Abstract
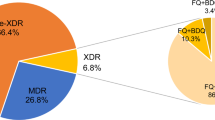
Emergence of extensively drug-resistant (XDR) tuberculosis (TB) in Bangladesh has increased as a result of the inadequate management of TB-infected individuals. The present study attempted to detect the frequency of multidrug resistance (MDR) among the TB patients categorically from relapse, category I failure, category II failure, and return after default category I and II cases, using the conventional drug susceptibility test. Among 100 sputum specimens from all four categories, 81 and 84 positive cases were identified under light-emitting diode fluorescence microscope and the Lowenstein–Jensen (L-J) culture method, respectively. Of 84 culture-positive cases, elevated resistance was observed against isoniazid (89.3 %) and rifampicin (91.7 %) compared to that against streptomycin (53.6 %) and ethambutol (47.7 %). Resistance against ofloxacin, gatifloxacin, and kanamycin was 8.3, 5.9, and 2.4 %, consecutively. Fifty-nine cases were found to be MDR-TB. Two of these cases, which showed resistance against kanamycin and ofloxacin, were further identified as XDR. The proportion of XDR cases was more likely to be in the return after default category I and II cases.
Similar content being viewed by others
References
Kumar V, Abbas AK, Fausto N, Mitchell RN, editors. Robbins basic pathology. 8th ed. Philadelphia: Saunders Elsevier; 2007. p. 516–522.
McAdam AJ, Sharpe AH. Mycobacteria. In: Robbins and Cotran pathologic basis of disease. 7th ed. Philadelphia: Saunders. 2004; p. 381–387.
Lutfor AB. Extensively-drug resistant tuberculosis (XDR-TB). Bangladesh J Med Microbiol. 2009;03:1–3.
Rahman F, Munshi SK, Kamal SMM, Rahman ASMM, Rahman MM, Noor R. Comparison of different microscopic methods with conventional TB culture. Stamford J Microbiol. 2011;1:46–50.
Salim AH, Aung KJM, Hossain MA, Van Deun A. Early and rapid microscopy-based diagnosis of true treatment failure and MDR-TB. Int J Tuberc Lung Dis. 2006;10:1248–554.
Parvez MKN, Hasan M, Rumi S, Ahmed M, Salimullah Y, Tahera DJ, et al. PCR can help early diagnosis of pulmonary tuberculosis. Southeast Asian J Trop Med Public Health. 2003;34:147–53.
Kamal SMM, Ahsan HM, Ahmed S, Ayaz K, Mahbub KS, Khan MAI, et al. Isolation and Identification of Mycobacterium from extra-pulmonary specimens at NTRL, NIDCH. J Med Microbiol. 2010;11:128–30.
Zaman K, Rahim Z, Yunus M, Arifeen SE, Baqui AH, Sack DA, et al. Drug resistance of Mycobacterium tuberculosis in selected urban and rural areas in Bangladesh. Scand J Infect Dis. 2005;37:21–6.
Mahmud AM, Rahman M, Hassan MR, Hossain MA, Islam MR, Kamal SMM, et al. Multidrug resistant TB (MDR-TB) and DOTS-plus project in Bangladesh. Respirology. 2008;13:106.
WHO. Global tuberculosis control: surveillance, planning, financing. Geneva, Switzerland: WHO; 2006.
Sharma SK, Kumar S, Saha PK, George N, Arora SK, Gupta D, et al. Prevalence of multidrug-resistant tuberculosis among Category II pulmonary tuberculosis patients. Indian J Med Res. 2011;133:312–5.
WHO. Multidrug and extensively drug-resistant TB (M/XDR-TB): 2010 global report on surveillance and response. Geneva: World Health Organization; 2010, p. 18.
Banerjee R, Schecter GF, Flood J, Porco TC. Extensively drug resistant tuberculosis: new strains, new challenges. Expert Rev Anti Infect Ther. 2008;6:713–24.
Zapata P, Arbeloa M, Aznar J. Evaluation of mycobacteria growth indicator tube (MGIT) for drug susceptibility testing of Mycobacterium tuberculosis isolates from clinical specimens. Clin Microbiol Infect. 1999;5:227–30.
Kamal M, Jewel A, Shamim H. Standard Operating Procedure (SOP) for Culture and DST of Mycobacteria. 1st ed. Bangladesh: National TB Control Program (NTP), Director General of Health Services (DGHS), Ministry of Health and Family Welfare; 2009.
