Abstract
Background
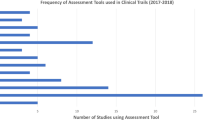
PASI is an inadequate outcome measure for the assessment of psoriasis treatments. No currently used endpoints provide a benefit: risk assessment of treatment taking into consideration all available efficacy and safety data.
Objective
To propose a new outcome measure called “safe psoriasis control” (SPC), which assesses multiple dimensions of the disease in a clinically meaningful way through the combined use of appropriate efficacy, quality of life, and safety data.
Methods
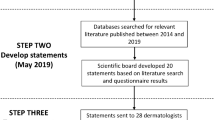
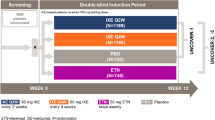
Data from 3,500 subjects were used for the purpose of derivation and validation of the SPC endpoint. Advanced statistical methodology was used to evaluate and validate important components in the assessment of therapeutic benefit.
Results
SPC was shown to be a simple but meaningful combined endpoint showing the proportion of patients who had treatment benefit without major side effects.
Conclusion
The SPC endpoint may be a step-forward in providing a composite tool for the evaluation of treatments for psoriasis.
Sommaire
Antécédents
Le PASI est un élément de mesure inadéquat pour l’évaluation des traitements du psoriasis. Aucun paramètre utilisé actuellement ne permet d’évaluer le ratio bénéfice/risque d’un traitement en tenant compte de toutes les données concernant l’efficacité et l’innocuité.
Objectif
Proposer une nouvelle mesure, appelée «Contrôle sécuritaire du psoriasis» (CSP), qui évalue plusieurs dimensions de la maladie, de façon significative du point de vue clinique, au moyen de données sur l’efficacité, la qualité de vie et l’innocuité.
Méthodes
Des données sur 3 500 sujets ont été utilisées pour fin de calcul et de validation des paramètres du CSP. Une méthodologie statistique avancée a servi à évaluer et à valider des composantes essentielles à l’évaluation de l’avantage thérapeutique.
Résultats
Le CSP s’est avéré une combinaison simple mais efficace de paramètres qui permet d’obtenir la proportion de patients ayant bénéficié du traitement sans avoir subi des effets secondaires importants.
Conclusion
Le CSP peut être un pas en avant vers la création d’un outil composite de l’évaluation des traitements du psoriasis.



Similar content being viewed by others
References:
Gottlieb AB. Psoriasis. Dis Manag Clin Outcomes 1998; 1(6):195–202
Rapp SR, Feldman SR, Exum ML, et al. Psoriasis causes as much disability as other major medical diseases. J Am Acad Dermatol 1999; 41(3 Pt 1):401–407
Jacobson CC, Kimball AB. Rethinking the psoriasis area and severity index: the impact of area should be increased. Br J Dermatol 2004; 151:381–387
Carlin CS, Feldman SR, Krueger JG, et al. A 50% reduction in the Psoriasis Area and Severity Index (PASI 50) is a clinically significant endpoint in the assessment of psoriasis. J Am Acad Dermatol 2004; 50(6):859–866
de Arruda LHF, De Moraes APF. The impact of psoriasis on quality of life. Br J Dermatol 2001; 144 (Suppl 58):33–36
Kirby B, Richards HL, Woo P, et al. Physical and psychologic measures are necessary to assess overall psoriasis severity. J Am Acad Dermatol 2001; 45(1):72–76
Koo J, Menter A. The Koo–Menter psoriasis instrument for identifying candidate patients for systemic therapy. In: Poster presented at the 9th International Psoriasis Symposium, New York, June 18–22, 2003
Al Suwaidan SN, Feldman SR. Clearance is not a realistic expectation of psoriasis treatment. J Am Acad Dermatol 2000; 42(5 Pt 1):796–802
Griffiths CEM, Sterry W, Henninger E. Safe control of psoriasis: evaluation of a new approach to assessing efficacy of psoriasis treatments. JEADV 2004; 18(suppl.2):355 (Ref. P06.106)
Fredriksson T, Pettersson U. Severe psoriasis—oral therapy with a new retinoid. Dermatologica 1978; 157:238–244
Finlay AY, Khan GK. Dermatology life quality index (DLQI)—a simple practical measure for routine clinical use. Clin Exp Dermatol 1994; 19(3):210–216
Juniper EF, Guyatt GH, Willan A, et al. Determining a minimal important change in a disease-specific quality of life questionnaire. J Clin Epidemiol 1994; 47:81–87
Kazis LE, Anderson JJ, Meenan RF. Effect sizes for interpreting changes in Health Status. Med Care 1989; 27:3
Cohen J. Statistical power analysis for the behavioural sciences. Hillsdale, NJ, Lawrence Earlbaum, 1988
Kirby B, Fortune DG, Bhushan M, et al. The salford psoriasis index: an holistic measure of psoriasis severity. Br J Dermatol 2000; 142:728–732
Zachariae R, Zachariae H, blomqvist K, et al. Quality of life in 6,497 Nordic patients with psoriasis. Br J Dermatol 2002; 146:1006–1016
Note for Guidance on Clinical Investigation of Medicinal Products indicated for the Treatment of Psoriasis. Draft published by EMEA/CPMP on 20 November 2003
Mckenna KE, Stern RS. The outcomes movement and new measures of the severity of psoriasis. J Am Acad Dermatol 1996; 34(3):534–538
Touw CR, Hakkaart-Van Roijen L, Verboom P, et al. Quality of life and clinical outcome in psoriasis patients using intermittent cyclosporin. Br J Dermatol 2001; 144(5):967–972
Krueger GG, Feldman SR, Camisa C, et al. Two considerations for patients with psoriasis and their clinicians: what defines mild, moderate, and severe psoriasis? What constitutes a clinically significant improvement when treating psoriasis? J Am Acad Dermatol 2000; 43(2 Pt 1):281–285
Bateman ED, Bousquet J, Braunstein GL. Is overall asthma control being achieved? A hypothesis-generating study. Eur Respir J 2001; 17:589–595
Bateman ED, Frith LF, Braunstein GL. Achieving guideline-based asthma control: does the patient benefit? Eur Respir J 2001; 20:588–595
Griffiths CEM, Sterry W, Henninger E. Safe control of psoriasis: evaluation of a new approach to assessing efficacy of psoriasis treatments. JEADV 2004; 18(suppl. 2):355 (Ref. P06.106)
Author information
Authors and Affiliations
Additional information
Conflicts of Interest:
Kim Papp has acted as a consultant to Serono
Eric Henninger is an employee of Serono
This material was presented as a poster during the EADV 2004 convention
About this article
Cite this article
Papp, K.A., Henninger, E. Safe Psoriasis Control: A New Outcome Measure for the Composite Assessment of the Efficacy and Safety of Psoriasis Treatment. J Cutan Med Surg 9, 276–283 (2005). https://doi.org/10.1007/s10227-005-0121-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10227-005-0121-4