Abstract
Background
The UK hip fracture best practice tariff (BPT) aims to deliver hip fracture surgery within 36 h of admission. Ensuring that delays are reserved for conditions which compromise survival, but are responsive to medical optimisation, would help to achieve this target. We aimed to identify medical risk factors of surgical delay, and assess their impact on mortality.
Materials and methods
Prospectively collected patient data was obtained from the National Hip Fracture Database (NHFD). Medical determinants of surgical delay were identified and analysed using a multivariate regression analysis. The mortality risk associated with each factor contributing to surgical delay was then calculated.
Results
A total 1361 patients underwent hip fracture surgery, of which 537 patients (39.5 %) received surgery within 36 h of admission. Following multivariate analyses, only hyponatraemia was deduced to be a significant risk factor for delay RR = 1.24 (95 % CI 1.06–1.44). However, following a validated propensity score matching process, a Pearson chi-square test failed to demonstrate a statistical difference in mortality incidence between the hypo- and normonatraemic patients [χ 2(1, N = 512) = 0.10, p = 0.757].
Conclusions
Hip fracture surgery should not be delayed in the presence of non-severe and isolated hyponatraemia. Instead, surgical delay may only be warranted in the presence of medical conditions which contribute to mortality and are optimisable.
Level of evidence
III
Similar content being viewed by others
Introduction
A fracture of the hip is the commonest cause of injury-related death in the UK [1]. Prompt surgery has been associated with higher rates of independent living and lower 30-day and 1-year mortality rates [2–5]. Earlier surgery has also been shown to improve patient outcomes by reducing pain scores, and lowering of the risk of decubitus ulcer formation and length of inpatient stay [2, 6, 7].
The inception of best practice tariffs (BPTs), which aimed to improve these patient outcomes, stemmed from the ‘Equity and Excellence: liberating the NHS’ government white paper [8]. BPTs are incentivised targets, which financially compensate organisations for delivering high quality care. In the context of hip fracture management, the BPT consists of an initial base tariff, with additional payments if further criteria of best practice have been met. One of these criteria is delivering hip fracture surgery within 36 h of presentation to a health care institution. This government target is also in accordance with clinical guidelines set by the British Orthopaedic Association (BOA) and National Institute of Clinical Excellence (NICE), which state that hip fracture surgery should be performed on the day of, or the day after admission and within normal working hours [9, 10]. However, the National Hip Fracture Database (NHFD) has reported that this specific BPT target was met in only 71.4 % of hip fracture patients, equating to £15.9 million in ‘lost’ monetary incentives [1].
Clearly, resources must be made available to allow such a level of service provision and to qualify for the maximum financial reward the BPT has to offer. Optimal clinical decision-making could therefore augment and streamline management in order to facilitate early surgery. As survival is perhaps the most desirable outcome following a fracture of the neck of femur (FNOF), and delay to surgery in itself carries an increased risk to mortality, then it certainly follows that delays for medical optimisation would only be justified for conditions which also carry a mortality risk [3–7]. Therefore, identifying medical risk factors for surgical delay and their associated mortality risk would assist organisations to rationalise clinical decision-making, and thus enhance compliance with the BPT target.
The primary aim of this study was therefore to identify medical conditions associated with patients failing to achieve the 36-h cut-off for surgery following a hip fracture. We subsequently evaluated whether these factors were justifiable in risking surgical delay by gauging whether they were also associated with an increased risk to mortality.
Materials and methods
We obtained prospectively collected hip fracture patient information from the UK NHFD from before April 2010 and prior to the inception of the 36-h BPT guideline. Data was subsequently cross-referenced with our institution’s patient records. The use of data after the introduction of the BPT guidelines may have risked missing patients with legitimate causes of delay, who may have had their surgery expedited to meet the 36-h target. Hence analysis of delays was performed on data pre-dating the BPT introduction, allowing all medical causes of delays to be identified and an assessment of their risk to mortality to be performed.
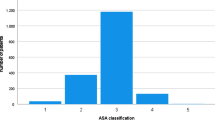
We collected patient-level information including demographic data, American Society of Anesthesiologists (ASA) grade at the time of surgery, fracture type, source of admission and walking ability [11]. All patient co-morbidity data was identified using the International Classification of Disease 10th revision (ICD-10) codes, and these were used to calculate the Charlson co-morbidity index for each patient as a separate variable [12]. Biochemical parameters collected included admission haemoglobin levels (Hb), white cell count (WCC), coagulation profile, urea and electrolyte levels. Time to surgery from presentation was also collected.
