Abstract
Recent long-term studies showed an unsatisfactory recurrence rate of severe mitral regurgitation 3–5 years after surgical repair, suggesting that excessive tissue stresses and the resulting strain-induced tissue failure are potential etiological factors controlling the success of surgical repair for treating mitral valve (MV) diseases. We hypothesized that restoring normal MV tissue stresses in MV repair techniques would ultimately lead to improved repair durability through the restoration of MV normal homeostatic state. Therefore, we developed a micro- and macro- anatomically accurate MV finite element model by incorporating actual fiber microstructural architecture and a realistic structure-based constitutive model. We investigated MV closing behaviors, with extensive in vitro data used for validating the proposed model. Comparative and parametric studies were conducted to identify essential model fidelity and information for achieving desirable accuracy. More importantly, for the first time, the interrelationship between the local fiber ensemble behavior and the organ-level MV closing behavior was investigated using a computational simulation. These novel results indicated not only the appropriate parameter ranges, but also the importance of the microstructural tuning (i.e., straightening and re-orientation) of the collagen/elastin fiber networks at the macroscopic tissue level for facilitating the proper coaptation and natural functioning of the MV apparatus under physiological loading at the organ level. The proposed computational model would serve as a logical first step toward our long-term modeling goal—facilitating simulation-guided design of optimal surgical repair strategies for treating diseased MVs with significantly enhanced durability.












Similar content being viewed by others
Notes
A convective curvilinear cylindrical coordinate was adopted to describe the contiguous MV leaflet entity, and fiber directions were assumed to be all uniformly aligned with the circumferential direction in this coordinate system for the case associated with uniformly curvilinear fiber directions.
FE simulations of MV systolic closure (\(\sim \)0.3 s) were performed on PC with Intel Xeon X5650 processor with one single thread and 32 GB memory, and each job with 300,000 time increments took \(\sim \)5 h for completion.
References
Adams DH, Rosenhek R, Falk V (2010) Degenerative mitral valve regurgitation: best practice revolution. Eur Heart J 31:1958–1966
Aggarwal A, Aguilar VS, Lee C-H, Ferrari G, Gorman JH, Gorman RC, Sacks MS (2013) Patient-specific modeling of heart valves: from image to simulation. In: Qurselin S, Rueckert D, Smith N (eds) Functional imaging and modeling of the heart. Springer, Berlin, pp 141–149
Aggarwal A, Ferrari G, Joyce E, Daniels MJ, Sainger R, Gorman JH 3rd, Gorman R, Sacks MS (2014) Architectural trends in the human normal and bicuspid aortic valve leaflet and its relevance to valve disease. Ann Biomed Eng 42:986–998
Amini R, Eckert CE, Koomalsingh K, McGarvey J, Minakawa M, Gorman JH, Gorman RC, Sacks MS (2012) On the in vivo deformation of the mitral valve anterior leaflet: effects of annular geometry and referential configuration. Ann Biomed Eng 40:1455–1467
Bouxsein ML, Boyd SK, Christiansen BA, Guldberg RE, Jepsen KJ, Müller R (2010) Guidelines for assessment of bone microstructure in rodents using micro-computed tomography. J Bone Miner Res 25:1468–1486
Braunberger E, Deloche A, Berrebi A, Abdallah F, Celestin JA, Meimoun P, Chatellier G, Chauvaud S, Fabiani JN, Carpentier A (2001) Very long-term results (more than 20 years) of valve repair with carpentier’s techniques in nonrheumatic mitral valve insufficiency. Circulation 104:I8–11
Carpentier A (1983) Cardiac valve surgery-the “French correction”. J Thorac Cardiovasc Surg 86:323–337
Carpentier A, Relland J, Deloche A, Fabiani J-N, D’Allaines C, Blondeau P, Piwnica A, Chauvaud S, Dubost C (1978) Conservative management of the prolapsed mitral valve. Ann Thorac Surg 26:294–302
