Abstract
Background
Clinical outcomes of early gastric cancer (EGC) patients after noncurative endoscopic submucosal dissection (ESD) have not been fully elucidated; we therefore aimed to clarify these outcomes.
Methods
A total of 3058 consecutive patients with 3474 clinically diagnosed EGCs at initial onset underwent ESD with curative intent at our hospital between 1999 and 2010. We retrospectively assessed the following clinical outcomes of noncurative gastric ESD patients with a possible risk of lymph node (LN) metastasis by dividing patients into two groups with different treatment strategies (additional gastrectomy and simple follow-up): presence of LN metastasis at the time of gastrectomy, incidence of LN and distant metastases during the follow-up period, clinicopathological factors associated with metastasis, and 5-year disease-specific survival (DSS).
Results
After exclusion of 75 noncurative ESD patients with only a positive horizontal margin, 569 noncurative ESD patients with a possible risk of LN metastasis were identified. Among the 356 patients undergoing additional gastrectomy, LN metastasis was identified in 18 patients. A positive vertical margin with submucosal invasion (odds ratio 3.6) and lymphovascular invasion (odds ratio 3.5) were significantly associated with LN metastasis. The 5-year DSS rate was 98.8 %. Among the 212 patients who underwent simple follow-up, LN and/or distant metastases were found in eight patients. In this group, lymphovascular invasion (hazard ratio 6.6) was significantly associated with metastasis with a 5-year DSS rate of 96.8 %.
Conclusions
Additional gastrectomy should be performed particularly in noncurative gastric ESD patients with lymphovascular invasion or a positive vertical margin with submucosal invasion.
Similar content being viewed by others
Introduction
Endoscopic submucosal dissection (ESD) is currently performed for early gastric cancer (EGC) with negligible risk of lymph node (LN) metastasis; the reported curative resection rates range from 73.6 to 94.7 % [1–14]. However, cases of noncurative resection still exist because the precise endoscopic prediction of EGC in terms of tumor depth, lateral spread, or lymphovascular invasion is difficult before treatment [5–14]. Although Japanese gastric cancer treatment guidelines describe nonsurgical management (close observation or immediate additional endoscopic treatment) instead of gastrectomy as an acceptable option for patients with differentiated-type adenocarcinoma in whom the only noncurative factor is a cancer-positive horizontal margin (HM), gastrectomy with LN dissection remains the standard treatment for cases of noncurative resection diagnosed with a possible risk of LN metastasis [4]. In general, noncurative ESD patients with a possible risk of LN metastasis are treated with additional gastrectomy; however, a relatively small number of these patients are selected to undergo simple follow-up without surgical treatment for various reasons [15]. Although several studies have reported clinical outcomes of noncurative gastric endoscopic resection (ER) patients, most of these reports have described clinical outcomes in a small number of patients without detailed assessments, with only two previous studies including more 200 noncurative gastric ER cases [15–25]. Therefore, we attempted to clarify the clinical outcomes of noncurative gastric ESD patients with a possible risk of LN metastasis by dividing the patients according to the following two treatment strategies on the basis of data from a large consecutive patient series: additional gastrectomy and simple follow-up.
Patients and methods
Patients
Patients with metachronous EGCs after ER, EGCs in the remnant stomach, and EGCs in the gastric tube were excluded from the present study. Following exclusion, 3058 consecutive patients [male-to-female ratio 3.5:1; median age 68 years (range 27–94 years)] with 3474 clinically diagnosed EGC lesions at initial onset in the normal stomach (579 in the upper third, 1442 in the middle third. and 1453 in the lower third) underwent ESD with curative intent at our hospital between 1999 and 2010.
The risks and benefits of the ESD procedure were thoroughly explained to each patient, and written informed consent was obtained before ESD.
ESD procedure
The ESD procedure was initiated with the identification of the lesion and the marking of dots at a distance of about 5 mm outside the lesion border. After submucosal injection of saline solution or sodium hyaluronate (MucoUp®; Johnson & Johnson, Tokyo, Japan) with epinephrine, a 1- to 2-mm precut incision was made with an electrosurgical needle knife (KD-1L-1; Olympus, Tokyo, Japan) or a DualKnife (KD-650Q; Olympus), followed by a circumferential mucosal incision outside the marking dots with an insulation-tipped (IT) diathermy knife (KD-610L; Olympus) or an ITknife2 (KD-611L; Olympus). The submucosal layer was then dissected with an ITknife or an ITknife2 after an additional submucosal injection.
