Abstract
Background
The aim of the present study was to evaluate the effects of preoperative nutritional status on the short-term outcomes of an enhanced recovery after surgery (ERAS) programme for colorectal cancer surgery.
Methods
This prospective observational study included 149 patients who underwent elective resection of colorectal cancer with ERAS from January 2011 to January 2014 in a university hospital. Subjective global assessment (SGA) was used to determine preoperative nutritional status. Primary outcomes included the length of postoperative stay, postoperative morbidity, gastrointestinal recovery, and 30-day readmission.
Results
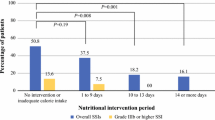
The patients were divided into 3 groups according to the SGA classification. There were 96 patients (64.4 %) in SGA-A (well-nourished), 48 (32.2 %) in SGA-B (mild to moderately malnourished), and 5 (3.4 %) in SGA-C (severely malnourished). Patients in SGA-A had the median length of postoperative stay of 4 days (range 2–23), which was significantly shorter compared to SGA-B (5 days; range 2–16; p < 0.01) and SGA-C (7 days; range 4–17; p < 0.01). The overall complication rates of SGA-A, SGA-B, and SGA-C patients were 11, 31 % (adjusted OR 3.76; 95 % CI 1.36–10.36; p < 0.01) and 40 % (adjusted OR 2.15; 95 % CI 0.07–63.64; p = 0.66). Mean time to resumption of normal diet and time to first defecation were 1.6 ± 1.3 and 2.2 ± 0.9 days in SGA-A, 2.6 ± 1.7 and 3.1 ± 1.6 days in SGA-B (p < 0.01 compared to SGA-A) and 3.2 ± 2.4 days and 2.6 ± 1.5 days in SGA-C (p = 0.07 and p = 0.1 compared to SGA-A, respectively). No 30-day mortality occurred in any group. One patient in SGA-A (1 %), and 3 patients in SGA-B (6 %) had unplanned 30-day re-admission; p = 0.11.
Conclusions
Within an ERAS programme for colorectal cancer surgery, malnourished patients were at risk for increased postoperative morbidity, delayed recovery of gastrointestinal function, and prolonged length of hospital stay.
Similar content being viewed by others
References
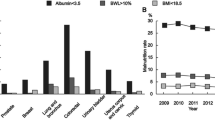
Lohsiriwat V, Chinswangwatanakul V, Lohsiriwat S et al (2007) Hypoalbuminemia is a predictor of delayed postoperative bowel function and poor surgical outcomes in right-sided colon cancer patients. Asia Pac J Clin Nutr 16:213–217
Lohsiriwat V, Lohsiriwat D, Boonnuch W, Chinswangwatanakul V, Akaraviputh T, Lert-Akayamanee N (2008) Pre-operative hypoalbuminemia is a major risk factor for postoperative complications following rectal cancer surgery. World J Gastroenterol 14:1248–1251
Cid Conde L, Fernandez Lopez T, Neira Blanco P, Arias Delgado J, Varela Correa J, Gomez Lorenzo F (2008) Hyponutrition prevalence among patients with digestive neoplasm before surgery. Nutr Hosp 23:46–53
Pressoir M, Desne S, Berchery D et al (2010) Prevalence, risk factors and clinical implications of malnutrition in French Comprehensive Cancer Centres. Br J Cancer 102:966–971
Zhang JQ, Curran T, McCallum JC et al (2014) Risk factors for readmission after lower extremity bypass in the American College of Surgeons National Surgery Quality Improvement Program. J Vasc Surg 59:1331–1339
Vashi PG, Gupta D, Lammersfeld CA et al (2013) The relationship between baseline nutritional status with subsequent parenteral nutrition and clinical outcomes in cancer patients undergoing hyperthermic intraperitoneal chemotherapy. Nutr J 12:118
Weimann A, Braga M, Harsanyi L et al (2006) ESPEN guidelines on enteral nutrition: surgery including organ transplantation. Clin Nutr 25:224–244
Ukleja A, Freeman KL, Gilbert K et al (2010) Standards for nutrition support: adult hospitalized patients. Nutr Clin Pract 25:403–414
Chambrier C, Sztark F (2012) French clinical guidelines on perioperative nutrition. Update of the 1994 consensus conference on perioperative artificial nutrition for elective surgery in adults. J Visc Surg 149:e325–e336
Braga M, Ljungqvist O, Soeters P, Fearon K, Weimann A, Bozzetti F (2009) ESPEN guidelines on parenteral nutrition: surgery. Clin Nutr 28:378–386