Choi A, Rim Y, Mun JS, Kim H (2014) A novel finite element-based patient-specific mitral valve repair: virtual ring annuloplasty. Biomed Mater Eng 24:341–347
Dal-Bianco JP, Aikawa E, Bischoff J, Guerrero JL, Handschumacher MD, Sullivan S, Johnson B, Titus JS, Iwamoto Y, Wylie-Sears J, Levine RA, Carpentier A (2009) Active adaptation of the tethered mitral valve: insights into a compensatory mechanism for functional mitral regurgitation. Circulation 120:334–342
David TE, Ivanov J, Armstrong S, Christie D, Rakowski H (2005) A comparison of outcomes of mitral valve repair for degenerative disease with posterior, anterior, and bileaflet prolapse. J Thorac Cardiovasc Surg 130:1242–1249
David TE, Omran A, Armstrong S, Sun Z, Ivanov J (1998) Long-term results of mitral valve repair for myxomatous disease with and without chordal replacement with expanded polytetrafluoroethylene sutures. J Thorac Cardiovasc Surg 115:1279–1286
Eckert CE, Zubiate B, Vergnat M, Gorman JH 3rd, Gorman RC, Sacks MS (2009) In vivo dynamic deformation of the mitral valve annulus. Ann Biomed Eng 37:1757–1771
Einstein DR, Kunzelman KS, Reinhall PG, Cochran RP, Nicosia MA (2004) Haemodynamic determinants of the mitral valve closure sound: a finite element study. Med Biol Eng Comput 42:832–846
Einstein DR, Kunzelman KS, Reinhall PG, Nicosia MA, Cochran RP (2005) The relationship of normal and abnormal microstructural proliferation to the mitral valve closure sound. J Biomech Eng 127:134–147
Fan R, Sacks MS (2014) Simulation of planar soft tissues using a structural constitutive model: finite element implementation and validation. J Biomech 47:2043–2054
Flameng W, Herijgers P, Bogaerts K (2003) Recurrence of mitral valve regurgitation after mitral valve repair in degenerative valve disease. Circulation 107:1609–1613
Flameng W, Meuris B, Herijgers P, Herregods M-C (2008) Durability of mitral valve repair in Barlow disease versus fibroelastic deficiency. J Thorac Cardiovasc Surg 135:274–282
Flugge W (1972) Tensor analysis and continuum mechanics. Springer, New York
Frater R, Vetter H, Zussa C, Dahm M (1990) Chordal replacement in mitral valve repair. Circulation 82:IV125–IV130
Fung YC (1993) Biomechanics: mechanical properties of living tissues, 2nd edn. Springer, New York
Gillinov AM, Blackstone EH, Nowicki ER, Slisatkorn W, Al-Dossari G, Johnston DR, George KM, Houghtaling PL, Griffin B, Sabik JF III (2008) Valve repair versus valve replacement for degenerative mitral valve disease. J Thorac Cardiovas Surg 135:885–893 e882
Gorman JH 3rd, Gupta KB, Streicher JT, Gorman RC, Jackson BM, Ratcliffe MB, Bogen DK, Edmunds LH Jr (1996) Dynamic three-dimensional imaging of the mitral valve and left ventricle by rapid sonomicrometry array localization. J Thorac Cardiovasc Surg 112:712–726
Gorman RC, Gorman JH 3rd (2006) Why should we repair ischemic mitral regurgitation? Ann Thorac Surg 81:785 (author reply 785–786)
Grande-Allen KJ, Borowski AG, Troughton RW, Houghtaling PL, Dipaola NR, Moravec CS, Vesely I, Griffin BP (2005) Apparently normal mitral valves in patients with heart failure demonstrate biochemical and structural derangements: an extracellular matrix and echocardiographic study. J Am Coll Cardiol 45:54–61
Grashow JS, Yoganathan AP, Sacks MS (2006) Biaxial stress-stretch behavior of the mitral valve anterior leaflet at physiologic strain rates. Ann Biomed Eng 34:315–325
He Z, Ritchie J, Grashow JS, Sacks MS, Yoganathan AP (2005) In vitro dynamic strain behavior of the mitral valve posterior leaflet. J Biomech Eng 127:504–511
Jassar AS, Minakawa M, Shuto T, Robb JD, Koomalsingh KJ, Levack MM, Vergnat M, Eperjesi TJ, Jackson BM, Gorman JH III (2012) Posterior leaflet augmentation in ischemic mitral regurgitation increases leaflet coaptation and mobility. Ann Thorac Surg 94:1438–1445
Jensen MO, Jensen H, Levine RA, Yoganathan AP, Andersen NT, Nygaard H, Hasenkam JM, Nielsen SL (2011) Saddle-shaped mitral valve annuloplasty rings improve leaflet coaptation geometry. J Thorac Cardiovasc Surg 142:697–703