The primary outcome of interest was a delay to surgery over 36 h from initial hospital presentation. The secondary outcome examined was the occurrence and causes of mortality within 30 days of admission. Primary and secondary causes of death were noted from death certificates and hospital death records. A total of 1674 patients were initially identified, but following exclusions of incomplete data sets and incorrect or duplicate entries, a total of 1361 patients were included in the study.
Statistical analysis was undertaken in a two-stage process. We initially categorised patients into two groups: group1 = time to surgery <36 h; group 2 = time to surgery >36 h). All variables collected were then compared between these two groups on initial univariate analysis using the chi-square or Fisher’s exact test for categorical data and the independent t/Mann–Whitney test for continuous variables. A subsequent backward stepwise Cox regression model was undertaken to identify the most significant determinants of surgical delay beyond 36 h. Our criteria for inclusion of variables into the model included a p value <0.15 on univariate analysis, in accordance with published statistical methods [13]. Results were displayed as relative risks rather than odds ratios, in order to aid clinical interpretation [14].
The decision to delay hip fracture surgery on medical grounds is undertaken to avoid significant complications which may result from precipitous surgery. Death is perhaps the most important complication to avoid. Therefore, it is logical to validate variables that risk a delay to surgery beyond 36 h in terms of their impact on mortality. We undertook a second-stage analysis to assess mortality likelihood at 30 days following surgery for each individual variable which had been found to delay surgery. To limit potential for selection bias, when assessing one variable’s association with mortality we had to control for all other variables. We therefore derived a single scalar propensity score from the regression of all remaining covariates in Tables 1 and 2. Between-group propensity score matching was performed using a “nearest neighbour” matching strategy [15]. An assessment of the matching process consisted of an evaluation of between-group standardised mean differences and variance ratios according to published standards [16]. Between-group mortality analysis used a chi-square test for each variable influencing surgical delay only after the matching process had been verified as being successful in balancing covariates between the two groups.
Results
A total 1361 patients underwent hip fracture surgery, of which 537 patients (39.5 %) received surgery within 36 h of admission. The overall median time to surgery from presentation was 23 h (3–36) in group 1 and 72 h (36–774) in group 2. The demographics were similar between patients who did (group 1) and those who did not (group 2) receive timely surgery (Table 1). There was no difference between the two groups with respect to age, gender, walking ability, fracture pattern and ASA grade. However, with regards to admission source, there was a higher proportion of patients presenting from a community care institution in group 1, whilst a higher proportion of patients were from their own home in group 2 (p = 0.013).
The distribution of the different co-morbidities between the two groups are summarised in Table 2. There was a higher proportion of patients with cardiac co-morbidities in group 1, while a higher proportion of patients in group 2 presented with hyponatraemia (sodium <135 mmol/l) (p = 0.00). There was no difference between the two groups with respect to a number of factors, including pre-existing anticoagulation therapy (p = 0.303). Furthermore, the calculated Charlson’s co-morbidity index was also similar between the two groups (p = 0.835). There was no statistical difference in haematological and serum biochemical parameters between the two groups (Table 2).
Following univariate analysis, seven variables, including admission source, history of dementia, ischaemic heart disease, MI, cerebrovascular accidents (CVA), urinary tract infections and hyponatraemia met criteria for inclusion into the Cox regression model. The model thereafter inferred only hyponatraemia to be a significant risk factor for delay to surgery beyond 36 h with a covariate adjusted relative risk (RR) 1.24 (95 % CI 1.06–1.44, p = 0.006).
The overall 30-day mortality in our cohort of hip fracture patients was 9.0 %. The commonest cause of death was from pneumonia (37 %). Following propensity score analysis, 256 patients with hyponatraemia were matched to 256 patients with normal sodium levels. The absolute acceptable propensity score caliper width was 0.01. A near perfect standardised mean difference of 0.0003 and a variance ratio of 1 (0.01:0.01) confirmed between-group homogeneity to be well within acceptable limits [16]. Thus, the matching process controlled for all collected variables, including time to surgery. The 30-day mortality rates for hyponatraemic patients was 10 % (24/256) and 9 % (22/256) for normonatraemic patients. This was not statistically significant (p = 0.757).
