Abstract
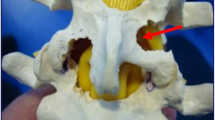
Large lumbosacral disc herniations causing bi-radicular symptoms are very rare clinical entities and may present a surgical challenge. This study was undertaken to evaluate the effectiveness of the simply modified combined lateral and interlaminar approach for the treatment of these unique disc herniations. Between 2000 and 2005, 18 patients with bi-radicular symptoms secondary to large disc herniations of the lumbar spine underwent surgery. There were 13 men and five women, ranging in age between 25 and 64 years (mean 54.3 years). In this three-step operation, the osseous areas that are not essential for the facet joint were removed and both upper and lower nerve roots were decompressed. There were no intraoperative or postoperative complications, except transient dysesthesia in one (5.5%) patient. The mean follow-up period was 62.6 months (range 36–96 months). At the latest follow-up examination, outcomes using the Macnab classification were excellent in 13 patients (72.2 %), good in four (22.2%) and fair in one (5.5%). Recurrent disc herniations and/or instability, either symptomatic or radiographic, have not occurred as a result of the procedure during the follow-up period. The combined approach described here is a safe and effective procedure in the surgical treatment of this subtype of disc herniations with bi-radicular involvement. It permits optimum decompression of both nerve roots, avoiding the risk of secondary spinal instability.




Similar content being viewed by others
References
Abdullah AF, Wolber PGH, Warfield JR, Gunadi IK (1998) Surgical management of extreme lateral lumbar disc herniations: review of 138 cases. Neurosurgery 22:648–653
Darden BV, Wade JF, Alexander R, Wood KE, Rhyne AL, Hicks JR (1995) Far lateral disc herniations treated by microscopic fragment excision: techniques and results. Spine 20:1500–1505
Di Lorenzo N, Porta F, Onnis G, Cannas A, Arbau G, Maleci A (1998) Pars interarticularis fenestration in the treatment of foraminal lumbar disc herniation: a further surgical approach. Neurosurgery 42:87–89
Ditsworth DA (1998) Endoscopic transforaminal lumbar discectomy and reconfiguration: a postero-lateral approach into the spinal canal. Surg Neurol 49(6):588–597
Donaldson WF, Star MJ, Thorne RP (1993) Surgical treatment for the far lateral herniated lumbar disc. Spine 18:1263–1267
Ebeling U, Reulen HJ (1983) Lateral lumbar intervertebral disk prolapse: a case series [in German]. Nervenartz 54:521–524
Epstein NE (1995) Evaluation of varied surgical approaches used in the management of 170 far-lateral lumbar disc herniations: indications and results. J Neurosurg 83:648–656
Epstein NE (2002) Foraminal and far lateral lumbar disc herniations: surgical alternatives and outcome measures. Spinal Cord 40:491–500
Epstein NE (2003) Far lateral and foraminal lumbar disc herniations. In: Batjer HH, Loftus CM (eds) Neurological Surgery. Principles and Practice. Lippincott Williams & Wilkins, Philadelphia, pp 1661–1668
Faust SE, Ducker TB, VanHassent JA (1992) Lateral lumbar disc herniations. J Spinal Disord 5:97–103
Frankhauser H, de Tribolet N (1987) Extreme lateral lumbar disc herniation. Br J Neurosurg 1:111–129
Garrido E, Connaughton PN (1991) Unilateral facetectomy approach for lateral lumbar disc herniation. J Neurosurg 74:754–756
Haher TR, O’Brien MF, Dryer JW, Nucci R, Zipnik R, Leone DJ (1994) The role of lumbar facet joints in spinal instability: identification of alternative paths of loading. Spine 19:2667–2671
Hassler W, Brandner S, Slansky I (1996) Microsurgical management of lateral lumbar disc herniations: combined Lateral and interlaminar approach. Acta Neurochir (Wien) 138:907–911
Witzmann A, Hergan K, Hassler W (2001) Combined transarticular lateral and medial approach with partial facetectomy for lumbar foraminal stenosis. J Neurosurg (Spine 1) 96:118–121
Hodges SD, Humphreys SC, Eck JC, Covington LA (1999) The surgical treatment of far lateral L3–L4 and L4–l5 disc herniations: a modified technique and outcomes analysis of 25 patients. Spine 24(12):1243–1249
Hood RS (1993) Far lateral lumbar disc herniations. Neurosurg Clin North Am 4(1):117–124
Huber P, Reulen HJ (1989) CT observations of the intra- and extracanalicular disc herniation. Acta Neurochir (Wien) 100:3–11
