Abstract
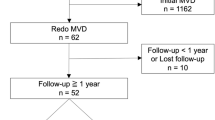
Microvascular decompression (MVD) is an effective and safe treatment option that offers the prospect of definitive cure for hemifacial spasm (HFS). However, there are potential risks of complications for MVD associated with retromastoid suboccipital craniectomy (RmSOC) and cranial nerves in particular. The purpose of this study was to identify clinical characteristics of possible complications after MVD for HFS and to establish appropriate management concept of these complications. We retrospectively reviewed medical records of 2040 patients who underwent RmSOC with MVD for HFS at Samsung medical center between January 1998 and March 2013. Of 2040 patients, 2027 were followed (99.4 %). Of the 2027 patients, 1841 (90.8 %) exhibited complete relief or minimal symptoms, and 113 (5.6 %) reported improved spasm but had mild remnant symptoms. After operation, the most frequently developed complications were facial nerve palsy (8.19 %), followed by middle ear effusion (4.90 %) and hearing loss (3.63 %). There were two cases of supratentorial subdural hemorrhage, three cases of infarction. MVD was found to be safe and effective treatment for HFS, in consistent with previous reports. Some of the complications such as facial nerve palsy, middle ear effusion, and hearing loss are relatively common. However, they have mild clinical courses that are usually transient.

Similar content being viewed by others
References
Barker FG 2nd, Jannetta PJ, Bissonette DJ, Larkins MV, Jho HD (1996) The long-term outcome of microvascular decompression for trigeminal neuralgia. N Engl J Med 334:1077–1083
Barker FG 2nd, Jannetta PJ, Bissonette DJ, Shields PT, Larkins MV, Jho HD (1995) Microvascular decompression for hemifacial spasm. J Neurosurg 82:201–210
Burchiel KJ, Clarke H, Haglund M, Loeser JD (1988) Long-term efficacy of microvascular decompression in trigeminal neuralgia. J Neurosurg 69:35–38
da Cruz MJ, Fagan P, Atlas M, McNeill C (1997) Drill-induced hearing loss in the nonoperated ear. Otolaryngol Head Neck Surg 117:555–558
Furukawa K, Sakoh M, Kumon Y et al (2003) Delayed facial palsy after microvascular decompression for hemifacial spasm due to reactivation of varicella-zoster virus. No Shinkei Geka 31:899–902
Gardner WJ (1962) Concerning the mechanism of trigeminal neuralgia and hemifacial spasm. J Neurosurg 19:947–958
Gardner WJ (1968) Trigeminal neuralgia. Clin Neurosurg 15:1–56
Grant R, Ferguson MM, Strang R, Turner JW, Bone I (1987) Evoked taste thresholds in a normal population and the application of electrogustometry to trigeminal nerve disease. J Neurol Neurosurg Psychiatry 50:12–21
Guclu B, Sindou M, Meyronet D, Streichenberger N, Simon E, Mertens P (2011) Cranial nerve vascular compression syndromes of the trigeminal, facial and vago-glossopharyngeal nerves: comparative anatomical study of the central myelin portion and transitional zone; correlations with incidences of corresponding hyperactive dysfunctional syndromes. Acta Neurochir (Wien) 153:2365–2375
Han JS, Lee JA, Kong DS, Park K (2012) Delayed cranial nerve palsy after microvascular decompression for hemifacial spasm. J Korean Neurosurg Soc 52:288–292
Harrison SA, Risser WL (1988) Repeat lumbar puncture in the differential diagnosis of meningitis. Pediatr Infect Dis J 7:143–145
Hongo K, Kobayashi S, Takemae T, Sugita K (1985) Posterior fossa microvascular decompression for hemifacial spasm and trigeminal neuralgia—some improvements on operative devices and technique. No Shinkei Geka 13:1291–1296
Huh R, Han IB, Moon JY, Chang JW, Chung SS (2008) Microvascular decompression for hemifacial spasm: analyses of operative complications in 1582 consecutive patients. Surg Neurol 69:153–157, discussion 157