Jimenez JH, Soerensen DD, He Z, He S, Yoganathan AP (2003) Effects of a saddle shaped annulus on mitral valve function and chordal force distribution: an in vitro study. Ann Biomed Eng 31:1171–1181
Kincaid EH, Riley RD, Hines MH, Hammon JW, Kon ND (2004) Anterior leaflet augmentation for ischemic mitral regurgitation. Ann Thorac Surg 78:564–568 discussion 568
Komeda M, Glasson JR, Bolger AF, Daughters GT 2nd, MacIsaac A, Oesterle SN, Ingels NB Jr, Miller DC (1997) Geometric determinants of ischemic mitral regurgitation. Circulation 96(II):128–133
Krishnamurthy G, Ennis DB, Itoh A, Bothe W, Swanson JC, Karlsson M, Kuhl E, Miller DC, Ingels NB Jr (2008) Material properties of the ovine mitral valve anterior leaflet in vivo from inverse finite element analysis. Am J Physiol Heart Circ Physiol 295:H1141–H1149
Kunzelman KS, Cochran RP, Chuong C, Ring WS, Verrier ED, Eberhart RD (1993a) Finite element analysis of the mitral valve. J Heart Valve Dis 2:326–340
Kunzelman KS, Cochran RP, Murphree SS, Ring WS, Verrier ED, Eberhart RC (1993b) Differential collagen distribution in the mitral valve and its influence on biomechanical behaviour. J Heart Valve Dis 2:236–244
Kunzelman KS, Einstein DR, Cochran RP (2007) Fluid-structure interaction models of the mitral valve: function in normal and pathological states. Philos Trans R Soc Lond B Biol Sci 362:1393–1406
Kunzelman KS, Reimink MS, Cochran RP (1998) Flexible versus rigid ring annuloplasty for mitral valve annular dilatation: a finite element model. J Heart Valve Dis 7:108–116
Lanir Y (1983) Constitutive equations for fibrous connective tissues. J Biomech 16:1–12
Lee C-H, Amini R, Sakamoto Y, Carruthers CA, Aggarwal A, Gorman RC, Gorman JH III, Sacks MS (2015a) Mitral valves: a computational framework. In: De S, Hwang W, Kuhl E (eds) Multiscale modeling in biomechanics and mechanobiology. Springer, London, pp 223–255
Lee CH, Amini R, Gorman RC, Gorman JH 3rd, Sacks MS (2014) An inverse modeling approach for stress estimation in mitral valve anterior leaflet valvuloplasty for in-vivo valvular biomaterial assessment. J Biomech 47:2055–2063
Lee CH, Carruthers CA, Ayoub S, Gorman RC, Gorman JH, Sacks MS (2015b) Quantification and simulation of layer-specific mitral valve interstitial cell deformation under physiological loading. J Theor Biol 373:26–39
Lee CH, Zhang W, Liao J, Carruthers CA, Sacks J, Sacks MS (2015c) On the presence of affine fibril and fiber kinematics in the mitral valve anterior leaflet under simulated physiological loading. Biophys J 108:1–14
Mahmood F, Gorman JH 3rd, Subramaniam B, Gorman RC, Panzica PJ, Hagberg RC, Lerner AB, Hess PE, Maslow A, Khabbaz KR (2010) Changes in mitral valve annular geometry after repair: saddle-shaped versus flat annuloplasty rings. Ann Thorac Surg 90:1212–1220
Mansi T, Voigt I, Georgescu B, Zheng X, Mengue EA, Hackl M, Ionasec RI, Noack T, Seeburger J, Comaniciu D (2012) An integrated framework for finite-element modeling of mitral valve biomechanics from medical images: application to MitralClip intervention planning. Med Image Anal 16:1330–1346
May-Newman K, Yin FC (1998) A constitutive law for mitral valve tissue. J Biomech Eng 120:38–47
Pouch AM, Wang H, Takabe M, Jackson BM, Gorman J, Gorman RC, Yushkevich PA, Sehgal CM (2014) Fully automatic segmentation of the mitral leaflets in 3D transesophageal echocardiographic images using multi-atlas joint label fusion and deformable medial modeling. Med Image Anal 18:118–129
Prot V, Haaverstad R, Skallerud B (2009) Finite element analysis of the mitral apparatus: annulus shape effect and chordal force distribution. Biomech Model Mechanobiol 8:43–55
Prot V, Skallerud B (2009) Nonlinear solid finite element analysis of mitral valves with heterogeneous leaflet layers. Comput Mech 43:353–368
Prot V, Skallerud B, Holzapfel G (2007) Transversely isotropic membrane shells with application to mitral valve mechanics. Constitutive modelling and finite element implementation. Int J Numer Methods Eng 71:987–1008