Jane JA, Haworth CS, Broaddus WC, Lee JH, Malik J (1990) A neurosurgical approach to far-lateral disc herniation. Technical note. J Neurosurg 72:143–144
Kambin P, Casey K, O’Brien E, Zhou I (1996) Transforaminal arthroscopic decompression of lateral recess stenosis. J Neurosurg 84(3):462–471
Kirkaldy-Willis WH (1984) The relationship of structural pathology to the nerve root. Spine 9:49–52
Kunogi J, Hasue M (1991) Diagnosis and operative treatment of intraforaminal and extraforaminal nerve root compression. Spine 16:1312–1320
Lanzino G, Shaffrey CI, Jane JA (1999) Surgical treatment of lateral lumbar herniated discs. In: Rengachary SS, Wilkins RH (eds) Neurosurgical Operative Atlas, vol 8. Williams & Wilkins, Philadelphia, pp 243–251
Macnab I (1971) Negative disc exploration. An analysis of the causes of nerve root involvement in sixty-eight patients. J Bone Joint Surg (Am) 53:891–903
Markwalder TM, Reulen HJ (1989) Diagnostic approach in instability and irritative state of a ‘lumbar motion segment’ following disc surgery: failed back surgery syndrome. Acta Neuochir (Wien) 99:51–57
Markwalder TM, Reulen HJ (1989) Translaminar screw fixation in lumbar spine pathology. Acta Neurochir (Wien) 99:58–60
Maroon JC, Kopitnik TA, Schulhof LA, Abla A, Wilberger JE (1990) Diagnosis and microsurgical approach to far-lateral disc herniation in the lumbar spine. J Neurosurg 72:378–382
Melvill RL, Baxter BL (1994) The intertransverse approach to extraforaminal disc protrusion in the lumbar spine. Spine 19:2707–2714
Müller A, Reulen HJ (1998) A paramedian tangential approach to lumbosacral extraforaminal disc herniations. Neurosugery 43(4):854–861
O’Brien MF, Peterson D, Crockard HA (1995) A posterolateral microsurgical approach to extreme-lateral lumbar disc herniation. J Neurosurg 83:636–640
Oeckler R, Hamburger C, Schmiedek P, Haberl H (1992) Surgical observations in extremely lateral lumbar disc herniation. Neurosurg Rev 15:255–258
Paolini S, Ciappetta P, Raco A, Missori P, Delfini R (2006) Combined intra-extracanal approach to lumbosacral disc herniations with bi-radicular involvement. Technical considerations from a surgical series of 15 cases. Eur Spine J 15:554–558
Porchet E, Chollet-Bornand A, de Tribolet N (1999) Long term follow up of patients surgically treated by the far lateral approach for foraminal and extraforaminal lumbar disc herniations. J Neurosurg (Spine 1) 90:59–66
Postacchini F, Cinotti G, Gumina S (1998) Microsurgical excision of lateral lumbar disc herniation through an interlaminar approach. J Bone Joint Surg (Br) 80-B:201–B207
Recoules-Arche D (1985) Surgery of disk hernia of the lumbar vertebral canal. [in French]. Neurochirurgie 31:61–64
Reulen HJ, Müller A, Ebeling U (1996) Microsurgical anatomy of the lateral approach to extraforaminal lumbar disc herniations. Neurosurgery 39(2):345–351
Reulen HJ, Pfaundler S, Ebeling U (1987) The lateral microsurgical approach to the ‘extracanalicular’ lumbar disc herniation. I: a technical note. Acta Neurochir (Wien) 84:64–67
Schlesinger SM, Frankhauser H, de Tribolet N (1992) Microsurgical anatomy and operative technique for extreme lateral lumbar disc herniations. Acta Neurochir (Wien) 118:117–129
Siebner HR, Faulhauer K (1990) Frequency and specific surgical management of far lateral lumbar disc herniations. Acta Neurochir (Wien) 105:124–131
Sturm PF, Armstrong GW, O’Neil DJ, Belanger JM (1992) Far lateral lumbar disc herniation treated with anterolateral retroperitoneal approach: report of two cases. Spine 17:363–365
Viswanathan R, Swamy NK, Tobler WD, Greiner AL, Keller JT, Dunsker SB (2002) Extraforaminal lumbar disc herniations: microsurgical anatomy and surgical approach. J Neurosurg (Spine 2) 96:206–211
Wiltse LL, Bateman JG, Hutchinson RH, Nelson WE (1968) The paraspinal sacrospinalis-splitting approach to the lumbar spine. J Bone Joint Surg (Am) 50A:919–926
Wiltse LL, Spencer CW (1988) New uses and refinements of the paraspinal approach to the lumbar spine. Spine 13:696–706
Zindrick MR, Wiltse LL, Rauschning W (1987) Disc herniations lateral to the intervertebral foramen. In: White AH, Rothman RH, Ray CD (eds) Lumbar Spine Surgery. Techniques and Contoversies. CV Mosby, St. Louis, pp 195–207
Author information
Authors and Affiliations
Corresponding author
Additional information
Comments
Mehmet Daneyemez, Ankara, Turkey
