Abstract
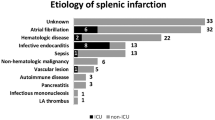
Acute splenic infarcts classically present with left upper quadrant pain, but may be discovered incidentally in many hospitalized patients with otherwise vague complaints. The purpose of our study was to document causes or predisposing conditions in patients found to have acute splenic infarctions on imaging. Following IRB approval, a retrospective review of an imaging database from May 2008 to May 2015 was performed for cases of acute splenic infarctions. The electronic medical record was then reviewed for potential predisposing factors or known causes. Specific note was made of cases with active malignancy, vascular disorders, or inflammatory conditions with an increased risk of vasculopathy. Echocardiogram and electrocardiogram results were reviewed when available. One hundred twenty-three patients with acute splenic infarcts were identified, 65 female and 58 male. The average age was 57 years (range of 22 to 88). Active malignancy was present in 40 patients or 33 %. The most common malignancy in patient with nontraumatic splenic infarctions was pancreatic cancer, present in 16 patients (13 %). In these patients, splenic infarction was due to direct invasion of vessels in the splenic hilum. Acute pancreatitis (severe) was directly responsible for splenic infarction in seven additional cases (6 %). Additional visceral infarcts were present in 18 patients (15 %), most commonly concomitant hepatic or renal infarcts. Documented atrial fibrillation was present in 12 patients, but only 2 cases of left-sided cardiac thrombi were seen on CT (1 atrial, and 1 ventricular thrombus). Eight cases of endocarditis with valvular vegetations were documented on echocardiography (7 %). Splenomegaly was present in 32 patients (26 %) with acute splenic infarction. In patients with nontraumatic splenic infarctions, there appears to be a relatively high association with active malignancy (up to a third of patients). Pancreatic disorders, malignant and inflammatory, also appear to be an important cause of splenic infarction, presumably due to the close proximity of the pancreas to the splenic vessels.


Similar content being viewed by others
References
Lawrence Y, Pokroy R, Berlowitz D et al (2010) Splenic Infarction: an update on William Osler’s observations. Israeli Med Assoc J 12:362
Catalano O, Cusati B, Nunziata A et al (2004) Real-time, contrast-specific, sonography of acute splenic disorders: pictorial review. Emerg Radiol 11:15–21
Tonolini M, Bianco R (2013) Nontraumatic splenic emergencies: cross-sectional imaging findings and triage. Emerg Radiol 20:323–332
Gayer G, Galperin-Eizenberg M (2008) Iatrogenic splenic injuries in postoperative patients: a series of case reports. Emerg Radiol 15:109–113
Sanon S, Lenihan D, Mouhayar E (2010) Peripheral arterial ischemic events in cancer patients. Vasc Med 16:119–130
Thomas R (2001) Hypercoagulability syndromes. Arch Intern Med 161:2433–2439
Kakkar A, DeRuvo N, Chinswangwatanakul V et al (1995) Extrinsic-pathway activation in cancer with high factor VIIs and tissue factor. Lancet 346:1004–1005
Pinzon R, Drewinko B, Trujillo J et al (1986) Pancreatic cancer and Trousseau’s Syndrome: experience at a large cancer center. J Clin Oncol 4:509–514
Nores M, Phillips E, Morgenstern L et al (1998) The clinical spectrum of splenic infarction. Am Surg 64:182–188
Gorg C, Gorg K (2004) Acute, complete splenic infarction in cancer patients is associated with a fatal outcome. Abdom Imaging 29:224–227
Rao VM, Levin DC, Parker L et al (2011) Trends in utilization of various imaging modalities in emergency departments: nationwide Medicare data from 2000–2008. J Am Coll Radiol 8:706–709
Howlader N, Noone A, Krapcho M, et al. SEER Cancer Statistics Review, 1975–2012. National Cancer Institute, Bethesda, MD. http://seer.cancer.gov/csr/ Accessed 11/28/2015.
Cox M, Balasubramanya R, Hou A et al (2015) Incidental left atrial and ventricular thrombi on routine CT: outcome and influence on subsequent management at an urban tertiary care referral center. Emerg Radiol 22:657–660
Schwartz S, Stubbs A, Taljanovic M et al (2008) Pancreatitis-associated splenic vein thrombosis with intrasplenic venous thrombosis: a case report. Emerg Radiol 15:433–436
Agarwal M, Levenson R, Siewert B et al (2015) Limited utility of performing follow-up contrast-enhanced CT in patients undergoing initial non-enhanced CT for evaluation of flank pain in the emergency department. Emerg Radiol 22:109–115
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
IRB statement
This retrospective review study was approved by the Thomas Jefferson University Hospitals Institutional Review Board.
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Cox, M., Li, Z., Desai, V. et al. Acute nontraumatic splenic infarctions at a tertiary-care center: causes and predisposing factors in 123 patients. Emerg Radiol 23, 155–160 (2016). https://doi.org/10.1007/s10140-016-1376-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10140-016-1376-3