A, Lebman DA, Fang XJ. Lysophosphatidic acid-induced p21(Waf1) expression mediates the cytostatic response of breast and ovarian cancer cells to TGF beta. Mol Cancer Res. 2011;9(11):1562–70. doi:10.1158/1541-7786.Mcr-11-0340.
Hartman ZC, Poage GM, den Hollander P, Tsimelzon A, Hill J, Panupinthu N, et al. Growth of triple-negative breast cancer cells relies upon coordinate autocrine expression of the proinflammatory cytokines IL-6 and IL-8. Cancer Res. 2013;73(11):3470–80. doi:10.1158/0008-5472.Can-12-4524-T.
Popnikolov NK, Dalwadi BH, Thomas JD, Johannes GJ, Imagawa WT. Association of autotaxin and lysophosphatidic acid receptor 3 with aggressiveness of human breast carcinoma. Tumor Biol. 2012;33(6):2237–43. doi:10.1007/s13277-012-0485-1.
Bullock MD, Sayan AE, Packham GK, Mirnezami AH. MicroRNAs: critical regulators of epithelial to mesenchymal (EMT) and mesenchymal to epithelial transition (MET) in cancer progression. Biol Cell. 2012;104(1):3–12. doi:10.1111/boc.201100115.
De Craene B, Berx G. Regulatory networks defining EMT during cancer initiation and progression. Nat Rev Cancer. 2013;13(2):97–110. doi:10.1038/nrc3447.
Choi KU, Yun JS, Lee IH, Heo SC, Shin SH, Jeon ES, et al. Lysophosphatidic acid-induced expression of periostin in stromal cells: prognostic relevance of periostin expression in epithelial ovarian cancer. Int J Cancer. 2011;128(2):332–42. doi:10.1002/ijc.25341.
Sun CK, Ng KT, Lim ZX, Cheng Q, Lo CM, Poon RT, et al. Proline-rich tyrosine kinase 2 (Pyk2) promotes cell motility of hepatocellular carcinoma through induction of epithelial to mesenchymal transition. PLoS One. 2011;6(4):e18878. doi:10.1371/journal.pone.0018878.
Jahn SC, Law ME, Corsino PE, Parker NN, Pham K, Davis BJ, et al. An in vivo model of epithelial to mesenchymal transition reveals a mitogenic switch. Cancer Lett. 2012;326(2):183–90. doi:10.1016/j.canlet.2012.08.013.
Cai H, Xu Y. The role of LPA and YAP signaling in long-term migration of human ovarian cancer cells. Cell Commun Signal. 2013;11. doi:10.1186/1478-811x-11-31.
Yuan M, Tomlinson V, Lara R, Holliday D, Chelala C, Harada T, et al. Yes-associated protein (YAP) functions as a tumor suppressor in breast. Cell Death Differ. 2008;15(11):1752–9. doi:10.1038/cdd.2008.108.
Tufail R, Jorda M, Zhao W, Reis I, Nawaz Z. Loss of Yes-associated protein (YAP) expression is associated with estrogen and progesterone receptors negativity in invasive breast carcinomas. Breast Cancer Res Treat. 2012;131(3):743–50. doi:10.1007/s10549-011-1435-0.
Acknowledgments
This work is supported by the National Natural Science Foundation of China (Grant No. 81171397).
Conflict of interest
The authors declare no completing interests related to this work.
Author information
Authors and Affiliations
Corresponding authors
Additional information
Kai Sun and Hui Cai have contributed equally to this work.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution License which permits any use, distribution, and reproduction in any medium, provided the original author(s) and the source are credited.
About this article
Cite this article
Sun, K., Cai, H., Duan, X. et al. Aberrant expression and potential therapeutic target of lysophosphatidic acid receptor 3 in triple-negative breast cancers. Clin Exp Med 15, 371–380 (2015). https://doi.org/10.1007/s10238-014-0306-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10238-014-0306-5