Present paper reported the experience in a clinic of 18 patients who underwent the combined intertransverse–interlaminar approach to large disc herniations with paramedian and lateral extensions that compressed the upper and lower nerve roots related to the disc space, as described. According to their findings, modified combined lateral and interlaminar approach was defined as ‘safe and effective procedure’ in the surgical treatment of the large disc herniations in properly selected patients.
I have been affected by the technique described in the text though it included slight differences from those which were described previously by numerous authors, because the operational technique has been described very clearly and moreover, it is clinically practical rather than just being a postulation with constricted experimental use.
Traditional techniques consisted usually of complete removal of the facet for decompression of the spinal canal and exploration of the intervertebral foramen. This inevitably frequently resulted in spinal instability. Consequently, additional posterolateral fusion is required adding morbidity and prolonged hospital stay. However, with the use of this surgical combined approach, affected nerve roots can be explored and decompressed without giving much harm to normal facet joint. Keeping the integrity of pars interarticularis sparing the lateral portion of the pars in tricortical structure will rationally enhance to decreasing the risk of spinal instability.
Approach to the L5–S1 intervertebral intertransverse pathologies seems to necessitate drilling the para-articular notch.
The goal of the aforescribed surgical technique was preservation of the pars interarticularis and the major part of the facet joint and I had the practical sense that the described approach is a successful trial and deserve appreciation as applied to properly selected group of patients.
Jack Jallo, Philadelphia, USA
The authors in this article report on their surgical experience in 18 patients over a 5-year period who underwent a combined intertransverse–interlaminar approach to large disc herniations that compressed the upper and lower nerve roots with a mean follow-up of 62.6 months.
The technique described is a simple and well-illustrated modification of previously reported surgical techniques that allows exploration of the affected roots without disruption of the facet joint. They report good outcomes in 72.2% of patients over the follow-up period and no instability or recurrent disc herniations.
In summary, the authors present an interesting and new approach to technically challenging disc herniations in a small series of patients.
Ernst Delwel, Rotterdam, the Netherlands
The authors have produced a useful article on a unique combined approach for a subgroup of patients with a bi-radicular syndrome caused by a lateral lumbar disc herniation.
This subgroup consisted of 2.1% of the total amount of patients with a symptomatic lumbar disc herniation that were operated in the period of 2000–2005. A meticulous description is given of the operative procedure and the authors have explained the indication for this technique thoroughly. They have to be complemented with their good results, even after a long follow-up period and their very low complication rate.
Before using this new and rather complex technique, a training period on anatomic specimen in the lab would be advisable to my opinion. Furthermore, I would like to emphasise to use peroperative neuronavigation or at least peroperative fluoroscopy to prevent exploring the wrong level.
Luciano Mastronardi, Rome, Italy
Disc herniations with bi-radicular involvement are rare and the optimal approach should allow the total removal of the fragments and avoid further vertebral instability.
The authors propose an interesting combined lateral and interlaminar approach, sparing the joints and, thus, preserving the stability. The good results seem to confirm that this three-step procedure is a valid proposal for this kind of procedure. Prospective studies on larger should be warranted.
Rights and permissions
About this article
Cite this article
Kutlay, M., Topuz, K., Çolak, A. et al. Management of disc herniations with bi-radicular symptoms via combined lateral and interlaminar approach. Neurosurg Rev 33, 97–105 (2010). https://doi.org/10.1007/s10143-009-0218-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10143-009-0218-0