Rabbah J-P, Saikrishnan N, Yoganathan AP (2013) A novel left heart simulator for the multi-modality characterization of native mitral valve geometry and fluid mechanics. Ann Biomed Eng 41:305–315
Rabkin-Aikawa E, Farber M, Aikawa M, Schoen FJ (2004) Dynamic and reversible changes of interstitial cell phenotype during remodeling of cardiac valves. J Heart Valve Dis 13:841–847
Reimink MS, Kunzelman KS, Verrier ED, Cochran RP (1995) The effect of anterior chordal replacement on mitral valve function and stresses. A finite element study. Asaio J 41:M754–762
Ritchie J, Jimenez J, He Z, Sacks MS, Yoganathan AP (2006) The material properties of the native porcine mitral valve chordae tendineae: an in vitro investigation. J Biomech 39:1129–1135
Robb JD, Minakawa M, Koomalsingh KJ, Shuto T, Jassar AS, Ratcliffe SJ, Gorman RC, Gorman JH, 3rd (2011) Posterior leaflet augmentation improves leaflet tethering in repair of ischemic mitral regurgitation. Eur J Cardiothorac Surg 40(6):1501–1507
Sacks MS (2003) Incorporation of experimentally-derived fiber orientation into a structural constitutive model for planar collagenous tissues. J Biomech Eng 125:280–287
Sacks MS, Chuong CJ, Templeton GH, Peshock R (1993) In vivo 3-D reconstruction and geometric characterization of the right ventricular free wall. Ann Biomed Eng 21:263–275
Sacks MS, He Z, Baijens L, Wanant S, Shah P, Sugimoto H, Yoganathan AP (2002) Surface strains in the anterior leaflet of the functioning mitral valve. Ann Biomed Eng 30:1281–1290
Sacks MS, Smith DB, Hiester ED (1997) A small angle light scattering device for planar connective tissue microstructural analysis. Ann Biomed Eng 25:678–689
Sacks MS, Yoganathan AP (2008) Heart valve function: a biomechanical perspective. Philos Trans R Soc Lond B Biol Sci 363:2481
Schoen FJ, Levy RJ (2005) Calcification of tissue heart valve substitutes: progress toward understanding and prevention. Ann Thorac Surg 79:1072–1080
Shuhaiber J, Anderson RJ (2007) Meta-analysis of clinical outcomes following surgical mitral valve repair or replacement. Eur J Cardiothorac Surg 31:267–275
Skallerud B, Prot V, Nordrum IS (2011) Modeling active muscle contraction in mitral valve leaflets during systole: a first approach. Biomech Model Mechanobiol 10:11–26
Smith DB, Sacks MS, Vorp DA, Thornton M (2000) Surface geometric analysis of anatomic structures using biquintic finite element interpolation. Ann Biomed Eng 28:598–611
Stevanella M, Maffessanti F, Conti CA, Votta E, Arnoldi A, Lombardi M, Parodi O, Caiani EG, Redaelli A (2011) Mitral valve patient-specific finite element modeling from cardiac MRI: application to an annuloplasty procedure. Cardiovas Eng Technol 2:66–76
Stevanella M, Votta E, Redaelli A (2009) Mitral valve finite element modeling: implications of tissues’ nonlinear response and annular motion. J Biomech Eng 131:121010
Vassileva CM, Boley T, Markwell S, Hazelrigg S (2011) Meta-analysis of short-term and long-term survival following repair versus replacement for ischemic mitral regurgitation. Eur J Cardiothorac Surg 39:295–303
Votta E, Le TB, Stevanella M, Fusini L, Caiani EG, Redaelli A, Sotiropoulos F (2013) Toward patient-specific simulations of cardiac valves: state-of-the-art and future directions. J Biomech 46:217–228
Wang Q, Sun W (2013) Finite element modeling of mitral valve dynamic deformation using patient-specific multi-slices computed tomography scans. Ann Biomed Eng 41:142–153
Acknowledgments
Support from the National Institutes of Health (NIH) Grants R01 HL119297, HL63954, HL103723, and HL73021 is greatly acknowledged. Dr. Chung-Hao Lee was supported in part by the American Heart Association (AHA) Postdoctoral Fellowship (14POST18160013) and a UT Austin ICES Postdoctoral Fellowship. The assistance from Ted Weber and Ronen G. Aniti for image segmentation and development of the MV finite element model is greatly appreciated.