After the lesion had been resected, histopathological examination was performed in accordance with the recommendations of the Japanese classification of gastric carcinoma [26]. The endoscopically resected specimens were sectioned at 2-mm intervals, and all specimens were reviewed by at least two board-certified expert gastrointestinal pathologists. Histological type was defined according to the major histological features of the resected lesions. According to the Japanese classification of gastric carcinoma and Japanese gastric cancer treatment guidelines, differentiated-type adenocarcinoma included tubular adenocarcinoma and papillary adenocarcinoma, whereas undifferentiated-type adenocarcinoma included poorly differentiated adenocarcinoma, signet ring cell carcinoma, and mucinous adenocarcinoma [4, 26]. Tumoral infiltration of the submucosa was subclassified as SM1 (less than 500 μm from the muscularis mucosae) or SM2 (500 μm or more from the muscularis mucosae) [4, 26]. The presence of ulcerative findings, including ulcer and ulcer scar, was histologically determined. Lymphovascular invasion was first determined with hematoxylin and eosin stained sections; when the diagnosis of lymphovascular invasion was inconclusive with hematoxylin and eosin stained sections, immunohistochemistry using the monoclonal antibody D2-40 and/or Victoria blue or Elastica van Gieson staining was additionally performed.
Pathological curability
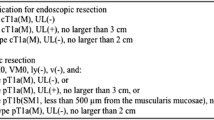
According to the Japanese gastric cancer treatment guidelines from 2010 (version 3), the following was curative ESD for the absolute indications: en bloc resection, tumor size 2 cm or less, differentiated-type histological appearance, pT1a, negative HM (HM 0), negative vertical margin (VM 0), no lymphatic invasion, and no venous invasion [4]. In addition, the resection was considered as curative ESD for the expanded indications when all of the following conditions were fulfilled: en bloc resection, HM 0, VM 0, no lymphatic invasion, and no venous invasion, with (1) tumor size greater than 2 cm, differentiated-type cancer, pT1a (M), no ulcerative findings; (2) tumor size 3 cm or smaller, differentiated-type cancer, pT1a, ulcerative findings; (3) tumor size 2 cm or smaller, undifferentiated-type cancer, pT1a, no ulcerative findings; (4) tumor size 3 cm or smaller, differentiated-type cancer, pT1b (SM1). Resection that did not satisfy any of the above criteria was considered as noncurative ESD. In the present study, the patients were divided into two groups on the basis of the above-mentioned confirmation of pathological curability: (1) curative ESD for absolute indications or for expanded indications, and (2) noncurative ESD. For patients with multiple EGCs, the curability was considered as noncurative ESD when the criteria for noncurative ESD were fulfilled for at least one lesion.
Follow-up care after ESD
According to the Japanese gastric cancer treatment guidelines, noncurative ESD patients with a possible risk of LN metastasis were generally referred for additional gastrectomy with LN dissection [4]. If patients with noncurative resections were not selected to undergo surgical resection for various reasons, these patients generally underwent endoscopic surveillance with abdominal computed tomography, abdominal ultrasonography, or endoscopic ultrasonography every 6–12 months for at least 3 years, with annual follow-up thereafter. In addition, abdominal computed tomography or abdominal ultrasonography was performed every 12 months in noncurative ESD patients undergoing an additional gastrectomy.
Assessment of the clinical outcomes of noncurative ESD
By dividing patients into two groups with different treatment strategies (additional gastrectomy and simple follow-up), we assessed the following clinical outcomes of noncurative gastric ESD patients with a possible risk of LN metastasis: clinicopathological findings, including age, sex, and Charlson comorbidity index, for the two treatment strategies, the reasons for simple follow-up, the presence of LN metastasis at the time of additional gastrectomy, and the incidence of LN and distant metastases in patients selected to undergo simple follow-up [27]. We further analyzed the following clinicopathological factors associated with metastasis for each treatment strategy using multivariate analyses: age (younger than 70 years vs 70 years or older), sex (male vs female), location (upper/middle vs lower), macroscopic type (flat/depressed vs elevated), tumor size (less than 30 mm vs 30 mm or more), depth of invasion (mucosa/SM1 vs SM2), presence/absence of ulcerative findings, major histological type (differentiated type vs undifferentiated type), presence/absence of positive HM, presence/absence of positive VM with submuscosal invasion, and presence/absence of lymphovascular invasion. Finally, we assessed the long-term survival outcomes, including 5-year overall survival (OS) and disease-specific survival (DSS), for the two treatment strategies. We further analyzed the clinicopathological factors associated with gastric-cancer-related death in noncurative gastric ESD patients using multivariate analyses.
