Abstract
Background
Technical feasibility of inferior rectal nerve anastomosis to the anterior vagus branch of the perineally transposed antropyloric valve for total anorectal reconstruction has been previously demonstrated in cadavers. To the best of our knowledge, the present study is the first report of using this procedure in humans.
Methods
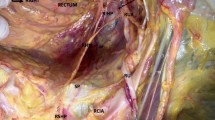
Eight patients [mean age 35.5 years (range 15–55 years); (male/female = 7:1)] underwent the procedure. The antropyloric valve with its anterior vagus branch was mobilized based on the left gastroepiploic arterial pedicle. The antral end was anastomosed to the distal colon. The anterior vagus nerve was anastomosed by epineural technique to the inferior rectal nerve in the perineum. A diverting proximal colostomy was maintained for 6 months. Anatomical integrity of the graft (on magnetic resonance imaging scans), its arterial pedicle (on computed tomography angiogram) and neural continuity (on ultrasound and pyloric electromyography) were assessed. Functional assessment was performed using barium retention studies, endoscopy, manometry and fecal incontinence scores.
Results
Tension-free end-to-end anastomosis of the anterior vagus nerve to the right (n = 7) and left (n = 1) inferior rectal nerve was achieved. An intact left gastroepiploic pedicle, a healthy graft and neural continuity were visualized on perineal ultrasound. Electromyographic activity was noticed on neural stimulation. Endoscopy and barium studies showed voluntary antral contraction and contrast retention, respectively, in all patients. The mean resting and squeeze pressures were 26.25 mmHg (range 16–62 mmHg) and 50.25 mmHg (range 16–113 mmHg), respectively. St. Mark’s incontinence scores varied between 7 and 12. There were no major surgical complications.
Conclusions
Pudendal (inferior rectal) innervation of the perineally transposed antropylorus in total anorectal reconstruction is feasible and may improve outcomes in selected patients with end-stage fecal incontinence.




Similar content being viewed by others
References
Tjandra JJ, Lim JF, Matzel K (2004) Sacral nerve stimulation: an emerging treatment for faecal incontinence. ANZ J Surg 74:1098–1106
Madoff RD, Baeten CG, Christiansen J et al (2000) Standards for anal sphincter replacement. Dis Colon Rectum 43:135–141
Mander BJ, Abercrombie JF, George BD, Williams NS (1996) The electrically stimulated gracilis neosphincter incorporated as part of total anorectal reconstruction after abdominoperineal excision of the rectum. Ann Surg 224:702–709
Congilosi SM, Johnson DR, Medot M et al (1997) Experimental model of pudendal nerve innervation of a skeletal muscle neosphincter for faecal incontinence. Br J Surg 84:1269–1273
Sato T, Konishi F, Kanazawa K (1997) Functional perineal colostomy with pudendal nerve anastomosis following anorectal resection: a cadaver operation study on a new procedure. Surgery 121:569–574
Sato T, Konishi F, Kanazawa K (1997) Anal sphincter reconstruction with a pudendal nerve anastomosis following abdominoperineal resection: report of a case. Dis Colon Rectum 40:1497–1502
Sato T, Konishi F, Endoh N, Uda H, Sugawara Y, Nagai H (2005) Long-term outcomes of a neo-anus with a pudendal nerve anastomosis contemporaneously reconstructed with an abdominoperineal excision of the rectum. Surgery 137:8–15
Chandra A, Kumar A, Noushif M et al (2013) Perineal antropylorus transposition for end-stage fecal incontinence in humans: initial outcomes. Dis Colon Rectum 56:360–366
Goldsmith HS, Chandra A (2011) Pyloric valve transposition as substitute for a colostomy in humans: a preliminary report. Am J Surg 202:409–416
Chandra A, Ghoshal UC, Gupta V (2012) Physiological and functional evaluation of the transposed human pylorus as a distal sphincter. J Neurogastroenterol Motil 18:269–277
Chandra A, Kumar A, Noushif M et al (2013) Feasibility of neurovascular antropylorus perineal transposition with pudendal nerve anastomosis following anorectal excision: a cadaveric study for neoanal reconstruction. Ann Coloproctol 29:7–11
Chandra A, Gupta V, Kumar M et al (2013) Anatomical basis of antro-pyloric transposition for fecal incontinence in humans: the infrapyloric approach. Surg Radiol Anat 35:67–74
Rodríguez L, Rodríguez P, Neto MG et al (2012) Short-term electrical stimulation of the lower esophageal sphincter increases sphincter pressure in patients with gastroesophageal reflux disease. Neurogastroenterol Motil 24:446–450
Chandra A (2012) Reply to: should we, not could we? A commentary on “pyloric valve transposition as substitute for a colostomy in humans: a preliminary report”. Am J Surg 204:806–807
Ratani RS, Yazaki E, Scott M, Pilot MA, Williams NS (1997) Electrically stimulated smooth muscle neosphincter. Br J Surg 84:1286–1289
Madoff RD, Rosen HR, Baeten CG et al (1999) Safety and efficacy of dynamic muscle plasty for anal incontinence: lessons from a prospective, multicenter trial. Gastroenterology 116:549–556
Wolford LM, Stevao EL (2003) Considerations in nerve repair. Proc (Bayl Univ Med Cent) 16:152–156
Burnett MG, Zager EL (2004) Pathophysiology of peripheral nerve injury: a brief review. Neurosurg Focus 16:E1
Dong C, Gao W, Jia R, Li S, Shen Z, Li B (2013) Reconstruction of anorectal function through end-to-side neurography by autonomic nerves and somatic nerve in rats. J Surg Res 180:e63–e71
Canning BJ (2006) Reflex regulation of airway smooth muscle tone. J Appl Physiol 101:971–985
Guyenet PG (2006) The sympathetic control of blood pressure. Nat Rev Neurosci 7:335–346
Acknowledgments
This study was supported by fund from Grant Number 2835/Lekha/09, Department of Surgical Gastroenterology, King George Medical University, India.
Conflict of interest
The authors declare no conflicts of interest.
Ethical standard
Ethics Committee, Institutional Review Board, King George’s Medical University, Lucknow, India.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Endoscopic assessment of the perineal antropyloric segment showing the suture line (colon–antral anastomosis) and antral contractions on voluntary attempts to retain feces (MPG 4836 kb)
Rights and permissions
About this article
Cite this article
Chandra, A., Kumar, A., Noushif, M. et al. Neurovascular antropylorus perineal transposition using inferior rectal nerve anastomosis for total anorectal reconstruction: preliminary report in humans. Tech Coloproctol 18, 535–542 (2014). https://doi.org/10.1007/s10151-013-1092-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10151-013-1092-x