Abstract
Methodology for the diagnosis and staging of early gastric cancer (EGC) has improved in Japan since the development of the gastro-camera and determination of a definition of EGC. Imaging technology has been steadily evolving in the endoscopy field. Improvements in the resolution of standard endoscopy images used in screening and surveillance provide greater opportunities to find gastric cancer earlier. Image enhancement endoscopy (IEE), such as narrow band imaging (NBI), highlights mucosal structures and vascularity. In particular, when NBI is used with magnifying endoscopy, it reveals fine details of subtle superficial abnormalities of EGC that are difficult to recognize using standard white light endoscopy. IEE-assisted magnifying endoscopy has improved the accuracy of the differentiation of superficial gastric cancer as well as delineation of the diseased mucosa. The advanced imaging technology enables precise assessment of the risk of lymph node metastasis of EGC and is widely used to determine indications for endoscopic treatment. It is not an overstatement to say that this has become the basis for the current development and dissemination of endoscopic treatments. Moreover, the resolution of endoscopic imaging has been upgraded to the microscopy level by the development of endomicroscopy, including endocytoscopy and confocal laser endomicroscopy. Endomicroscopy allows real-time histological analysis of living tissue during routine endoscopy and may reduce the number of biopsies needed to reach the correct diagnosis, minimizing the risk of sampling errors.
Similar content being viewed by others
Introduction
The macroscopic classification of early gastric cancer (EGC) was proposed by the Japanese Endoscopy Society on the basis of contrast radiography and gastro-camera findings in 1962. The original macroscopic classification for EGC is still used as the basis of endoscopic assessment for EGC, with minor modifications. For example, in the current Japanese macroscopic classification of gastric cancer [1], superficial-type gastric cancers (type 0) are grossly subclassified into type 0-I (polyploid lesions protruding more than 3 mm), type 0-IIa (slightly elevated lesions protruding less than 3 mm), type 0-IIb (flat lesions), type 0-IIc (slightly depressed lesions), and type 0-III (excavated lesions with a deep depression). In order to find gastric cancer earlier, endoscopists first need to know what EGC looks like under white light endoscopy. Typical endoscopic findings have been analyzed for different pathologic subtypes of gastric cancer (intestinal or diffuse) for each macroscopic type.
Innovations in endoscopic imaging have made it possible to clearly describe subtle morphological changes in superficial cancers that are difficult to recognize using standard white light endoscopy. In recent decades, an array of novel optical image enhancement endoscopy (IEE) technologies [i.e., narrow band imaging (Olympus Medical System, Tokyo, Japan), blue light imaging (Fujifilm, Tokyo, Japan), and i-scan (Hoya-Pentax, Tokyo, Japan)] have been developed to analyze surface tissue structures in detail. Endoscopists can readily switch to IEE from white light endoscopy at will using a button on the scope during routine endoscopy as an alternative to chromoendoscopy. The combined use of magnifying endoscopy and IEEs also highlights irregularities of surface structures, including the superficial capillary network of EGC [2]. As a consequence of the technological developments and improvements in diagnostic accuracy, endoscopy plays a more important role not only in the detection and characterization of mucosal abnormalities, but also in delineation and depth assessment to determine T-staging and therapeutic indications for EGC. The improved detection rate of EGCs has resulted in an increased opportunity for their endoscopic excision. Indeed, endoscopic tissue resection has become one of first-line therapeutic options for EGC in countries with a high prevalence of gastric cancer. Furthermore, in vivo analysis of EGC at the cellular level is technologically possible by using endomicroscopy technologies with image resolution equivalent to bench-top microscopy.