Shiferaw G, Woldeamanuel Y, Gebevehu M, Girmachew F, Demessie D, Lemma E. Evaluation of microscopic observation drug susceptibility assay for detection of multidrug-resistant Mycobacterium tuberculosis. J Clin Microbiol. 2007;45:1093–7.
Mahadev B, Srikantaramu N, James P, Mathew PG, Bhagirathi R. Comparison between rapid colorimetric mycobacterial isolation and susceptibility testing method and conventional method using LJ medium. Indian J Tuberc. 2001;48:129.
Iqbal R, Shabbir I, Khan SU, Saleem S, Munir K. Multidrug resistance tuberculosis in Lahore. Pak J Med Res. 2008;47:1.
Sabouni R, Kourout M, Chaoui I, Jordaan A, Akrim M, Victor TC, et al. Molecular analysis of multidrug resistant Mycobacterium tuberculosis isolates from Morocco. Ann Microbiol 2008;58:749–754.
Jou R, Chen H, Chiang C, Yu M, Su I. Genetic diversity of multidrug-resistant Mycobacterium tuberculosis isolates and identification of 11 novel rpoB alleles in Taiwan. J Clin Microbiol. 2005;43:1390–4.
Bengisun JS, Karnak D, Palabiyikoglu I, Saygun N. Mycobacterium tuberculosis drug resistance in Turkey, 1976–97. Scand J Infect Dis. 2000;32:507–10.
World Health Organization. Tuberculosis profile- Bangladesh (high TB burden; high MDR-TB burden), 2010. Available at: http://www.who.int/tb/country/data/profiles/en/index.html.
Gandhi NR, Moll A, Sturm AW, Pawinski R, Govender T, Lalloo U, et al. Extensively drug resistant tuberculosis as a cause of death in patients co-infected with tuberculosis and HIV in a rural area of South Africa. Lancet. 2006;368:1575–80.
World Health Organization. Global tuberculosis control: epidemiology, strategy, financing: report 2009. Publication no. WHO/HTM/TB/2009.411. Geneva: World Health Organization; 2009; p. 8–9.
Wallengren K, Scano F, Nunn P, Margot B, Buthelezi SSS, Williams B, et al. Drug-resistant tuberculosis, KwaZulu-Natal, South Africa, 2001–2007. Emerg Infect Dis. 2011;17:1913–6.
Zhao Y, Xu S, Wang L, Chin DP, Wang S, Jiang, et al. National survey of drug-resistant tuberculosis in China. N Engl J Med. 2012;366:2161–70.
Jugheli L, Bzekalava N, de Rijk P, Fissette K, Portaels F, Rigouts L. High level of cross-resistance between kanamycin, amikacin, and capreomycin among Mycobacterium tuberculosis isolates from Georgia and a close relation with mutations in the rrs gene. Antimicrob Agents Chemother. 2009;53:5064–8.
Maus CE, Pikaytis BB, Shinnick TM. Molecular analysis of cross-resistance to capreomycin, kanamycin, amikacin, and viomycin in Mycobacterium tuberculosis. Antimicrob Agents Chemother. 2005;49(8):3192–7.
Hwang SS, Kim HR, Kim HJ, Kim MJ, Lee SM, Yoo CG, et al. Impact of resistance to first-line and injectable drugs on treatment outcomes in MDR-TB. Eur Respir J. 2009;33:581–5.
Jeon CY, Hwang SH, Min JH, Prevots DR, Goldfeder LC, Lee H, et al. Extensively drug resistant tuberculosis in South Korea: risk factors and treatment outcomes among patients at a tertiary referral hospital. Clin Infect Dis. 2008;46:42–9.
Kim DH, Kim HJ, Park SK, Kong SJ, Kim YS, Kim TH, et al. Treatment outcomes and long-term survival in patients with extensively drug-resistant tuberculosis. Am J Respir Crit Care Med. 2008;178:1075–82.
Acknowledgments
We thank NTRL of NIDCH for providing us with the facilities for all the experiments described here. All the expenditures to carry out the necessary experiments required for this study have been met by the National Tuberculosis Reference Laboratory (NTRL), NIDCH, Bangladesh.
Conflict of interest
Authors have no potential conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
About this article
Cite this article
Noor, R., Akhter, S., Rahman, F. et al. Frequency of extensively drug-resistant tuberculosis (XDR-TB) among re-treatment cases in NIDCH, Dhaka, Bangladesh. J Infect Chemother 19, 243–248 (2013). https://doi.org/10.1007/s10156-012-0490-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10156-012-0490-8