Abstract
Background
Regorafenib is a key agent for patients with advanced or recurrent colorectal cancer. Sarcopenia represented by skeletal muscle depletion is closely related to frailty and predicts oncological prognoses. We hypothesized that sarcopenia negatively affects the time to treatment failure (TTF) or overall survival (OS) of patients treated with regorafenib.
Methods
We retrospectively reviewed the medical records of all patients treated with regorafenib between May 2013 and April 2019 at our institution. The cross-sectional area of the psoas muscle at the level of the third lumbar vertebra on baseline computed tomography (CT) was assessed to calculate the psoas muscle index (PMI). Sarcopenia was defined based on PMI cut-off values for Asian adults (6.36 cm2/m2 for males and 3.92 cm2/m2 for females).
Results
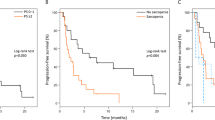
Thirty-four patients were analyzed. The prevalence of sarcopenia was 44.1%. Sarcopenia was significantly associated with poorer OS (median 3.2 vs. 5.3 months, p = 0.031). Less 75% 1-Month Relative Dose Intensity patients experienced significantly shorter TTF and OS than the rest, as did patients receiving total regorafenib dose of < 3360 mg (median 3.1 and 9.4 months, p < 0.001). Multivariate analysis showed that sarcopenia was a significant predictor of prognosis.
Conclusion
Sarcopenia was a predictive marker of negative outcome for patients with advanced or recurrent colorectal cancer treated with regorafenib. Screening for sarcopenia can be used to identify patients more likely to benefit from regorafenib in routine clinical practice.


Similar content being viewed by others
References
Grothey A, Van Cutsem E, Sobrero A et al (2013) Regorafenib monotherapy for previously treated metastatic colorectal cancer (CORRECT): an international, multicentre, randomised, placebo-controlled, phase 3 trial. Lancet 381(9863):303–312. https://doi.org/10.1016/S0140-6736(12)61900-X
Moriwaki T, Fukuoka S, Taniguchi H et al (2018) Propensity score analysis of regorafenib versus trifluridine/tipiracil in patients with metastatic colorectal cancer refractory to standard chemotherapy (REGOTAS): a Japanese Society for Cancer of the Colon and Rectum multicenter observational study. Oncologist 23(1):7–15. https://doi.org/10.1634/theoncologist.2017-0275
Lieffers JR, Bathe OF, Fassbender K et al (2012) Sarcopenia is associated with postoperative infection and delayed recovery from colorectal cancer resection surgery. Br J Cancer 107(6):931–936. https://doi.org/10.1038/bjc.2012.350
Rier HN, Jager A, Sleijfer S et al (2016) The prevalence and prognostic value of low muscle mass in cancer patients: a review of the literature. Oncologist 21(11):1396–1409. https://doi.org/10.1634/theoncologist.2016-0066
Miyamoto Y, Baba Y, Sakamoto Y et al (2015) Negative impact of skeletal muscle loss after systemic chemotherapy in patients with unresectable colorectal cancer. PLoS ONE. https://doi.org/10.1371/journal.pone.0129742
Shiroyama T, Nagatomo I, Koyama S et al (2019) Impact of sarcopenia in patients with advanced non-small cell lung cancer treated with PD-1 inhibitors: a preliminary retrospective study. Sci Rep. https://doi.org/10.1038/s41598-019-39120-6
Mitsiopoulos N, Baumgartner RN, Heymsfield SB et al (1998) Cadaver validation of skeletal muscle measurement by magnetic resonance imaging and computerized tomography. https://www.jap.org. Accessed 20 Apr 2020
Hamaguchi Y, Kaido T, Okumura S et al (2016) Proposal for new diagnostic criteria for low skeletal muscle mass based on computed tomography imaging in Asian adults. Nutrition 32(11–12):1200–1205. https://doi.org/10.1016/j.nut.2016.04.003
Shitara K, Matsuo K, Yokota T et al (2011) Prognostic factors for metastatic colorectal cancer patients undergoing irinotecan-based second-line chemotherapy. Gastrointest Cancer Res 4(5–6):168–172
Tohme S, Sukato D, Chalhoub D et al (2015) Neutrophil–lymphocyte ratio is a simple and novel biomarker for prediction of survival after radioembolization for metastatic colorectal cancer. Ann Surg Oncol 22(5):1701–1707. https://doi.org/10.1245/s10434-014-4050-6
Therneau TM, Grambsch PM (2000) Modeling survival data: extending the Cox model. Springer, New York. ISBN:0-387-98784-3
R Core Team (2019) R: a language and environment for statistical computing. R Foundation for Statistical Computing. Vienna. https://www.R-project.org/. Accessed 20 Apr 2020
Blauwhoff-Buskermolen S, Versteeg KS, De Van Der Schueren MAE et al (2016) Loss of muscle mass during chemotherapy is predictive for poor survival of patients with metastatic colorectal cancer. J Clin Oncol 34(12):1339–1344. https://doi.org/10.1200/JCO.2015.63.6043
Jung H, Kim JW, Kim J et al (2015) Effect of muscle mass on toxicity and survival in patients with colon cancer undergoing adjuvant chemotherapy. Support Care Cancer 23:687–694. https://doi.org/10.1007/s00520-014-2418-6
