Abstract
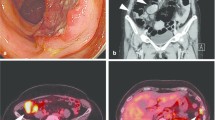
A 77-year-old man presented with a 2-month history of an enlarged right inguinal lymph node. Diagnostic excisional biopsy of the inguinal lymph node proved it to be a poorly differentiated neuroendocrine carcinoma by histological and immunohistological analyses. We diagnosed a poorly differentiated neuroendocrine carcinoma by histological examination and immunohistological analysis of the resected inguinal lymph node. We performed computed tomographic examination and positron emission tomography, which identified lymph node involvement without any signs of other tumors. Because these tumors had grown expandingly and had been encapsulated locally, we performed an operation to dissect all of the involved lymph nodes. Direct invasion to the right external iliac artery was not detected, and two of the enlarged lymph nodes were successfully resected without any complications. Pathologically, the resected specimen was diagnosed as a neuroendocrine carcinoma with a negative surgical margin and it was similar to the histology of the inguinal lymph node previously resected. The patient had no recurrence for 3 years without receiving any adjuvant treatment. There have been no reports describing a case of poorly differentiated neuroendocrine carcinoma, of unknown origin, which metastasized to other lymph nodes. Although further studies are required, complete resection of the involved lymph nodes should be considered as a choice for localized, expanding growth-pattern disease even if it is undifferentiated type.


Similar content being viewed by others
References
Hess KR, Abbruzzese MC, Lenzi R et al (1999) Classification and regression tree analysis of 1000 consecutive patients with unknown primary carcinoma. Clin Cancer Res 5:3403–3410
Pavlidis N (2003) Cancer of unknown primary: biological and clinical characteristics. Ann Oncol 14(suppl 3):iii11–iii18
Pavlidis N (2007) Forty years experience of treating cancer of unknown primary. Acta Oncol 46:592–601
Demir H, Berk F, Raderer M et al (2004) The role of nuclear medicine in the diagnosis of cancer of unknown origin. Q J Nucl Med Mol Imaging 48:164–173
Briasoulis E, Fountzilas G, Bamias A et al (2008) Multicenter phase-II trial of irinotecan plus oxaliplatin [IROX regimen] in patients with poor-prognosis cancer of unknown primary: a Hellenic Cooperative Oncology Group study. Cancer Chemother Pharmacol 62:277–284
Ghosh L, Dahut W, Kakar S et al (2005) Management of patients with metastatic cancer of unknown primary. Curr Probl Surg 42:12–66
Briasoulis E, Tolis C, Bergh J et al (2005) ESMO minimum clinical recommendations for diagnosis, treatment and follow-up of cancers of unknown primary site (CUP). Ann Oncol 16(suppl 1):i75–i76
Eng TY, Boersma MG, Fuller CD et al (2004) Treatment of Merkel cell carcinoma. Am J Clin Oncol 27:510–515
Ott MJ, Tanabe KK, Gadd MA et al (1999) Multimodality management of Merkel cell carcinoma. Arch Surg 134:388–392 (discussion 92–93)
Lin X, Saad RS, Luckasevic TM et al (2007) Diagnostic value of CDX-2 and TTF-1 expressions in separating metastatic neuroendocrine neoplasms of unknown origin. Appl Immunohistochem Mol Morphol 15:407–414
Essner R, Scheri R, Kavanagh M et al (2006) Surgical management of the groin lymph nodes in melanoma in the era of sentinel lymph node dissection. Arch Surg 141:877–882 (discussion 82–84)
Zhu Y, Zhang SL, Ye DW et al (2009) Prospectively packaged ilioinguinal lymphadenectomy for penile cancer: the disseminative pattern of lymph node metastasis. J Urol 181:2103–2108
Eusebi V, Capella C, Cossu A et al (1992) Neuroendocrine carcinoma within lymph nodes in the absence of a primary tumor, with special reference to Merkel cell carcinoma. Am J Surg Pathol 16:658–666
Kuwabara H, Mori H, Uda H et al (2003) Nodal neuroendocrine (Merkel cell) carcinoma without an identifiable primary tumor. Acta Cytol 47:515–517
Hainsworth JD, Spigel DR, Litchy S et al (2006) Phase II trial of paclitaxel, carboplatin, and etoposide in advanced poorly differentiated neuroendocrine carcinoma: a Minnie Pearl Cancer Research Network Study. J Clin Oncol 24:3548–3554
Kulke MH, Bergsland EK, Ryan DP et al (2006) Phase II study of recombinant human endostatin in patients with advanced neuroendocrine tumors. J Clin Oncol 24:3555–3561
Kulke MH, Stuart K, Enzinger PC et al (2006) Phase II study of temozolomide and thalidomide in patients with metastatic neuroendocrine tumors. J Clin Oncol 24:401–406
Acknowledgments
We thank Yohei Shimono and Michael E. Rothenberg for critical reading.
Conflict of interest statement
None.
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Hisamori, S., Okabe, H., Yoshizawa, A. et al. A case of long-term recurrence-free poorly differentiated neuroendocrine carcinoma of lymph nodes treated by surgical resection without any chemotherapy. Int J Clin Oncol 15, 493–496 (2010). https://doi.org/10.1007/s10147-010-0058-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10147-010-0058-5