Jeon CJ, Kong DS, Lee JA, Park K (2010) The efficacy and safety of microvascular decompression for hemifacial spasm in elderly patients. J Korean Neurosurg Soc 47:442–445
Jo KW, Lee JA, Park K, Cho YS (2013) A new possible mechanism of hearing loss after microvascular decompression for hemifacial spasm. Otol Neurotol 34:1247–1252
Lee MH, Lee HS, Jee TK et al (2015) Cerebellar retraction and hearing loss after microvascular decompression for hemifacial spasm. Acta Neurochir (Wien) 157:337–343
Lovely TJ, Getch CC, Jannetta PJ (1998) Delayed facial weakness after microvascular decompression of cranial nerve VII. Surg Neurol 50:449–452
McLaughlin MR, Jannetta PJ, Clyde BL, Subach BR, Comey CH, Resnick DK (1999) Microvascular decompression of cranial nerves: lessons learned after 4400 operations. J Neurosurg 90:1–8
Menovsky T, van Overbeeke JJ (1999) On the mechanism of transient postoperative deficit of cranial nerves. Surg Neurol 51:223–226
Miller LE, Miller VM (2012) Safety and effectiveness of microvascular decompression for treatment of hemifacial spasm: a systematic review. Br J Neurosurg 26:438–444
Negrini B, Kelleher KJ, Wald ER (2000) Cerebrospinal fluid findings in aseptic versus bacterial meningitis. Pediatrics 105:316–319
Nguyen DQ, Franco-Vidal V, Guerin J, Darrouzet V (2004) Delayed facial palsy after vestibular schwannoma resection: the role of viral reactivation. Our experience in 8 cases. Rev Laryngol Otol Rhinol (Bord) 125:23–29
Park JH, Jo KI, Park K (2013) Delayed unilateral soft palate palsy without vocal cord involvement after microvascular decompression for hemifacial spasm. J Korean Neurosurg Soc 53:364–367
Park JS, Kong DS, Lee JA, Park K (2007) Intraoperative management to prevent cerebrospinal fluid leakage after microvascular decompression: dural closure with a “plugging muscle” method. Neurosurg Rev 30:139–142, discussion 142
Park K, Hong SH, Hong SD, Cho YS, Chung WH, Ryu NG (2009) Patterns of hearing loss after microvascular decompression for hemifacial spasm. J Neurol Neurosurg Psychiatry 80:1165–1167
Park P, Toung JS, Smythe P, Telian SA, La Marca F (2006) Unilateral sensorineural hearing loss after spine surgery: case report and review of the literature. Surg Neurol 66:415–418, discussion 418-419
Polo G, Fischer C, Sindou MP, Marneffe V (2004) Brainstem auditory evoked potential monitoring during microvascular decompression for hemifacial spasm: intraoperative brainstem auditory evoked potential changes and warning values to prevent hearing loss—prospective study in a consecutive series of 84 patients. Neurosurgery 54:97–104, discussion 104-106
Rhee DJ, Kong DS, Park K, Lee JA (2006) Frequency and prognosis of delayed facial palsy after microvascular decompression for hemifacial spasm. Acta Neurochir (Wien) 148:839–843, discussion 843
Sammons VJ, Jacobson E, Lawson J (2009) Resolution of hydrocephalus-associated sensorineural hearing loss after insertion of ventriculoperitoneal shunt. J Neurosurg Pediatr 4:394–396
Shah A, Nikonow T, Thirumala P et al (2012) Hearing outcomes following microvascular decompression for hemifacial spasm. Clin Neurol Neurosurg 114:673–677
Sindou M, Leston J, Howeidy T, Decullier E, Chapuis F (2006) Micro-vascular decompression for primary Trigeminal Neuralgia (typical or atypical). Long-term effectiveness on pain; prospective study with survival analysis in a consecutive series of 362 patients. Acta Neurochir (Wien) 148:1235–1245, discussion 1245
Tandon PN, Sinha A, Kacker SK, Saxena RK, Singh K (1973) Auditory function in raised intracranial pressure. J Neurol Sci 18:455–467
Walsted A, Nielsen OA, Borum P (1994) Hearing loss after neurosurgery. The influence of low cerebrospinal fluid pressure. J Laryngol Otol 108:637–641