Discussion
Our study has shown that 60.5 % of patients had surgery delayed beyond 36 h. Furthermore, hyponatraemia was identified as a pre-operative risk factor for this. Interestingly, the impact of hyponatraemia on 30-day mortality was not significant.
Nationally, the reason for 37.9 % of patients failing to meet the UK hip fracture BPT target was because of a perceived need for medical optimisation [17]. At first glance the rates of delay in our study may seem high. This was because data collection predated the NICE guidelines for time to surgery. We realised that the guidelines could have modified clinical practice owing to the need for expediting surgery within 36 h. Hence, potential medical causes for delay that would have otherwise been apparent prior to the guidelines would potentially be missed following its introduction. Thus, pre-guideline data were used in an effort to prevent this potential bias.
The median age in both groups of our cohort was above 80 years with a higher proportion of females. This is in agreement with demographic information published by the NHFD [18]. With respect to admission source, we found that a comparatively higher proportion of patients admitted from their own home with a hip fracture were delayed beyond 36 h. Conversely, a higher proportion of patients admitted from a community care institution were seen in the timely surgery group. It is entirely possible that clinical practice may have inherently favoured expedited treatment owing to fears of complications of delayed surgery in patients who were perceived to be frailer. Such patients are more likely to present from a community care institution than their own home [19, 20]. This is also reflected by the comparatively higher proportion of cardiac related co-morbidities in the early surgery group.
This study found that the mean international normalised ratio (INR) and ranges between the two groups were similar. This is because patients with comparatively higher INRs in group 1 had been aggressively treated to correct the values within the 36-h time frame by using, according to our institution’s formalised protocol, vitamin k therapy. This practice is supported by Gleeson et al. who demonstrated in their cohort of 1080 patients, that an active management strategy for the reversal of warfarin anticoagulation facilitated earlier surgery without increasing complications of thromboembolic events, mortality or 30-day re-admission [21]. Equally, it follows that patients in group 2 with comparatively normal INRs were delayed for other reasons.
We found hyponatraemia to be comparatively more common in the delayed surgery cohort. While we did not formally explore the underlying reasons for this, anecdotally we believe that hyponatraemia was perceived to be associated with peri-operative mortality and morbidity. The association between hyponatraemia and mortality has been demonstrated previously [22]. However, it has also been suggested that severe underlying disease is the cause of death while hyponatraemia is merely another complication of this underlying disease. Hence, while it shows an association, it does not necessarily prove causality. Chawla et al. in their study of just over 45,000 patients found that mortality rates tended to increase as sodium levels changed from normal to mild hyponatraemia. Surprisingly, as hyponatraemia became more severe (sodium <120 mmol/l) mortality trends reversed [23]. Furthermore, over the 12 years of their study, only three deaths were directly attributable to adverse hyponatraemia sequelae. Our study also found no difference in mortality incidence between hypo- and normonatraemic patients after matching groups for confounders, such as liver and renal failure, which may have contributed to both mortality and hyponatraemia. This supports the notion that hyponatraemia may not necessarily be singularly causal to mortality. Subgroup analysis of those with severe hyponatraemia (sodium <120 mmol/l) was unfortunately precluded because there were only three patients that fell into this category. We cannot therefore draw conclusions as to whether severe hyponatraemia is a risk factor to mortality and whether it is reasonable to delay surgery in its presence.
Interestingly, we found that patients with a history of ischaemic heart disease were significantly less likely to have their surgery delayed beyond 36 h (23.6 versus 30 %, p = 0.01). Patients with a history of myocardial infarction also were significantly less likely to have delayed surgery (4.1 versus 2.1 %, p = 0.03). These patients may have been prioritised as these risk factors are non-modifiable and clinical opinion may have been not to increase their risk further by also having delayed surgery. Similarly, there is an increased awareness of the need to avoid unnecessary delays in order to gain financial compensation for services used in treating such patients, and to avoid increased costs associated with longer hospital stays in these patients [24, 25].