Detecting gastric cancer earlier
The quality of endoscopic imaging has improved markedly, facilitating the detection of gastric cancer at earlier stages. The development of the gastro-camera enabled EGCs to be photographed and has greatly reduced the burden, for both patients and endoscopists, associated with endoscopic investigations compared with investigations during the rigid scope era. The totally flexible fiberoptic scope revolutionized the diagnostic ability of endoscopy, the etiologic analysis of gastrointestinal (GI) diseases, including gastric cancer, and screening methods of the stomach, tissue sampling, and education. Currently, high-definition video-endoscopes are used across Japan as the standard for gastric cancer surveillance (Figs. 1, 2a, 3a, 4a). Ichikawa et al. reported that at the National Cancer Center Hospital in Tokyo, between 1962 and 1968, only 19.5 % of gastric cancers were found at an early stage using contrast radiography and the gastro-camera [3]. Ichikawa et al. also reported that the overall 5-year survival rate for gastric cancer was 36.7 %, even though the rate for EGC at the same time was 90.3 %, and increased to 96.6 % when non-cancer-related deaths were excluded. According to nationwide population-based data in Japan for the period 2006–08 [4], more than half of all gastric cancers were classified as EGC at the time of diagnosis, and the overall 5-year survival rate for gastric cancer was over 60 %. The improvement in the survival rate for gastric cancers in Japan seems to be attributable to the unique social environment: specifically, gastric cancer has been one of most common causes of cancer-related deaths because of the high rate of infection with Helicobacter pylori; mass screening with standardized contrast radiography has been practiced since the 1960s; many private practices provide ready access to endoscopy. From a global perspective, there is significant geographical diversity in the incidence of EGC and the survival rate for gastric cancer. In the US, most gastric cancers are found as advanced disease, and the overall 5-year survival rate is less than 30 % [5]. Recently, a 15-year follow-up population-based cohort study performed in Japan revealed that gastric cancer mortality was reduced by 67 % by endoscopic screening compared with radiographic screening [6].
Endoscopic images of an early stage undifferentiated or diffuse-type adenocarcinoma of the stomach acquired at different times using different imaging systems (images courtesy of Prof. Hisao Tajiri). a Image taken using a gastro-camera with a fiberoptic system in the 1970s. b Image taken using a fiberoptic scope in the 1980s. c Image obtained in the 1990s using a video endoscope
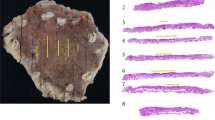
A small undifferentiated or diffuse-type early gastric cancer invading into the submucosa. a Standard white light endoscopy image showing a small depressed lesion <10 mm in diameter located in the anterior wall of the lower body of the stomach. The lesion was associated with submucosal tumor-like elevation at the margins. b Vascular findings on magnifying endoscopy with narrow band imaging revealed a “corkscrew pattern,” and the lesion was diagnosed as a diffuse-type cancer. c High-frequency endoscopic ultrasonography (EUS; 20 MHz) showing cancer invasion into the shallow submucosa. d Histopathology. The tumor was a 9 × 6-mm 0-IIc-type cancer. Signet ring cell carcinoma had invaded into the shallow submucosal layer
Endoscopic images of a differentiated or intestinal-type mucosal cancer of the stomach. a Standard white light endoscopy image showing a slightly depressed lesion approximately 20 × 10 mm in size located at the posterior wall of the upper body of the stomach. b A chromoendoscopic image of the lesion obtained using acetic acid-indigo carmine, which highlighted the lesion as an isolated reddish area. c Magnifying endoscopy with narrow band imaging of the lesion revealed absent and irregular microsurface patterns within the depressed area. The delineation of the irregular findings was clearly recognized as a demarcation line (arrows). d The microvascular structure exhibited a fine network pattern at a higher magnification level