Watanabe E, Schramm J, Strauss C, Fahlbusch R (1989) Neurophysiologic monitoring in posterior fossa surgery. II. BAEP-waves I and V and preservation of hearing. Acta Neurochir (Wien) 98:118–128
Ying T, Thirumala P, Shah A et al (2013) Incidence of high-frequency hearing loss after microvascular decompression for hemifacial spasm. J Neurosurg 118:719–724
Youn J, Kwon S, Kim JS, Jeong H, Park K, Cho JW (2013) Safety and effectiveness of microvascular decompression for the treatment of hemifacial spasm in the elderly. Eur Neurol 70:165–171
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Additional information
Comments
Marc Sindou and Andrei Brinzeu, Lyon, France
Authors report the postoperative complications that they observed after micro-vascular decompression (MVD) for hemifacial spasm (HFS), together with putative mechanisms. Results are impressive both in terms of number of patients treated and quality of outcome. Preoperative assessment of the patients, technical means engaged during surgery, and postoperative evaluation were most rigorous. Scope of types of complications is very similar to the ones encountered in literature and our personal practice. As regarding main complications, general consensus to reduce harmful consequences of MVD can be expressed as follows.
Immediate facial palsies are often related to surgical insults, especially coagulation of—even the tiniest—vessels (vasa nervorum) located at the REZ; these are little propitious to recover. Also, neocompression of the nerve by the inserted material may be responsible; when suspected, early reoperation may be justified. Free-running EMG monitoring of the facial nerve might be of some help to provide warning signals of the nerve suffering in “delicate “ cases, especially when an atheromatous megadolicho-artery (predicted on imaging) is the conflict.
Decrease in hearing is less prone to happen if trajectory to the ventro-caudal aspect of the facial REZ is infrafloccular without stretching of the eighth nerve. Most reliable warning of BEAP monitoring is an increase in latency of peak V approaching 1 ms. Release of retraction and rectification in trajectory generally obtains prompt reversibility. Loss of hearing can also be due to cochlear ischemia due to manipulation of the anterior superior cerebellar artery and/or its labyrinthine branch. Warning on BEAP is sudden decrease in amplitude of peak I. When vasospasm is observed, topical application of a few droplets of papaverine (10 % in saline) constantly reverses spasm within a minute or so. Because of the very acid pH of papaverine only, a few droplets should be applied. Regular warm saline irrigation is important to avoid drying of the (fragile) neural structures of the CPA. BEAP monitoring at least during the learning curve period, if not constantly, is of valuable practical help.
CSF leakage may occur and lead to rhinorrhea and meningitis when mastoid air cells are widely opened. Closure of dura and occlusion of cells can be secured by using an aponevrotic patch and fat tissue, respectively. To avoid on-site harmful harvesting with risk of occipital nerve injury, small pieces of fascia lata and fat can be taken from the thigh.
As shown by the authors, provided careful and meticulous surgical maneuvers are performed, MVD for HFS is the more so as justified as it is at present the sole curative treatment available.
Min Ho Lee and Tae Keun Jee contributed equally to this work.
Rights and permissions
About this article
Cite this article
Lee, M.H., Jee, T.K., Lee, J.A. et al. Postoperative complications of microvascular decompression for hemifacial spasm: lessons from experience of 2040 cases. Neurosurg Rev 39, 151–158 (2016). https://doi.org/10.1007/s10143-015-0666-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10143-015-0666-7