Clinical outcome data, including long-term survival outcome data, were collected retrospectively from medical records from October 2014 to December 2014. For patients who had not visited our hospital regularly, data were retrieved by our requesting the data from the referring physicians, contacting the patient’s homes, or checking the statistical data maintained by the local government registry.
Statistical analysis
The Fisher exact test or the χ 2 test was used for the univariate analyses to assess the clinicopathological factors associated with LN metastasis at the time of additional gastrectomy. We performed a multivariate logistic regression analysis for factors that were significant in univariate analyses to identify independent risk factors for LN metastasis. In addition, we performed univariate analysis using the log-rank test to evaluate the clinicopathological factors associated with LN and distant metastases in patients selected to undergo simple follow-up and the clinicopathological factors associated with gastric-cancer-related death in noncurative gastric ESD patients. We then performed multivariate analysis using the Cox proportional hazards model for variables considered significant on univariate analysis.
Survival time was calculated as the interval between the date of the first treatment and the date of death or the last date on which patients were confirmed to be alive. Survival curves were drawn in accordance with the Kaplan–Meier method. Patients with successful follow-up were defined as those for whom information regarding whether they were alive over a 3-year period after the ESD or dead could be obtained. All the statistical analyses were performed with the statistical analysis software program SPSS, version 20 (SPSS Japan, Tokyo, Japan). P < 0.05 was considered statistically significant.
Results
By patient-based analysis, 644 noncurative ESD patients were found (21 % of the 3058 EGC patients). After exclusion of 75 noncurative ESD patients with only a positive HM, 569 noncurative ESD patients with a possible risk of LN metastasis were identified and divided into two groups with different treatment strategies: additional gastrectomy (356 patients) and simple follow-up (212 patients); only one patient underwent additional ESD (Fig. 1).
The clinicopathological findings for the two treatment strategies for noncurative gastric ESD patients are shown in Table 1 [9, 15, 27]. A higher proportion of SM2 invasion (n = 217, 61 %), lymphovascular invasion (n = 142, 40 %), and a positive VM with submuscosal invasion (n = 54, 15 %) was observed in the 356 patients who underwent additional gastrectomy, whereas a higher proportion of advanced age (age 70 years or older, n = 124, 58 %), comorbidity (Charlson comorbidity index 2 or greater, n = 43, 20 %), SM1 invasion with a noncurative factor (SM1 more than 3 cm or undifferentiated-type component with SM1 invasion, n = 35, 17 %), positive VM in mucosal cancer (n = 31, 15 %), and mucosal cancer with ulcerative findings and tumor size of more than 3 cm (n = 26, 12 %) was observed in the 212 patients who underwent simple follow-up (Table 1).
The following reasons were observed for patient selected to undergo simple follow-up (n = 212): (1) patient refusing to undergo surgery (n = 47, 22 %); (2) poor prognosis and/or high surgical risk (considered inoperable because of poor physical condition) because of advanced age (n = 46, 22 %), concomitant disease (n = 41, 19 %), comprising concomitant cancer in other organs (n = 27), and severe comorbidities (n = 14); (3) unknown (n = 7); and (4) the presence of noncurative factors that are regarded as indicative of a relatively low risk of LN metastasis by individual physicians (n = 71, 33 %). These noncurative factors include a positive VM in mucosal cancer (n = 23), mucosal cancer with ulcerative findings and tumor size of more than 3 cm (n = 17), SM1 cancer with tumor size of more than 3 cm (n = 14), undifferentiated-type cancer with tumor size of more than 2 cm (n = 5), undifferentiated-type cancer with ulcerative findings (n = 4), positive HM in undifferentiated-type cancer (n = 4), positive VM in SM1 cancer (n = 2), and SM2 invasion (n = 2 each; 550 and 800 μm, respectively).