The main weakness of this study lies in the fact that we present data pertaining to only one major trauma unit. One may argue that patient data from other units may yield differing results. However, our findings may be more widely generalisable as our patient population demographics and mortality rates of 9.0 % (n = 123/1361) at 30 days were comparable to other published studies and NHFD reports [18, 26, 27]. Although retrospective by design, we cross-referenced prospectively collected data from multiple sources, including a national hip fracture registry and our own hospital-coding database, ensuring that the final dataset was reliable. Non-medical risk factors for delay are not available in the NHFD or medical notes and hence our regression model is limited by their absence. We have, however, made a comprehensive assessment of 38 medical and demographic variables. These variables are readily available on initial presentation and are thus easily collectable by other units who also wish to make similar assessments of their services.
This type of study is relevant in the current NHS culture of target-driven quality health care delivery. Verifying and investigating the legitimacy of medical causes of surgical delay is therefore not only pertinent, but has also been specifically highlighted as a vital area for future research by the NHFD Scientific Committee [9]. To our knowledge this study is unique in assessing the risk factors to delay in achieving the 36-h BPT target in these patients. Nationally, delays are also due to a lack of theatre time, equipment or high dependency beds (43 % of the time) [17]. Therefore, whilst streamlining medical decision-making may help improve the likelihood of attaining the BPT, availability of clinical resources plays an important part.
In conclusion, surgical delays can result when one aims to avoid medical complications associated with hastened hip fracture surgery. However, delay is not justifiable in the presence of non-severe and isolated hyponatraemia. Instead, surgical delay should only be warranted in the presence of medical conditions which contribute to mortality and are optimisable.
References
Royal College of Physicians (2013) National Hip Fracture Database national report. http://www.nhfd.co.uk/20/hipfractureR.nsf/0/CA920122A244F2ED802579C900553993/$file/NHFDReport2013.pdf. Accessed 20 Mar 2015
Al-Ani AN, Samuelsson B, Tidermark J, Norling A, Ekstrom W, Cederholm T, Hedstrom M (2008) Early operation on patients with a hip fracture improved the ability to return to independent living. A prospective study of 850 patients. J Bone Jt Surg Am 90(7):1436–1442. doi:10.2106/JBJS.G.00890
McGuire KJ, Bernstein J, Polsky D, Silber JH (2004) The 2004 Marshall Urist award: delays until surgery after hip fracture increases mortality. Clin Orthop Relat Res 428:294–301
Shiga T, Wajima Z, Ohe Y (2008) Is operative delay associated with increased mortality of hip fracture patients? Systematic review, meta-analysis, and meta-regression. Can J Anaesth 55(3):146–154. doi:10.1007/BF03016088
Weller I, Wai EK, Jaglal S, Kreder HJ (2005) The effect of hospital type and surgical delay on mortality after surgery for hip fracture. J Bone Jt Surg Br 87(3):361–366
Grimes JP, Gregory PM, Noveck H, Butler MS, Carson JL (2002) The effects of time-to-surgery on mortality and morbidity in patients following hip fracture. Am J Med 112(9):702–709
Orosz GM, Magaziner J, Hannan EL, Morrison RS, Koval K, Gilbert M, McLaughlin M, Halm EA, Wang JJ, Litke A, Silberzweig SB, Siu AL (2004) Association of timing of surgery for hip fracture and patient outcomes. JAMA, J Am Med Assoc 291(14):1738–1743. doi:10.1001/jama.291.14.1738
Department of Health (2010) Equity and excellence: liberating the NHS. http://www.gov.uk/government/uploads/system/uploads/attachment_data/file/213823/dh_117794.pdf. Accessed 20 Mar 2015
NICE clinical guideline 124 (June 2011). The management of hip fractures in adults. Modified March 2014. http://www.nice.org.uk/guidance/cg124. Accessed 22 Nov 2014
British Orthopaedic Association (2012) BOAST 1 guideline version 2—patients sustaining a fragility hip fracture. http://www.boa.ac.uk/publications/boa-standards-for-trauma-boasts/#toggle-id-1. Accessed 22 Nov 2014