High-definition endoscopy images of an early stage undifferentiated or diffuse-type adenocarcinoma of the stomach. a Standard white light endoscopy image of the lesion. The lesion was whitish, slightly depressed (0–IIc), well demarcated, approximately 20 × 10 mm in size, and located at the greater curvature of the mid body. b Magnifying endoscopy with narrow band imaging of the lesion revealed absent and irregular microsurface patterns within the depressed area. The microvascular structure exhibited a corkscrew pattern. c High-frequency endoscopic ultrasound shows the cancer (arrows) invading into the submucosa (the hyperechoic third layer from the top). d Confocal laser endomicroscopy (CLE) of the lesion revealed disappearance of glandular structures and the appearance of small black spots, which are typical CLE findings in undifferentiated type or diffuse-type gastric cancers. e Histopathology showing signet ring cell cancer invading deep into the submucosal layer (up to 1250 μm from the muscularis mucosa)
In order to clarify the contribution of the currently available endoscopic imaging technologies to the detection of EGC, two randomized controlled trials were conducted at Jikei University to compare three different types of endoscopy systems [7, 8]: (1) white light endoscopy with a high-definition scope (GIF H260Z, Olympus Medical Systems, Tokyo); (2) white light endoscopy with an ultra-thin scope (GIF-XP260 N, Olympus Medical Systems, Tokyo); (3) IEE [NBI and autofluorescent imaging (AFI) with a high-definition scope]. In these studies, the rate at which EGC was overlooked was analyzed in a case-enriched population in which patients with superficial gastric neoplasia referred for endoscopic submucosal dissection (ESD) were mixed with patients who were undergoing follow-up endoscopy after ESD as neoplasia-free controls. Between 22 and 23.4 % of EGCs were overlooked, and, surprisingly, the rate increased to 42.5 % when the ultra-thin scope was used. In contrast, the combination of magnifying endoscopy and NBI/AFI successfully reduced the rate to 6.4 %. Although these findings demonstrate the substantial contribution that technological progress in the endoscopy field has made to the detection of gastric cancers earlier, as well as to improvements in survival rate, the risk of overlooking EGC remains.
Chromoendoscopy with topical application of an indigo carmine solution is widely used to improve the screening effect at minimal extra expense [9]. Indigo carmine does not stain tissues directly, but enables visualization of the superficial topography by filling the pits and grooves on the mucosa, as well as contouring elevated areas. In addition, the combined use of indigo carmine and acetic acid improves the visualization and detection of EGC [10–12]. In the presence of acetic acid, it appears that the indigo carmine is washed out earlier from cancerous mucosa than from the surrounding non-cancerous mucosa with mucin secretion (Fig. 3b). In particular, there is a greater chance of distinctly delineating differentiated adenocarcinomas as reddish areas using this technique. Kawahara et al. also reported that the accuracy of EGC delineation was better for acetic acid-assisted chromoendoscopy than for white light endoscopy [13]. Although there is a paucity of reliable data for the effectiveness of mass screening, one meta-analysis concluded that chromoendoscopy has better diagnostic accuracy than white light endoscopy [11].
Differential diagnosis and delineation with IEE
After the identification of mucosal abnormalities, a differential diagnosis needs to be made to diagnose EGC. Because pathology is the relative standard for the final diagnosis of cancers, differential diagnosis in endoscopic examinations has overwhelmingly relied on forceps biopsies from the abnormal areas, when found. However, it is impossible to completely eliminate the risk of sampling errors from the target biopsy. In addition, there is often a discrepancy between biopsy-based diagnoses and the final pathological diagnosis. A meta-analysis of 16 studies involving 3303 cases showed that 25 % of forceps biopsy-proven gastric low-grade dysplasia (LGD) lesions were upgraded to more advanced lesions, including gastric high-grade dysplasia (HGD; 16.7 %) and gastric carcinoma (6.9 %), after endoscopic resection [14]. This emphasizes the importance of image-based diagnoses in achieving an accurate diagnosis of EGC. A series of studies demonstrated that the combined use of magnifying endoscopy and IEEs was useful in discriminating cancerous from non-cancerous mucosa [15–19]. Most of these studies investigated NBI-assisted diagnoses. In NBI, blue (415 nm) and green (540 nm) light is selectively emitted to tissues through a narrow band filter at the tip of the scope. Therefore, observations for NBI are inevitably darker than those for white light endoscopy and are suboptimal for surveillance of the stomach with a spatial lumen and a complex anatomy, with