Conflict of interest
None of the authors have a conflict of interests with the present work.
Author information
Authors and Affiliations
Corresponding author
Appendices
Appendix 1: Computation of displacement errors at fiducial marker positions
Each of the shell elements for the MV median leaflet surfaces at the reference configuration (Fig. 5a) developed in Sect. 2.3 was first extruded toward the left atrial direction with a distance of half the elemental thickness in order to obtain the FE mesh for the atrial leaflet surfaces. Then, each of all the 266 fiducial marker was associated with one shell element whose element region entirely covers this fiducial marker, and the corresponding four shape functions \((N_{1},N_{2},N_{3},N_{4})\) were computed based on the positions of the four nodes of this identified element as well as the fiducial marker location on the expanded 2D parametric domain \((s,t)\) (Fig. 12). Similar extrusion procedure was performed for the FE meshes under deformations at 30 and 70 mmHg transvalvular pressure, respectively, and the FE-predicted position of each fiducial marker was obtained by interpolation using the above four shape functions and the current locations of the four nodes
where \((\bar{{\mathbf{x}}}_{J}^{t} ,\bar{{\mathbf{y}}}_{J}^{t} ,\bar{{\mathbf{z}}}_{J}^{t} )\) is the current position (after extrusion) of node \(J\) in the deformed configuration \(\varOmega _{t}\), and superscript t denotes the state (30 or 70 mmHg). Finally, the displacement errors at the fiducial markers were evaluated by comparing the micro-CT segmented locations and the FE predictions as follows
Appendix 2: Kinematics and strain computations in the convective curvilinear coordinates
We modified previously developed approaches (Sacks et al. 1993, 2002; Smith et al. 2000) for computation of the strain field within the fiducial marker array by adopting an in-surface convective curvilinear coordinate system (\(u,v,n\)) based on the local tangent plane (Fig. 12). This coordinate system was defined with unit vectors \(\mathbf{e}_{v} \) parallel to the cylindrically circumferential direction, \(\mathbf{e}_{n} \) being the local surface normal, and \(\mathbf{e}_{v} =\mathbf{e}_{n} \times \mathbf{e}_{v} \). The 3D position vector of each marker (\(x,y,z\)) at different configurations was then translated and rotated into this (\(u,v,n\)) coordinate system. In this work, we utilized a point-based meshless surface interpolation to calculate the in-surface strain field within the MV leaflet delimited by the markers. The position vectors of each point at the reference state and the deformed state were given by
where \(\mathbf{R}_{u}^0 , \mathbf{R}_{v}^0 \), and \(\mathbf{R}_{n}^0 \) are the \(u, v, n\) components of the position vector associated with the reference state, and \(\mathbf{r}_{u}^t , \mathbf{r}_{v}^t \), and \(\mathbf{r}_{n}^t \) are the \(u,v,n\) components of the position vector corresponding to the deformed state. In this study, these components were computed by using the spline interpolation
Here, subscript \({ J}\in \{u,v,n\}, (\mathbf{R}_J^0 )_I \) and \((\mathbf{r}_J^t )_I \) are the \(J\)-components of the position vectors of marker \(I\) corresponding to the reference and deformed states, respectively, and \(\phi _\mathrm{I} (s,t;s_I ,t_I )\) is the \(C^{2}\)-continuous cubic spline function of marker I with a compact support d covering NP markers which has the form