Huemer F, Schlintl V, Hecht S et al (2019) Regorafenib is associated with increased skeletal muscle loss compared to TAS-102 in metastatic colorectal cancer. Clin Colorectal Cancer 18(2):159-166.e3. https://doi.org/10.1016/j.clcc.2019.04.003
Gökyer A, Küçükarda A, Köstek O et al (2019) Relation between sarcopenia and dose-limiting toxicity in patients with metastatic colorectal cancer who received regorafenib. Clin Transl Oncol 21(11):1518–1523. https://doi.org/10.1007/s12094-019-02080-4
Bekaii-Saab T, Kim R, Kim TW et al (2019) Third- or later-line therapy for metastatic colorectal cancer: reviewing best practice. Clin Colorectal Cancer 18(1):e117–e129. https://doi.org/10.1016/j.clcc.2018.11.002
Melosky B (2016) Meeting an unmet need in metastatic colorectal carcinoma with regorafenib. Asia Pac J Oncol Nurs 3(1):58. https://doi.org/10.4103/2347-5625.178174
Krishnamoorthy SK, Relias V, Sebastian S et al (2015) Management of regorafenib-related toxicities: a review. Ther Adv Gastroenterol 8(5):285–297. https://doi.org/10.1177/1756283X15580743
Ozdemir Y, Akin ML, Sucullu I et al (2014) Pretreatment neutrophil/lymphocyte ratio as a prognostic aid in colorectal cancer. Asia Pac J Cancer Prev 15(6):2647–2650. https://doi.org/10.7314/APJCP.2014.15.6.2647
Sato H, Tsubosa Y, Kawano T (2012) Correlation between the pretherapeutic neutrophil to lymphocyte ratio and the pathologic response to neoadjuvant chemotherapy in patients with advanced esophageal cancer. World J Surg 36(3):617–622. https://doi.org/10.1007/s00268-011-1411-1
Cruz-Jentoft AJ, Baeyens JP, Bauer JM et al (2010) Sarcopenia: European consensus on definition and diagnosis. Age Ageing 39(4):412–423. https://doi.org/10.1093/ageing/afq034
Chen LK, Liu LK, Woo J et al (2014) Sarcopenia in Asia: consensus report of the Asian Working Group for Sarcopenia. J Am Med Dir Assoc 15(2):95–101. https://doi.org/10.1016/j.jamda.2013.11.025
Fielding RA, Vellas B, Evans WJ et al (2011) Sarcopenia: an undiagnosed condition in older adults. Current consensus definition: prevalence, etiology, and consequences. International Working Group on Sarcopenia. J Am Med Dir Assoc 12(4):249–256. https://doi.org/10.1016/j.jamda.2011.01.003
Studenski SA, Peters KW, Alley DE et al (2014) The FNIH sarcopenia project: rationale, study description, conference recommendations, and final estimates. J Gerontol A Biol 69A(5):547–558. https://doi.org/10.1093/gerona/glu010
He L, Li H, Cai J et al (2018) Prognostic value of the Glasgow prognostic score or modified Glasgow prognostic score for patients with colorectal cancer receiving various treatments: a systematic review and meta-analysis. Cell Physiol Biochem 51(3):1237–1249. https://doi.org/10.1159/000495500
Hayashi N, Ando Y, Gyawali B et al (2016) Low skeletal muscle density is associated with poor survival in patients who receive chemotherapy for metastatic gastric cancer. Oncol Rep 35(3):1727–1731. https://doi.org/10.3892/or.2015.4475
Prado CMM, Lieff JR, McCargar LJ et al (2008) Prevalence and clinical implications of sarcopenic obesity in patients with solid tumours of the respiratory and gastrointestinal tracts: a population-based study. Lancet Oncol 9(7):629–635. https://doi.org/10.1016/S1470-2045(08)70153-0
Tsuchihashi K, Ito M, Moriwaki T et al (2018) Role of predictive value of the modified Glasgow prognostic score for later-line chemotherapy in patients with metastatic colorectal cancer. Clin Colorectal Cancer. https://doi.org/10.1016/j.clcc.2018.07.004
Jang BY, Bu SY (2019) Erratum to: Total energy intake according to the level of skeletal muscle mass in Korean adults aged 30 years and older: an analysis of the Korean national health and nutrition examination surveys (KNHANES) 2008–2011 [Nutrition Research and Practice, (2018);12, 3(222–223), 10.4162/nrp.2018.12.3.222)]. Nutr Res Pract 13(2):178. https://doi.org/10.4162/nrp.2019.13.2.178
Beaudart C, Dawson A, Shaw SC et al (2017) Nutrition and physical activity in the prevention and treatment of sarcopenia: systematic review. Osteoporos Int 28(6):1817–1833. https://doi.org/10.1007/s00198-017-3980-9
Osawa H (2017) Response to regorafenib at an initial dose of 120 mg as salvage therapy for metastatic colorectal cancer. Mol Clin Oncol 6(3):365–372. https://doi.org/10.3892/mco.2017.1145
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None of the authors has any conflicts of interest to declare.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
About this article
Cite this article
Murachi, Y., Sakai, D., Koseki, J. et al. Impact of sarcopenia in patients with advanced or recurrent colorectal cancer treated with regorafenib. Int J Clin Oncol 26, 409–416 (2021). https://doi.org/10.1007/s10147-020-01805-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10147-020-01805-8