Abstract
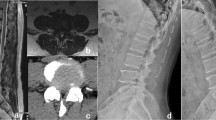
This study retrospectively compared clinical and radiological outcomes of unilateral biportal endoscopic lumbar interbody fusion (ULIF) to those of conventional posterior lumbar interbody fusion (PLIF). Seventy-one ULIF (age, 68 ± 8 years) and 70 PLIF (66 ± 9 years) patients for one lumbosacral segment followed more than 1 year were selected. Parameters for surgical techniques (operation time, whether transfused), clinical results [visual analogue scale (VAS) for back and leg pain, Oswestry disability index (ODI)], surgical complications (dural tear, nerve root injury, infection), and radiological results (cage subsidence, screw loosening, fusion) between the two groups were compared. The PLIF group demonstrated a significantly shorter operation time and more transfusions done than the ULIF group. The VAS for leg pain in both groups and for back pain in the ULIF group significantly improved at 1 week, while the VAS for back pain in the PLIF group significantly improved at 1 year. ODI scores improved at 1 year in both groups. Complication rates were not significantly different between groups. Fusion rates with definite and probable grades were not significantly different between groups. However, the ULIF group had significantly (P = 0.013) fewer cases of definite fusion and more cases of probable fusion [43 (74.1%) and 15 (25.9%) cases, respectively] than the PLIF group [58 (92.1%) and 5 (7.9%) cases, respectively]. ULIF is less invasive while just as effective as conventional PLIF in improving clinical outcomes and obtaining fusion. However, ULIF has a longer operation time than PLIF and requires further development to improve the fusion grade.





Similar content being viewed by others
Change history
24 June 2019
The original publication of this article has incorrect presentation of one of the author names. Instead of Sangu-Kyu Son, it should have been Sang-Kyu Son.
References
Basques B, Golinvaux N, Bohl D, Yacob A, Toy J, Varthi A, Grauer J (2014) Use of an operating microscope during spine surgery is associated with minor increases in operating room times and no increased risk of infection. Spine 39:1910–1916
Boukebir M, Berlin C, Navarro Ramirez R, Heiland T, Schöller K, Rawanduzy C, Kirnaz S, Jada A, Härtl R (2017) Ten-step minimally invasive spine lumbar decompression and dural repair through tubular retractors. Open Neurosci J 13:232–245
Elkan P, Sten Linder M, Hedlund R, Willers U, Ponzer S, Gerdhem P (2016) Markers of inflammation and fibrinolysis in relation to outcome after surgery for lumbar disc herniation. A prospective study on 177 patients. Eur Spine J 25:186–191
Gibson JNA, Subramanian A, Scott CEH (2017) A randomised controlled trial of transforaminal endoscopic discectomy vs microdiscectomy. Eur Spine J 26:847–856
Hara M, Takahashi H, Yokoyama Y, Wada A, Hasegawa K, Iida Y (2015) Comparison of the invasiveness of conventional discectomy and microendoscopic discectomy for lumbar disc herniation: differences in the methods of approach. Asian J Endosc Surg 8:40–47
Heo D, Son S, Eum J, Park C (2017) Fully endoscopic lumbar interbody fusion using a percutaneous unilateral biportal endoscopic technique: technical note and preliminary clinical results. Neurosurg Focus 43:E8–E8
Hsu H-T, Chang S-J, Yang S, Chai C (2013) Learning curve of full-endoscopic lumbar discectomy. Eur Spine J 22:727–733
Hwa Eum J, Hwa Heo D, Son S, Park C (2016) Percutaneous biportal endoscopic decompression for lumbar spinal stenosis: a technical note and preliminary clinical results. J Neurosurg Spine 24:602–607
Jacquot F, Gastambide D (2013) Percutaneous endoscopic transforaminal lumbar interbody fusion: is it worth it? Int Orthop 37:1507–1510
Jin Tao Q, Yu T, Mei W, Xu Dong T, Tian Jian Z, Guo Hua S, Lei C, Yue H, Zi Tian W, Yue Z (2015) Comparison of MIS vs. open PLIF/TLIF with regard to clinical improvement, fusion rate, and incidence of major complication: a meta-analysis. Eur Spine J 24:1058–1065
Komp M, Hahn P, Oezdemir S, Giannakopoulos A, Heikenfeld R, Kasch R, Merk H, Godolias G, Ruetten S (2015) Bilateral spinal decompression of lumbar central stenosis with the full-endoscopic interlaminar versus microsurgical laminotomy technique: a prospective, randomized, controlled study. Pain Physician 18:61–70
Lee C, Choi M, Ryu D, Choi I, Kim C, Kim H, Sohn M (2018) Efficacy and safety of full-endoscopic decompression via interlaminar approach for central or lateral recess spinal stenosis of the lumbar spine: a meta-analysis. Spine (Phila Pa 1976) 43:1756–1764. https://doi.org/10.1097/BRS.0000000000002708
Lee K, Yue W, Yeo W, Soehamo H, Tan S (2012) Clinical and radiological outcomes of open versus minimally invasive transforaminal lumbar interbody fusion. Eur Spine J 21:2265–2270
Lee S, Lee J, Yeom J, Kim K-J, Kim H-J, Chung S, Kang H (2010) A practical MRI grading system for lumbar foraminal stenosis. AJR Am J Roentgenol 194:1095–1098
Rasouli MR, Rahimi-Movaghar V, Shokraneh F, Moradi-Lakeh M, Chou R (2014) Minimally invasive discectomy versus microdiscectomy/open discectomy for symptomatic lumbar disc herniation. Cochrane Database Syst Rev 4. John Wiley &Sons, Ltd, New York. https://doi.org/10.1002/14651858.CD010328.pub2
Ruan W, Feng F, Liu Z, Xie J, Cai L, Ping A (2016) Comparison of percutaneous endoscopic lumbar discectomy versus open lumbar microdiscectomy for lumbar disc herniation: a metaanalysis. Int J Surg 31:86–92
Torudom Y, Dilokhuttakarn T (2016) Two portal percutaneous endoscopic decompression for lumbar spinal stenosis: preliminary study. Asian Spine J 10:335–342
Wang M, Grossman J (2016) Endoscopic minimally invasive transforaminal interbody fusion without general anesthesia: initial clinical experience with 1-year follow-up. Neurosurg Focus 40:E13–E13
Youn MS, Shin JK, Goh TS, Lee JS (2018) Full endoscopic lumbar interbody fusion (FELIF): technical note. Eur Spine J 27:1949–1955. https://doi.org/10.1007/s00586-018-5521-4
Funding
No funding was received for this research.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Ethical approval was obtained from the Institutional Ethics Committee of the Ministry of Health and Welfare in South Korea (P01-201810-21-006).
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original version of this article was revised as the name of Sang-Kyu Son was incorrectly presented as Sangu-Kyu Son.
Electronic supplementary material
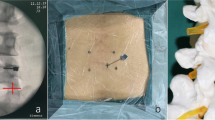
ULIF procedures resecting facet joint and exposing the ipsilateral disc surface (WMV 12427 kb)
Endplate preparation in ULIF procedures (WMV 13896 kb)
Online resource 3
Cage inserting procedure while protecting thecal sac in ULIF procedures (WMV 10740 kb)
Rights and permissions
About this article
Cite this article
Park, MK., Park, SA., Son, SK. et al. Clinical and radiological outcomes of unilateral biportal endoscopic lumbar interbody fusion (ULIF) compared with conventional posterior lumbar interbody fusion (PLIF): 1-year follow-up. Neurosurg Rev 42, 753–761 (2019). https://doi.org/10.1007/s10143-019-01114-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10143-019-01114-3