Association of Anaesthetists of Great Britain and Ireland safety guideline (2010) Management of proximal femoral fractures. http://www.aagbi.org/sites/default/files/femoralfractures2012_0pdf. Accessed 20 Aug 2014
Charlson ME, Pompei P, Ales KL, MacKenzie CR (1987) A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis 40(5):373–383
Bursac Z, Gauss CH, Williams DK, Hosmer DW (2008) Purposeful selection of variables in logistic regression. Source Code Biol Med 3:17. doi:10.1186/1751-0473-3-17
McNutt LA, Wu C, Xue X, Hafner JP (2003) Estimating the relative risk in cohort studies and clinical trials of common outcomes. Am J Epidemiol 157(10):940–943
Stuart EA (2010) Matching methods for causal inference: a review and a look forward. Statist Sci: Rev J Inst Math Statist 25(1):1–21. doi:10.1214/09-STS313
Rubin DB (2007) The design versus the analysis of observational studies for causal effects: parallels with the design of randomized trials. Stat Med 26(1):20–36. doi:10.1002/sim.2739
Royal College of Physicians (2011) National Hip Fracture Database annual report. http://www.nhfd.co.uk/003/hipfracturer.nsf/NHFDNationalReport2011_Final.pdf. Accessed 20 Mar 2015
Royal College of Physicians (2014) National Hip Fracture Database annual report. http://www.nhfd.co.uk/20/hipfractureR.nsf/welcome?readform. Accessed 20 Mar 2015
Beaupre LA, Cinats JG, Jones CA, Scharfenberger AV, William CJD, Senthilselvan A, Saunders LD (2007) Does functional recovery in elderly hip fracture patients differ between patients admitted from long-term care and the community? J Gerontol Ser A Biol Sci Med Sci 62(10):1127–1133
Eastwood EA, Magaziner J, Wang J, Silberzweig SB, Hannan EL, Strauss E, Siu AL (2002) Patients with hip fracture: subgroups and their outcomes. J Am Geriatr Soc 50(7):1240–1249
Gleason LJ, Mendelson DA, Kates SL, Friedman SM (2014) Anticoagulation management in individuals with hip fracture. J Am Geriatr Soc 62(1):159–164. doi:10.1111/jgs.12591
Mc Causland FR, Wright J, Waikar SS (2014) Association of serum sodium with morbidity and mortality in hospitalized patients undergoing major orthopedic surgery. J Hosp Med 9(5):297–302. doi:10.1002/jhm.2168
Chawla A, Sterns RH, Nigwekar SU, Cappuccio JD (2011) Mortality and serum sodium: do patients die from or with hyponatremia? Clin J Am Soc Nephrol 6(5):960–965. doi:10.2215/CJN.10101110
Kosy JD, Blackshaw R, Swart M, Fordyce A, Lofthouse RA (2013) Fractured neck of femur patient care improved by simulated fast-track system. J Orthop Traumatol 14(3):165–170. doi:10.1007/s10195-013-0240-4
Johnson DJ, Greenberg SE, Sathiyakumar V, Thakore R, Ehrenfeld JM, Obremskey WT, Sethi MK (2015) Relationship between the Charlson comorbidity index and cost of treating hip fractures: implications for bundled payment. J Orthop Traumatol 16(3):209–213. doi:10.1007/s10195-015-0337-z
Tarrant SM, Hardy BM, Byth PL, Brown TL, Attia J, Balogh ZJ (2014) Preventable mortality in geriatric hip fracture inpatients. Bone Jt J 96-B(9):1178–1184. doi:10.1302/0301-620X.96B9.32814
Haleem S, Lutchman L, Mayahi R, Grice JE, Parker MJ (2008) Mortality following hip fracture: trends and geographical variations over the last 40 years. Injury 39(10):1157–1163. doi:10.1016/j.injury.2008.03.022
Acknowledgments
The authors would like to thank the Orthopaedic Network, UK for their help in this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical standards
Obtaining informed consent from involved patients was waived by our Institutional Review Board for this retrospective study. All procedures involving human participants were in accordance with the 1964 Helsinki Declaration and its later amendments. Ethical approval was waived by our institutional review board as it involved retrospective patient data which evaluated service provision. This study was therefore in accordance with regulations from the National Patient Safety Agency.
Conflict of interest
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Aqil, A., Hossain, F., Sheikh, H. et al. Achieving hip fracture surgery within 36 hours: an investigation of risk factors to surgical delay and recommendations for practice. J Orthopaed Traumatol 17, 207–213 (2016). https://doi.org/10.1007/s10195-015-0387-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10195-015-0387-2