Abstract
Aim
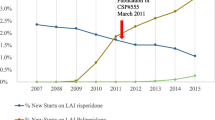
To estimate changes in resource usage, hospitalization rates, and costs in actual practice in Sweden for schizophrenia patients after switching to long-acting injectable risperidone (Risperdal Consta).
Methods
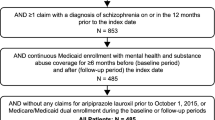
A retrospective chart review within-subject mirror-image study using actual practice chart review data was used to compare annual hospital bed-days and annual hospital episodes for adults with schizophrenia or schizoaffective disorder before and after switching to Risperdal Consta in the period 1 January 2003 to 30 June 2005. Secondary endpoints included mean length of hospital stay per episode, the cost of hospitalization, and the cost of antipsychotic treatment. The base case analytical approach allocated all hospital episodes overlapping the switch date entirely to pre-switch treatment. In order to investigate the impact of inpatient care ongoing at the time of the switch, the change in bed-days per year was also estimated using an alternative analytical approach inspired by economic modelling.
Results
One-hundred sixty-four patients were enrolled at nine geographically diverse sites. The switch to Risperdal Consta was associated with a significant reduction in mean annual days in hospital from 39 to 21 days per year (45%), which was linked to a significant reduction in the number of hospitalizations from 0.86 to 0.63 per year (27%). The alternative “modelling-inspired” estimate of the reduction in mean annual days in hospital was also 27%.
Conclusion
A naturalistic mirror-image study found that switching to long-acting injectable risperidone led to sizeable reductions in inpatient resource use. These results coincide with the findings of other international studies.

Similar content being viewed by others
Notes
Note: this reflects a protocol amendment changing the earliest allowable start date from 1 January 2004 to 1 January 2003. The amended study inclusion period covered 16 months prior to the official launch and reimbursement approval for Risperdal Consta in Sweden and 14 months following launch until the end of the inclusion period.
A protocol amendment affecting three study subjects altered the way in which antipsychotic medication could be collected. For affected subjects, the medical prescription history prior to the switch to Risperdal Consta was collected in full detail only for the 3 months immediately preceding the switch (rather than the full 2 years) with the remainder of the 2-year pre-switch period being recorded at fixed 3-month intervals.
Ordinary psychiatric hospital care costs were 4,442 SEK (€474) per bed-day in Lund, for example, and 3,415 SEK (€365) in Västra Götaland [7].
A per protocol approach was also undertaken in order to provide additional perspective. The results were qualitatively similar, though more favourable to Risperdal Consta, than the base case results presented here.
Risperdal Consta reaches satisfactory blood serum levels first after 3 weeks, until which time additional antipsychotic treatment is required to maintain adequate control [8].
“At risk” exposure for the post-switch period was adjusted to reflect the discharge date in patients in whom a hospitalization overlapped the index switch date.
Only two patients had no recorded antipsychotic treatment over the entire 2 years prior to initiation of Risperdal Consta. “Untreated” should not be confused with drug-naive even in these two patients, however, as they may have been treated prior to the study or they may have taken antipsychotic drugs not recorded in the charts or other nonantipsychotic drugs to control their schizophrenia at the time of the switch. Patients classified as “untreated” at the time of the switch were slightly older (47.64 vs. 44.02 years) and had slightly longer disease duration (18.16 vs. 15.80 years).
References
Regier, D.A., Narrow, W.E., Rae, D.S., Manderscheid, R.W., Locke, B.Z., Goodwin, F.K.: The de facto mental and addictive disorders service system. Epidemiologic catchment area prospective 1-year prevalence rates of disorders and services. Arch. Gen. Psychiatry 50, 85–94 (1993)
Niaz, O., Haddad, P.: Thirty-five months experience of risperidone long-acting injection in a UK psychiatric service including a mirror-image analysis of in-patient care. Acta Psychiatr. Scand. 116, 36–46 (2007)
Fuller, M., Shermock, K., Secic, M., Engelhart, L., Vallow, S., Flanders, S.: Hospitalization and resource utilization in schizophrenia following initiation of risperidone long-acting injection in the Veterans Affairs Healthcare System (VISN 10). Presented at the Collegium Internationale Neuro-psychopharmacolegium 25th Biennial Congress, Chicago, Illinois, 9–13 July 2006
Eriksson, L., Almqvist, A., Mehnert, A., Ingham, M., Eriksson, B.: Reduction in need for institutional care in chronic schizophrenia subjects switched to long-acting risperidone. Presented at the 42nd Annual Meeting of the American College of Neuropsychopharmacology, San Juan, Puerto Rico, 7–11 December 2003
Eriksson, L., Almqvist, A., Mehnert, A., Ingham, M., Eriksson, B.: Treatment with long acting risperidone significantly reduces the need for institutional psychiatric care regardless of previous treatment. Presented at the 45th Annual and 4th Mediterranean Meeting of the Scandinavian College of Neuro-psychopharmacology, Juan-les-Pins, France, 21–24 April 2004
Södra Regionsvårdsnämnden. 2006 price list for the University Hospital in Malmö, Region Skåne (2006)
Samverkansnämnden Västra Sjukvårdsregionen. Utomlänspriser 2006 För vårdtjänster enligt samverkansavtal om hälso-och sjukvård inom Västra sjukvårdsregionen. Västra Götalandsregionen (2006)
FASS (Swedish Drug Price List), The Swedish Association of the Pharmaceutical Industry (2006)
Taylor, A., Currie, A., Lloyd, K., Price, M., Peperell, K.: Impact of risperidone long acting injection on resource utilization in psychiatric secondary care. J. Psychopharmacol. 22, 128–131 (2008)
Gianfrancesco, F., Wang, R.-H., Mahmoud, R., White, R.: Methods for claims-based pharmacoeconomic studies in psychosis. Pharmacoeconomics 20, 499–511 (2002)
Acknowledgments
The authors wish to thank Maria Kastenholm for monitoring the study; Christian Asseburg at The Swedish Institute for Health Economics for invaluable assistance; Janssen-Cilag, Sweden for finance and data collection; and Dorin Borota, Cecilia Brain, Ludvig Elfwén, Kalle Forsman, Martin Fransson, Iris Förstberg, Ola Gefvert, Lars Gidlund, Siv Gustavsson, Per Hagström, Marie Hansson, Yvonne Holm, Lotta Ibstedt Farde, Magnus Malm, Deanne Mannelid, Hannele Mered, Urban Norén, Britt-Marie Hansson, Maivor Olsson, Hans Olsson, Natalja Shulman, Catharina Sigalin, Olof Strandell, and Gunnel Stråmo for participation at the sites. We also express our gratitude to the editor and to two anonymous reviewers for invaluable comments.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Willis, M., Svensson, M., Löthgren, M. et al. The impact on schizophrenia-related hospital utilization and costs of switching to long-acting risperidone injections in Sweden. Eur J Health Econ 11, 585–594 (2010). https://doi.org/10.1007/s10198-009-0215-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10198-009-0215-9