broad variation among individuals. Although a newer version of NBI provides brighter images, reliable evidence to prove the improvement has not been available. The light of specific wavelengths used in NBI is absorbed by hemoglobin. Thus, vascular structures are distinctively enhanced as dark linear structures in NBI. The green light, with a shorter wavelength, reflects at the shallower level and preferentially visualizes the superficial capillary network, whereas the blue light, with a longer wavelength, penetrates deeper and enables visualization of the vasculature at the subsurface level. Characterization of superficial lesions in the stomach could be challenging because the background non-cancerous mucosa can be affected, to varying degrees, by atrophic and/or intestinal metaplastic changes triggered by H. pylori infection. The VS (vascular and surface pattern) classification proposed by Yao et al. [20, 21] is the most commonly used structured classification to characterize superficial gastric lesions. In the VS classification system, in order to maximize the technological advantages of NBI and simplify the diagnostic process, the mucosal surface patterns and vascular architecture are evaluated separately. When both the irregular microvascular pattern (IMVP) and irregular microsurface pattern (IMSP) are observed on the lesion with a demarcation line (DL) (Table 1; Fig. 3c), which describes the front line of the lateral expansion of the cancer [22], the lesion meets the criteria for gastric cancer. Nakayoshi et al. also revealed that changes to the capillary network structures encircling gastric gland openings are correlated with the deformation and misalignment of glandular structures. Nakayoshi et al. [23] subdivided the microvascular pattern into two types, namely a fine network pattern (mesh formation; Fig. 3c, d) and a corkscrew pattern (tortuous with a lack of connections; Figs. 2b, 4b). The fine network pattern is more frequently observed in intestinal-type cancer, whereas the corkscrew pattern is predominantly observed in diffuse-type cancer. Recently, an algorithm for magnifying the endoscopy diagnosis of EGC was proposed by the Japanese Gastric Cancer Association (JGCA), the Japan Gastroenterological Endoscopy Society (JGES), and the World Endoscopy Organization [19] with the aim of establishing a simple, standardized systemic algorithm for the diagnosis of EGC diagnosis, unifying existing criteria, and using an evidence-based approach. This algorithm, the Magnifying Endoscopy Simple Diagnostic Algorithm for Early Gastric cancer (MESDA-G), is shown in Table 1.
Depth diagnosis of EGC
The risk of lymph node metastasis of gastric cancer is determined by the size, pathological type, and depth of the lesion, the presence or absence of ulceration, and vascular cancer involvement. Thus far, preoperative assessment of vascular involvement is technically impossible. Therefore, endoscopic staging of EGC should be focused on the assessment of other factors. Classically, the depth of cancer invasion has been estimated by morphologically and dynamically evaluating the elasticity and thickness of the lesion with endoscopy and contrast radiography [24] (Table 2), because the gastric wall becomes more solid and thicker as the depth of cancer invasion increases. Endoscopic ultrasound (EUS) is the sole technology that can provide anatomical information regarding the layered structures in the gut wall and the extraluminal organs, including lymph nodes. Therefore, EUS has been widely used for T and N staging of gastric cancer on a day-to-day basis for many years. Using a high-frequency miniature ultrasound probe-type EUS provides vertical images of finer details of cancer invasion (Figs. 2, 4). Mouri et al. reported that EUS was useful for identifying shallow submucosal invasion of EGC [25]. However, the advantage of EUS in T staging of EGC remains contentious. One systematic review analyzing 18 selected papers demonstrated that the sensitivity and specificity of EUS in detecting cancer invasion deeper than the submucosa were in the range 18.2–100 % (median 87.8 %) and 34.7–100 % (median 80.2 %), respectively [26]. In addition, Choi et al. demonstrated that EUS was not superior to white light endoscopy in terms of determining the depth of cancer invasion in patients with suspected EGC (67.4 vs 73.7 %, respectively; n = 955) [27]. At the very least, endoscopists need to recognize that accurate determination of the depth of invasion with EUS could be difficult if the lesion is larger than 5 cm and associated with an ulcer scar [28–30].