LN metastasis was identified in 18 (5.3 %) of the 338 patients undergoing additional gastrectomy in whom detailed data concerning surgical resection could be obtained (except the 18 patients whose data regarding surgical resection at other hospitals could not be obtained). Regarding clinicopathological factors associated with LN metastasis, a positive VM with submuscosal invasion and lymphovascular invasion was found to be significantly associated with LN metastasis at the time of gastrectomy on the basis of univariate analyses (Table 2). By multivariate analysis for variables considered significant on univariate analysis with a marginally significant variable (depth of invasion), a positive VM with submuscosal invasion [odds ratio (OR) 3.6; 95 % confidence interval (CI) 1.3–10.2; P = 0.017] and lymphovascular invasion (OR 3.5; 95 % CI 1.2–10.4; P = 0.022) were significantly associated with LN metastasis (Table 2).
Among the 192 patients who were selected to undergo simple follow-up with successful follow-up, LN and/or distant metastases was identified in eight patients (4.2 %) for a median duration of 70.0 months (range 1–181 months). Regarding clinicopathological factors associated with LN and/or distant metastases, lymphovascular invasion, a positive VM with submuscosal invasion, and SM2 invasion were found to be significantly associated with metastasis during the follow-up period by univariate analyses (Table 3). On the basis of multivariate analysis for variables considered significant on univariate analysis with a marginally significant variable (ulcerative findings), lymphovascular invasion (hazard ratio 6.6; 95 % CI 1.4–32.0; P = 0.018) was found to be significantly associated with metastasis (Table 3).
Analysis of the long-term survival outcomes indicated that successful follow-up was achieved in 95 % (n = 540) of the 568 noncurative ESD patients with a possible risk of LN metastasis. Specifically, 469 patients were confirmed as alive for at least 3 years after the ESD, whereas 71 patients died of various causes (including 13 patients who died of gastric cancer); the remaining 28 patients were lost to follow-up. The median follow-up period was 74 months (range 1–181 months). Among 348 noncurative ESD patients undergoing additional gastrectomy who were successfully followed up for a median duration of 76 months (range 3–154 months), six patients died of gastric cancer, despite gastrectomy. Of these six patients, only one patient was found to have LN metastasis at the time of additional gastrectomy. The 5-year OS and DSS rates in the 348 patients who underwent additional gastrectomy with successful follow-up were 94.7 and 98.8 % respectively (Figs. 2, 3). Conversely, among 192 patients who were selected to undergo simple follow-up with successful follow-up, seven died of gastric cancer. The 5-year OS and DSS rates among these 192 patients were 83.8 and 96.8 % respectively (Figs. 2, 3).
Assessment of the clinicopathological factors associated with gastric-cancer-related death in noncurative gastric ESD patients revealed that SM2 invasion, a positive VM with submuscosal invasion, and lymphovascular invasion were significantly associated with gastric-cancer-related death on the basis of univariate analyses (Table 4). By multivariate analysis for variables considered significant on univariate analysis with clinically important variables (age, sex, and treatment) and a marginally significant variable (ulcerative findings), lymphovascular invasion (OR 6.7; 95 % CI 1.8–25.7; P = 0.005) and simple follow-up (OR 5.7; 95 % CI 1.8–18.2; P = 0.004) were found to be significantly associated with gastric-cancer-related death (Table 4).
Discussion
Therapeutic outcomes of gastric ESD are currently excellent; however, a small number of cases of noncurative resection still occur because of the challenging nature of precise endoscopic diagnosis of EGC before ESD [1–14]. Although several studies have described the clinical outcomes of noncurative gastric ER patients, the definition of noncurative gastric ER differs between studies; most of these studies have assessed the clinical outcomes of noncurative gastric ER patients in small numbers of patients without detailed statistical analysis [15–25]. For example, noncurative gastric ER was defined according to the Japanese gastric cancer treatment guidelines in some studies but was defined according to the original criteria in others [4, 15–25]. In addition, with the exception of two studies by Oda et al. [15] and Yang et al. [16], fewer than 200 noncurative gastric ER cases were included in previous studies [15–25]. To the best of our knowledge, the present study is the largest study demonstrating the clinical outcomes of more 500 noncurative gastric ESD patients, including long-term survival outcomes with a median follow-up period of more than 5 years and clinicopathological factors associated with metastasis and gastric-cancer-related death. The definitions of noncurative gastric ER in the present study were based on the Japanese gastric cancer treatment guidelines [4].