where \(z_I (s,t;s_I ,t_I )\equiv {\sqrt{(s_I -s)^{2}+(t_I -t)^{2}}}/d, \mathrm{d}\) was chosen as twice of the average marker distance, and the covering fiducial makers were determined on the expanded 2D parametric domain (\(s,t\)) (Fig. 12). Hence, the covariant base vectors on the MV leaflet surfaces were determined by
where subscript \(\alpha \in \{u,v\}, \mathbf{G}_\alpha \) and \(\mathbf{g}_\alpha \) are the covariant base vectors in the reference and deformed configurations, respectively, and the third covariant base vectors were computed by \(\mathbf{G}_3 ={(\mathbf{G}_1 \times \mathbf{G}_2 )}/{||\mathbf{G}_1 \times \mathbf{G}_2 ||}\) and \(\mathbf{g}_3 ={(\mathbf{g}_1 \times \mathbf{g}_2 )}/{||\mathbf{g}_1 \times \mathbf{g}_2 ||}\). Then, the contra-variant base vectors were computed by their definition
After carrying out the components of each base vector, the in-plane deformation gradient tensor \(\mathbf{F}_{2\mathrm{D}} \) (used for the mapping algorithm presented in Sect. 2.3), right Cauchy–Green deformation tensor \(\mathbf{C}_{2\mathrm{D}} \), and Euler–Almansi strain tensor \(\mathbf{e}_{2\mathrm{D}} \) (served as validation data in Sects. 2.6, 2.7) were computed (Flugge 1972; Fung 1993) as the following:
Finally, the corresponding principal stretches \((\lambda _\mathrm{R},\lambda _\mathrm{C})\) and the principal directions can then be obtained by solving the eigenvalue problem of the above Euler-Almansi strain tensor for the eigenvalues and eigenvectors.
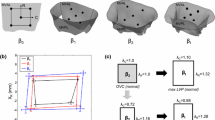
Appendix 3: Summary of validations of the in-surface principal stretches and sensitivity study
The FE-predicted maximum and minimum stretches in the central regions of the MV two leaflets at 70 mmHg transvalvular pressure were reported as follows: \(\lambda _\mathrm{R}=1.39 \pm 0.03\) and \(\lambda _\mathrm{C}=1.12 \pm 0.04\) for the MV anterior leaflet, and \(\lambda _\mathrm{R}=1.48 \pm 0.05\) and \(\lambda _\mathrm{C}=1.11 \pm 0.03\) for the MV posterior leaflet, whereas the in vitro experimental measurements were \(\lambda _\mathrm{R}=1.39 \pm 0.03\) and \(\lambda _\mathrm{C}=1.12 \pm 0.04\) for the MVAL, and \(\lambda _\mathrm{R}=1.48 \pm 0.04\) and \(\lambda _\mathrm{C}=1.11 \pm 0.02\) for the MVPL. Furthermore, the principal directions associated with the principal stretches from both numerical predictions and experimental data were very smooth, especially in the central regions of the MVAL and MVPL, and were in good alignment with the radial and circumferential directions, respectively (Figs. 13, 14). For the sensitivity study on the leaflet microstructural information, the FE prediction accuracy with various levels of model fidelity was evaluated based on the displacement errors at the fiducial marker positions at 70 mmHg transvalvular pressure (Fig. 15).
Comparison of the FE-predicted displacement errors at 70 mmHg transvalvular pressure with an increasing level of model fidelity: a level I—isotropic material, b level II—transversely isotropic material with uniformly curvilinear fiber directions and identical fiber dispersions, c level III—transversely isotropic material with uniformly curvilinear fiber directions and mapped fiber dispersions, and d level IV—transversely isotropic material with mapped fiber directions (via the proposed mapping technique) and mapped fiber dispersions
Rights and permissions
About this article
Cite this article
Lee, CH., Rabbah, JP., Yoganathan, A.P. et al. On the effects of leaflet microstructure and constitutive model on the closing behavior of the mitral valve. Biomech Model Mechanobiol 14, 1281–1302 (2015). https://doi.org/10.1007/s10237-015-0674-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10237-015-0674-0