Endomicroscopy
Endomicroscopy is an aptly named emerging endoscopic imaging technology enabling real-time cellular-level imaging of living tissues with a resolution at the microscopic level. Two different endomicroscopy systems, endocytoscopy and confocal laser endomicroscopy (CLE), have been examined clinically so far. Endocytoscopy consists of a contact optical microscope integrated at the tip of the endoscope, whereas CLE makes use of a confocal laser microscope miniaturized to accommodate a flexible endoscope. The eventual goal of endocytoscopy is to establish a histological diagnosis of neoplasia during routine endoscopy, minimizing the risk of sampling errors inherently associated with forceps biopsy and reducing the number of biopsies needed to reach a correct diagnosis. The vast majority of human tissues are colorless, except for pigments such as hemoglobin and melanin. Therefore, tissue staining using optimal dyes is necessary to visualize GI tissues with an endomicroscope (i.e., ultra-high magnifying endoscopy with a short focal distance). There are few reports of endomicroscopy of gastric lesions at present. Kaise et al. examined the effectiveness of endocytoscopy in differentiating EGC from non-cancerous superficial lesions using original diagnostic criteria [31]. The sensitivity, specificity, and positive and negative predictive values of endocytoscopy for a diagnosis of EGC were 86, 100, 100, and 94 %, respectively. In that study, a mixture of crystal violet and methylene blue was applied topically onto the target mucosa. However, optimal tissue staining was not achieved in 10 of 82 attempts and resulted in failure of interpretation [31].
The confocal microscopy system increases the resolution and contrast of microscopic images by using a spatial filter in the confocal plane of the lens eliminating out-of-focus noises (Fig. 4d). Therefore, CLE has advantages particularly in observations of thick objects, like the gastric wall. There are two types of CLE platforms, a scope-embedded type (eCLE) and a miniature probe type (pCLE), which can be passed through an accessary channel of a regular diagnostic scope. eCLE provides a relatively wider field of view and enables acquisition of image information at different depths, allowing three-dimensional image reconstruction. Meanwhile, pCLE provides a higher flame rate and can be used anytime, anywhere during standard endoscopy procedures. The imaging probe of a pCLE can also be passed through an endoscopic retrograde cholangiopancreatography (ERCP) catheter and even a puncture needle. At present, pCLE is the only commercially available CLE system in Japan. Bok et al. compared the accuracy of endoscopic forceps biopsy and pCLE for the diagnosis of superficial gastric neoplasia [32]. Overall agreement with the final diagnosis based on pathological analysis of specimens sampled by endoscopic resection was significantly higher for pCLE than traditional forceps biopsy diagnosis, and the overall accuracy of pCLE-based diagnosis of adenocarcinoma was 90.7 %. In addition, Li et al. demonstrated that in the diagnosis of superficial gastric cancer or high-grade intraepithelial neoplasia (HGIN), eCLE had higher sensitivity (88.9 %), specificity (99.3 %), and accuracy (98.9 %) than white light endoscopy in a large-scale prospective trial with 1572 participants undergoing eCLE, including 40 EGC and 15 HGIN cases [33]. Although these results clearly demonstrate the promise of CLE, the technology has substantial limitations. First, microscopic observation within the stomach is unstable and mobile because of respiratory fluctuations. Second, CLE requires the application of a fluorescent dye to visualize gut tissues, and fluorescein is the only clinically available stain so far. Fluorescein cannot stain nuclei; therefore fluorescein-assisted CLE diagnoses rely solely on structural atypia. Because of these disadvantages, it is anticipated that CLE will not be a viable alternative to forceps biopsy. Kobayashi et al. examined the effect of reviewers’ clinical background on the interpretation of pCLE [34] and found that gastroenterologists and Japanese reviewers achieved better outcomes than pathologists and German reviewers in discriminating neoplastic lesions from superficial gastric lesions. Previous experience with CLE and pathological training were not related to the improved diagnostic accuracy. There are still substantial discrepancies in the interpretation of results of endomicroscopy and standard histopathological analyses using fixed tissues.
Conclusions
Endoscopic imaging technology has evolved, resulting in significant improvements in the detection, differentiation, delineation, and assessment of the depth of invasion of EGC. However, novel technologies require technology-specific knowledge and skills to achieve good outcomes. In addition, novel technology is not a replacement for existing technology, and multimodal examinations tend to be more time consuming and cost more. In order to use the technologies seamlessly and more effectively, standardization of diagnostic strategies and terminology is desirable, integrating the advantages of each technology. It is also important to establish a large prospective database to clarify the socioeconomic benefits of the different technologies.
References
Japanese Gastric Cancer Association. Japanese classification of gastric carcinoma: 3rd english edition. Gastric Cancer. 2011;14:101–12.