In terms of long-term outcomes of noncurative gastric ER patients, a study by Oda et al. [15] from our institution enrolled a large number of patients and evaluated the long-term survival outcomes of noncurative gastric ER patients with a possible risk of LN metastasis (n = 226) by dividing the patients into noncurative gastric ER patients undergoing additional gastrectomy (n = 144) and patients selected to undergo simple follow-up only (n = 82). Among the 144 patients who underwent additional gastrectomy, LN metastasis was identified in 6.3 % of patients, with a 5-year DSS rate of 97.8 % for a median follow-up period of 4 years. In contrast, distant metastasis was identified in 2.4 % of the 82 patients selected to undergo simple follow-up alone, with a 5-year DSS rate of 91 % for a median follow-up period of 3.2 years. Although their study thoroughly evaluated the long-term survival outcomes, it included noncurative gastric endoscopic mucosal resection patients in addition to noncurative gastric ESD patients with a median follow-up period of less than 5 years. Choi et al. [20] reported the long-term survival outcomes of noncurative gastric ESD patients with submuscosa-invasive gastric cancer (n = 89). This study demonstrated that OS and disease-free survival did not differ significantly between patients treated with additional surgical resection and patients undergoing simple follow-up after ESD. More recently, Yamanouchi et al. [21] reported that the DSS rate did not differ significantly between observation and additional surgery groups after noncurative ESD, although there were only 79 noncurative gastric ESD patients in their report. In addition, Hoteya et al. [22] described that gastric-cancer-related deaths and OS rates did not differ significantly between observation and additional surgery groups; however the number of noncurative gastric ESD patients included in this study was also less than 200 (165 patients). The remaining studies have predominantly focused on tumor recurrence after noncurative ER without detailed analysis of survival outcomes [23–25]. Accordingly, the long-term survival outcomes of noncurative gastric ER patients have not been fully elucidated. We therefore conducted the present study to clarify the long-term survival outcomes of noncurative gastric ESD patients on the basis of our extensive clinical experience. In the present study, OS of the noncurative ESD patients who underwent simple follow-up was lower than that of the patients who underwent additional gastrectomy. Among the patients who underwent simple follow-up, advanced age or concomitant disease may have contributed to the poor prognosis of several patients in this group as the OS of the noncurative ESD patients who underwent simple follow-up was lower. Therefore, simple follow-up may be an acceptable management option instead of additional gastrectomy in noncurative ESD patients with lower survival rates, such as elderly patients and/or patients with severe concomitant disease. On the other hand, additional gastrectomy with lymphadenectomy may be more appropriate than simple follow-up in noncurative ESD patients without concomitant disease and who are young enough to undergo recommended surgical interventions according to the Japanese gastric cancer treatment guidelines because of the favorable outcomes of surgical treatment [4, 28–30]. Thus, it is necessary to assess the clinicopathological factors associated with LN and/or distant metastases and gastric-cancer-related death to identify noncurative ESD patients for whom additional gastrectomy should be particularly performed and to establish the evidence for decision making on additional gastrectomy in noncurative ESD patients.
