Abstract
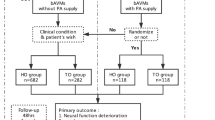
The treatment of brain arteriovenous malformations supplied by deep perforating arteries (PA) (P-BAVM) remains challenging. The aims of this study were to determine the outcomes after surgical treatment in patients with P-BAVMs and to identify the risk factors associated with postoperative neurological deficits. We retrospectively reviewed the medical charts and imaging records of 228 consecutive patients with BAVMs who underwent microsurgical resection of their BAVMs at Beijing Tiantan Hospital between September 2012 and March 2016. Patients were included if the BAVMs were totally or partially supplied by PA. All patients had undergone preoperative diffusion tensor imaging (DTI), MRI, 3D time-of-flight MRA (3D TOF-MRA) and digital subtraction angiography (DSA) followed by resection. Both functional and angioarchitectural factors were analysed with respect to the postoperative neurological deficits, including motor deficits, visual field deficits and aphasia. Statistical analysis was performed using the statistical package SPSS (version 20.0.0, IBM Corp.). Fifty-nine patients with P-BAVMs were enrolled. Radical obliteration was achieved in all P-BAVMs according to postoperative DSA. Forty-five (76.3%) patients obtained neurological deficits 1 week after surgery. At a mean follow-up of 14.7 ± 9.4 (3–30) months after surgery, 34 patients (57.6%) had long-term neurological deficits. Multivariable logistic regression analyses showed that a shorter lesion-to-eloquent fibre tracts distance (LFD) was an independent risk factor for short- (P = 0.014) and long-term (P = 0.013) neurological deficits. The cut-off point of LFD for long-term neurological deficits was 5.20 mm. The predominant supply of the PA (P = 0.008) was an independent risk factor for long-term neurological deficits. This study identified a high risk of surgical morbidity for P-BAVMs. The predominant supply of the PA and a shorter LFD are crucial risk factors for postoperative neurological deficits in patients with P-BAVMs.




Similar content being viewed by others
References
Bello L, Gambini A, Castellano A, Carrabba G, Acerbi F, Fava E, Giussani C, Cadioli M, Blasi V, Casarotti A, Papagno C, Gupta AK, Gaini S, Scotti G, Falini A (2008) Motor and language DTI fiber tracking combined with intraoperative subcortical mapping for surgical removal of gliomas. NeuroImage 39:369–382. doi:10.1016/j.neuroimage.2007.08.031
Berube J, McLaughlin N, Bourgouin P, Beaudoin G, Bojanowski MW (2007) Diffusion tensor imaging analysis of long association bundles in the presence of an arteriovenous malformation. J Neurosurg 107:509–514. doi:10.3171/JNS-07/09/0509
Catani M, Mesulam M (2008) The arcuate fasciculus and the disconnection theme in language and aphasia: history and current state. Cortex; a journal devoted to the study of the nervous system and behavior 44:953–961. doi:10.1016/j.cortex.2008.04.002
Dowd CF, Halbach VV, Barnwell SL, Higashida RT, Hieshima GB (1991) Particulate embolization of the anterior choroidal artery in the treatment of cerebral arteriovenous malformations. AJNR Am J Neuroradiol 12:1055–1061
Du R, Keyoung HM, Dowd CF, Young WL, Lawton MT (2007) The effects of diffuseness and deep perforating artery supply on outcomes after microsurgical resection of brain arteriovenous malformations. Neurosurgery 60:638–646 . doi:10.1227/01.NEU.0000255401.46151.8A discussion 646-638
Elkordy A, Endo H, Sato K, Matsumoto Y, Kondo R, Niizuma K, Endo T, Fujimura M, Tominaga T (2016) Embolization of the choroidal artery in the treatment of cerebral arteriovenous malformations. J Neurosurg:1–9. doi:10.3171/2016.2.JNS152370
Fujita K, Matsumoto S (1984) Anterior choroidal artery arteriovenous malformation. Its clinical manifestations and surgical treatment Surgical neurology 22:347–352
Hashimoto N, Nozaki K, Takagi Y, Kikuta K, Mikuni N (2007) Surgery of cerebral arteriovenous malformations. Neurosurgery 61:375–387 . doi:10.1227/01.NEU.0000255491.95944.EB discussion 387-379
Hong JH, Kim SH, Ahn SH, Jang SH (2009) The anatomical location of the arcuate fasciculus in the human brain: a diffusion tensor tractography study. Brain Res Bull 80:52–55. doi:10.1016/j.brainresbull.2009.05.011
Jiao Y, Lin F, Wu J, Li H, Wang L, Jin Z, Wang S, Cao Y (2016) Lesion-to-eloquent fiber distance is a crucial risk factor in presurgical evaluation of arteriovenous malformations in the temporo-occipital junction. World neurosurgery 93:355–364. doi:10.1016/j.wneu.2016.06.059
Kim DJ, Kim DI, Lee SK, Kim SY (2003) Homonymous hemianopia after embolization of an aneurysm-associated AVM supplied by the anterior choroidal artery. Yonsei Med J 44:1101–1105. doi:10.3349/ymj.2003.44.6.1101