Gustafsson UO, Scott MJ, Schwenk W et al (2012) Guidelines for perioperative care in elective colonic surgery: enhanced recovery after surgery (ERAS) society recommendations. Clin Nutr 31:783–800
Nygren J, Thacker J, Carli F et al (2012) Guidelines for perioperative care in elective rectal/pelvic surgery: enhanced recovery after surgery (ERAS) society recommendations. Clin Nutr 31:801–816
Lohsiriwat V (2014) Impact of enhanced recovery program after surgery on the treatment of colorectal cancer. Asian Pac J Cancer Prev 15:3825–3828
Gustafsson UO, Hausel J, Thorell A, Ljungqvist O, Soop M, Nygren J (2011) Adherence to the enhanced recovery after surgery protocol and outcomes after colorectal cancer surgery. Arch Surg 146:571–577
Cakir H, van Stijn MF, Lopes Cardozo AM et al (2013) Adherence to enhanced recovery after surgery and length of stay after colonic resection. Colorectal Dis 15:1019–1025
Detsky AS, McLaughlin JR, Baker JP et al (1987) What is subjective global assessment of nutritional status? JPEN J Parenter Enter Nutr 11:8–13
Detsky AS, Baker JP, Mendelson RA, Wolman SL, Wesson DE, Jeejeebhoy KN (1984) Evaluating the accuracy of nutritional assessment techniques applied to hospitalized patients: methodology and comparisons. JPEN J Parenter Enter Nutr 8:153–159
Gupta D, Vashi PG, Lammersfeld CA, Braun DP (2011) Role of nutritional status in predicting the length of stay in cancer: a systematic review of the epidemiological literature. Ann Nutr Metab 59:96–106
Sungurtekin H, Sungurtekin U, Balci C, Zencir M, Erdem E (2004) The influence of nutritional status on complications after major intraabdominal surgery. J Am Coll Nutr 23:227–232
Gustafsson UO, Ljungqvist O (2011) Perioperative nutritional management in digestive tract surgery. Curr Opin Clin Nutr Metab Care 14:504–509
Fearon KC, Ljungqvist O, Von Meyenfeldt M et al (2005) Enhanced recovery after surgery: a consensus review of clinical care for patients undergoing colonic resection. Clin Nutr 24:466–477
Lassen K, Soop M, Nygren J et al (2009) Consensus review of optimal perioperative care in colorectal surgery: enhanced recovery after surgery (ERAS) group recommendations. Arch Surg 144:961–969
Lohsiriwat V (2014) Enhanced recovery after surgery vs conventional care in emergency colorectal surgery. World J Gastroenterol 20 (in press)
The Veterans Affairs Total Parenteral Nutrition Cooperative Study Group (1991) Perioperative total parenteral nutrition in surgical patients. N Engl J Med 325:525–532
Tekkis PP, Prytherch DR, Kocher HM et al (2004) Development of a dedicated risk-adjustment scoring system for colorectal surgery (colorectal POSSUM). Br J Surg 91:1174–1182
Dindo D, Demartines N, Clavien PA (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240:205–213
Wu B, Yin TT, Cao W et al (2010) Validation of the Chinese version of the Subjective Global Assessment scale of nutritional status in a sample of patients with gastrointestinal cancer. Int J Nurs Stud 47:323–331
Steenson J, Vivanti A, Isenring E (2013) Inter-rater reliability of the subjective global assessment: a systematic literature review. Nutrition 29:350–352
Hendry PO, Hausel J, Nygren J et al (2009) Determinants of outcome after colorectal resection within an enhanced recovery programme. Br J Surg 96:197–205
Mueller C, Compher C, Ellen DM (2011) A.S.P.E.N. clinical guidelines: nutrition screening, assessment, and intervention in adults. JPEN J Parenter Enter Nutr 35:16–24
Basse L, Hjort Jakobsen D, Billesbolle P, Werner M, Kehlet H (2000) A clinical pathway to accelerate recovery after colonic resection. Ann Surg 232:51–57
Li K, Li JP, Peng NH, Jiang LL, Hu YJ, Huang MJ (2014) Fast-track improves post-operative nutrition and outcomes of colorectal surgery: a single-center prospective trial in China. Asia Pac J Clin Nutr 23:41–47
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lohsiriwat, V. The influence of preoperative nutritional status on the outcomes of an enhanced recovery after surgery (ERAS) programme for colorectal cancer surgery. Tech Coloproctol 18, 1075–1080 (2014). https://doi.org/10.1007/s10151-014-1210-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10151-014-1210-4