Kaise M. Advanced endoscopic imaging for early gastric cancer. Best Pract Res Clin Gastroenterol. 2015;29:575–87.
Ichikawa H, Yamada T, Horikoshi H, Doi H, Matsue H, Tobayashi K, et al. X-ray diagnosis of early gastric cancer. Jpn J Clin Oncol. 2010;40:e1–18.
The Editorial Board of the Cancer Statistics in Japan (2016) Cancer statistics in japan 2015.
Marques-Lespier JM, Gonzalez-Pons M, Cruz-Correa M. Current perspectives on gastric cancer. Gastroenterol Clin North Am. 2016;45:413–28.
Hamashima C, Shabana M, Okada K, Okamoto M, Osaki Y. Mortality reduction from gastric cancer by endoscopic and radiographic screening. Cancer Sci. 2015;106:1744–9.
Kato M, Kaise M, Yonezawa J, Goda K, Toyoizumi H, Yoshimura N, et al. Trimodal imaging endoscopy may improve diagnostic accuracy of early gastric neoplasia: a feasibility study. Gastrointest Endosc. 2009;70:899–906.
Toyoizumi H, Kaise M, Arakawa H, Yonezawa J, Yoshida Y, Kato M, et al. Ultrathin endoscopy versus high-resolution endoscopy for diagnosing superficial gastric neoplasia. Gastrointest Endosc. 2009;70:240–5.
Uedo N, Yao K. Endoluminal diagnosis of early gastric cancer and its precursors: bridging the gap between endoscopy and pathology. Adv Exp Med Biol. 2016;908:293–316.
Numata N, Oka S, Tanaka S, Yoshifuku Y, Miwata T, Sanomura Y, et al. Useful condition of chromoendoscopy with indigo carmine and acetic acid for identifying a demarcation line prior to endoscopic submucosal dissection for early gastric cancer. BMC Gastroenterol. 2016;16:72. doi:10.1186/s12876-016-0483-7.
Zhao Z, Yin Z, Wang S, Wang J, Bai B, Qiu Z, et al. Meta-analysis: the diagnostic efficacy of chromoendoscopy for early gastric cancer and premalignant gastric lesions. Hepatol: J Gastroenterol; 2016.
Song KH, Hwang JA, Kim SM, Ko HS, Kang MK, Ryu KH, et al (2016) Acetic acid chromoendscopy for determining the extent of gastric intestinal metaplasia. Gastrointest Endosc.
Kawahara Y, Takenaka R, Okada H, Kawano S, Inoue M, Tsuzuki T, et al. Novel chromoendoscopic method using an acetic acid-indigocarmine mixture for diagnostic accuracy in delineating the margin of early gastric cancers. Dig Endosc. 2009;21:14–9.
Zhao G, Xue M, Hu Y, Lai S, Chen S, Wang L. How commonly is the diagnosis of gastric low grade dysplasia upgraded following endoscopic resection? A meta-analysis. PLoS One. 2015;10:e0132699.
Sugano K. Detection and management of early gastric cancer. Curr Treat Options Gastroenterol. 2015;13:398–408.
Dohi O, Yagi N, Majima A, Horii Y, Kitaichi T, Onozawa Y, et al (2016) Diagnostic ability of magnifying endoscopy with blue laser imaging for early gastric cancer: a prospective study. Gastric Cancer.
Tao G, Xing-Hua L, Ai-Ming Y, Wei-Xun Z, Fang Y, Xi W, et al. Enhanced magnifying endoscopy for differential diagnosis of superficial gastric lesions identified with white-light endoscopy. Gastric Cancer. 2014;17:122–9.
Yao K. The endoscopic diagnosis of early gastric cancer. Ann Gastroenterol. 2013;26:11–22.
Muto M, Yao K, Kaise M, Kato M, Uedo N, Yagi K, et al. Magnifying endoscopy simple diagnostic algorithm for early gastric cancer (MESDA-G). Dig Endosc. 2016;28:379–93.
Yao K, Oishi T, Matsui T, Yao T, Iwashita A. Novel magnified endoscopic findings of microvascular architecture in intramucosal gastric cancer. Gastrointest Endosc. 2002;56:279–84.