Lawton MT, Kim H, McCulloch CE, Mikhak B, Young WL (2010) A supplementary grading scale for selecting patients with brain arteriovenous malformations for surgery. Neurosurgery 66:702–713 . doi:10.1227/01.NEU.0000367555.16733.E1 discussion 713
Lin F, Zhao B, Wu J, Wang L, Jin Z, Cao Y, Wang S (2015) Risk factors for worsened muscle strength after the surgical treatment of arteriovenous malformations of the eloquent motor area. J Neurosurg:1–10. doi:10.3171/2015.6.JNS15969
Marinkovic S, Gibo H, Milisavljevic M, Cetkovic M (2001) Anatomic and clinical correlations of the lenticulostriate arteries. Clin Anat 14:190–195. doi:10.1002/ca.1032
Marinkovic SV, Kovacevic MS, Marinkovic JM (1985) Perforating branches of the middle cerebral artery. Microsurgical anatomy of their extracerebral segments Journal of neurosurgery 63:266–271. doi:10.3171/jns.1985.63.2.0266
Ohue S, Kohno S, Inoue A, Yamashita D, Harada H, Kumon Y, Kikuchi K, Miki H, Ohnishi T (2012) Accuracy of diffusion tensor magnetic resonance imaging-based tractography for surgery of gliomas near the pyramidal tract: a significant correlation between subcortical electrical stimulation and postoperative tractography. Neurosurgery 70:283–293 . doi:10.1227/NEU.0b013e31823020e6 discussion 294
Okada T, Miki Y, Kikuta K, Mikuni N, Urayama S, Fushimi Y, Yamamoto A, Mori N, Fukuyama H, Hashimoto N, Togashi K (2007) Diffusion tensor fiber tractography for arteriovenous malformations: quantitative analyses to evaluate the corticospinal tract and optic radiation. AJNR Am J Neuroradiol 28:1107–1113. doi:10.3174/ajnr.A0493
Peltier J, Travers N, Destrieux C, Velut S (2006) Optic radiations: a microsurgical anatomical study. J Neurosurg 105:294–300. doi:10.3171/jns.2006.105.2.294
Potts MB, Young WL, Lawton MT, Project UBAS (2013) Deep arteriovenous malformations in the basal ganglia, thalamus, and insula: microsurgical management, techniques, and results. Neurosurgery 73:417–429. doi:10.1227/NEU.0000000000000004
Rhoton AL Jr, Fujii K, Fradd B (1979) Microsurgical anatomy of the anterior choroidal artery. Surg Neurol 12:171–187
Sherbondy AJ, Dougherty RF, Napel S, Wandell BA (2008) Identifying the human optic radiation using diffusion imaging and fiber tractography. J Vis 8(12):11–11. doi:10.1167/8.10.12
Speizler RF, Martin NA (2008) A proposed grading system for arteriovenous malformations. 1986. J Neurosurg 108:186–193. doi:10.3171/JNS/2008/108/01/0186
Umansky F, Gomes FB, Dujovny M, Diaz FG, Ausman JI, Mirchandani HG, Berman SK (1985) The perforating branches of the middle cerebral artery. A microanatomical study Journal of neurosurgery 62:261–268. doi:10.3171/jns.1985.62.2.0261
Wang S, Poptani H, Bilello M, Wu X, Woo JH, Elman LB, McCluskey LF, Krejza J, Melhem ER (2006) Diffusion tensor imaging in amyotrophic lateral sclerosis: volumetric analysis of the corticospinal tract. AJNR Am J Neuroradiol 27:1234–1238
Zhao B, Cao Y, Zhao Y, Wu J, Wang S (2014) Functional MRI-guided microsurgery of intracranial arteriovenous malformations: study protocol for a randomised controlled trial. BMJ Open 4:e006618. doi:10.1136/bmjopen-2014-006618
Zhu FP, Wu JS, Song YY, Yao CJ, Zhuang DX, Xu G, Tang WJ, Qin ZY, Mao Y, Zhou LF (2012) Clinical application of motor pathway mapping using diffusion tensor imaging tractography and intraoperative direct subcortical stimulation in cerebral glioma surgery: a prospective cohort study. Neurosurgery 71:1170–1183 . doi:10.1227/NEU.0b013e318271bc61 discussion 1183-1174
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This study was supported by the “Key Project of Beijing Municipal Science & Technology Commission” (Grant No. D161100003816006, Principle Investigator: Professor Shuo Wang and Grant No. D161100003816005, Principle Investigator: Professor Jizong Zhao) and the “National key research and development program of China during the 13th Five-Year Plan Period” (Grant No. 2016YFC1301801, Principle Investigator: Professor Shuo Wang and Grant No. 2016YFC1301803, Principle Investigator: Professor Yong Cao).
Conflict of interest
The authors declare that they have are no conflicts of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the Institutional Review Board of Beijing Tiantan Hospital Affiliated with Capital Medical University (ky2012-016-02) and the national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants who were included in the study.
Rights and permissions
About this article
Cite this article
Jiao, Y., Lin, F., Wu, J. et al. Risk factors for neurological deficits after surgical treatment of brain arteriovenous malformations supplied by deep perforating arteries. Neurosurg Rev 41, 255–265 (2018). https://doi.org/10.1007/s10143-017-0848-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10143-017-0848-6