Ezoe Y, Muto M, Uedo N, Doyama H, Yao K, Oda I, et al. Magnifying narrowband imaging is more accurate than conventional white-light imaging in diagnosis of gastric mucosal cancer. Gastroenterology. 2011;141:2017.e3–2025.e3.
Sumiyama K, Kaise M, Nakayoshi T, Kato M, Mashiko T, Uchiyama Y, et al. Combined use of a magnifying endoscope with a narrow band imaging system and a multibending endoscope for en bloc EMR of early stage gastric cancer. Gastrointest Endosc. 2004;60:79–84.
Nakayoshi T, Tajiri H, Matsuda K, Kaise M, Ikegami M, Sasaki H. Magnifying endoscopy combined with narrow band imaging system for early gastric cancer: correlation of vascular pattern with histopathology (including video). Endoscopy. 2004;36:1080–4.
Maruyama Y, Shimamura T, Koda K, Kageoka M, Ohata A, Shimura T, et al. Diagnosis of the depth of early gastric cancer by conventional and dying endoscopy-from the view point of the size and marcroscopic type. Stomach Intestine. 2014;49:35–46 (Japanese).
Mouri R, Yoshida S, Tanaka S, Oka S, Yoshihara M, Chayama K. Usefulness of endoscopic ultrasonography in determining the depth of invasion and indication for endoscopic treatment of early gastric cancer. J Clin Gastroenterol. 2009;43:318–22.
Kwee RM, Kwee TC. The accuracy of endoscopic ultrasonography in differentiating mucosal from deeper gastric cancer. Am J Gastroenterol. 2008;103:1801–9.
Choi J, Kim SG, Im JP, Kim JS, Jung HC, Song IS. Comparison of endoscopic ultrasonography and conventional endoscopy for prediction of depth of tumor invasion in early gastric cancer. Endoscopy. 2010;42:705–13.
Akashi K, Yanai H, Nishikawa J, Satake M, Fukagawa Y, Okamoto T, et al. Ulcerous change decreases the accuracy of endoscopic ultrasonography diagnosis for the invasive depth of early gastric cancer. Int J Gastrointest Cancer. 2006;37:133–8.
Lee HH, Lim CH, Park JM, Cho YK, Song KY, Jeon HM, et al. Low accuracy of endoscopic ultrasonography for detailed T staging in gastric cancer. World J Surg Oncol. 2012;10:190. doi:10.1186/1477-7819-10-190.
Park JS, Kim H, Bang B, Kwon K, Shin Y. Accuracy of endoscopic ultrasonography for diagnosing ulcerative early gastric cancers. Med (Baltimore). 2016;95:e3955.
Kaise M, Ohkura Y, Iizuka T, Kimura R, Nomura K, Kuribayashi Y, et al. Endocytoscopy is a promising modality with high diagnostic accuracy for gastric cancer. Endoscopy. 2015;47:19–25.
Bok GH, Jeon SR, Cho JY, Cho JH, Lee WC, Jin SY, et al. The accuracy of probe-based confocal endomicroscopy versus conventional endoscopic biopsies for the diagnosis of superficial gastric neoplasia (with videos). Gastrointest Endosc. 2013;77:899–908.
Li WB, Zuo XL, Li CQ, Zuo F, Gu XM, Yu T, et al. Diagnostic value of confocal laser endomicroscopy for gastric superficial cancerous lesions. Gut. 2011;60:299–306.
Kobayashi M, Neumann H, Hino S, Vieth M, Abe S, Nakai Y, et al. Influence of reviewers’ clinical backgrounds on interpretation of confocal laser endomicroscopy findings. Endoscopy. 2016;48:521–9.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
An erratum to this article is available at http://dx.doi.org/10.1007/s10120-017-0711-z.
Rights and permissions
About this article
Cite this article
Sumiyama, K. Past and current trends in endoscopic diagnosis for early stage gastric cancer in Japan. Gastric Cancer 20 (Suppl 1), 20–27 (2017). https://doi.org/10.1007/s10120-016-0659-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10120-016-0659-4