Accordingly, we assessed the clinicopathological factors associated with LN and/or distant metastases and gastric-cancer-related death. The results of the present study showed that a positive VM with submuscosal invasion and lymphovascular invasion were independent risk factors for LN metastasis in noncurative gastric ESD patients undergoing additional gastrectomy. In addition, lymphovascular invasion was identified as an independent predictor of LN and distant metastases in patients undergoing simple follow-up. Further, lymphovascular invasion and simple follow-up were identified as an independent predictors of gastric-cancer-related death in noncurative gastric ESD patients. Thus, we concluded that additional gastrectomy should be particularly performed for noncurative gastric ESD patients with lymphovascular invasion or a positive VM with submuscosal invasion who were suspected of being at high risk of metastasis. In addition, we suggest that additional gastrectomy should be considered specifically for noncurative gastric ESD patients with lymphovascular invasion to avoid gastric-cancer-related death. Regarding the clinicopathological factors associated with LN and/or distant metastases in noncurative gastric ER patients, Yang et al. [16] reported venous invasion, SM2 invasion, or antral tumor location as an independent predictor for LN metastasis on the basis of the evaluation of 267 patients who underwent noncurative ER for EGC. They also reported LN metastasis rates of 1.1 % (95 % CI 0–2.7) in patients with one or no predictor and 17.8 % (95 % CI 9.7–25.8) in those with two or more predictors. In addition, Ishii et al. [17] reported that both SM2 and moderate/marked lymphatic invasion are significant predictors for LN metastasis that may be important as references for additional gastrectomy after ER on the basis of the assessment of 112 patients with clinical T1aN0 tumors who underwent additional gastrectomy after noncurative ER. Except for these two reports and the present study, no other studies with detailed assessment of the clinicopathological factors associated with metastasis and gastric-cancer-related death have been performed in a large number noncurative ER patients. Further, the definitions of noncurative ER patients in the remaining reports were not based on the Japanese gastric cancer treatment guidelines [18, 19]. Most recently, Sekiguchi et al. [31] from our institution revealed detailed LN metastasis risk stratification data in EGCs and developed an 11-point scoring model with possible usefulness for the prediction of LN metastasis by using surgically resected EGC patients instead of endoscopically resected EGC patients. Therefore, the present study is particularly important as it provides sufficient evidence to identify predictors of metastasis and gastric-cancer-related death after noncurative ESD in a large number of noncurative ESD patients.
The results of the present study showed that lymphovascular invasion was an independent predictor of metastasis and gastric-cancer-related death in noncurative gastric ESD patients. Regarding the risk of LN metastasis in mucosal cancer with lymphovascular invasion, there was one patient (5.6 %) with LN metastasis among a total of 18 patients with mucosal cancer with lymphovascular invasion in this study (detailed data not shown). In addition, Sekiguchi et al. [31] reported the risk of LN metastasis in mucosal cancer with lymphovascular invasion to be 29.2 % (7/24) among 3131 surgically resected EGC patients; thus, the risk of LN metastasis is higher even in patients with mucosal cancer with lymphovascular invasion. Further, regarding histological examinations of lymphovascular invasion, Sako et al. [32] reported that the detection of lymphovascular invasion of undifferentiated-type cancer was difficult even with immunohistochemical staining. Therefore, despite extensive histopathological evaluation, including immunohistochemical staining, practical limitations in determining lymphovascular invasion, particularly for undifferentiated-type cancer, may exist, and we need to recognize the distinct possibility of such limitations.
The present study demonstrated the clinical outcomes of noncurative gastric ESD patients in a large number of patients with a median follow-up period of more than 5 years. However, the present study had several limitations. First, the results were obtained from a retrospective assessment based on the medical records of patients undergoing gastric ESD at a single major referral cancer center in Japan. Thus, a prospective multicenter nationwide study over a period of 5 years is required to evaluate the clinical outcomes of noncurative gastric ESD patients more precisely. Several multicenter prospective studies are being conducted [33–35]. Second, we did not directly identify EGC patients at relatively low risk of metastasis who could be followed up without additional surgery; instead we focused on noncurative EGC patients at high risk of metastasis and gastric-cancer-related death. Therefore, the results of our study, particularly our findings related to EGC patients at relatively low risk of metastasis, should be interpreted with caution because of this limitation. A study that focuses on the identification of EGC patients at relatively low risk of metastasis based on detailed data with risk stratification for LN and/or distant metastases after noncurative gastric ESD will be necessary to identify such patients who can be followed up without additional surgery [31]. In addition, the expected survival and surgical risk in individual patients who undergo noncurative gastric ESD could not be fully evaluated in the present study as it was difficult to obtain detailed information regarding stratification of the expected survival and surgical risk in individual patients in this retrospective study. Therefore, a prospective study including objective evaluation of the expected survival rate and surgical risk in individual patients is required to establish more appropriate treatment strategies and to develop more individualized treatment plans for patients undergoing noncurative ESD.
In conclusion, additional gastrectomy should be particularly performed in noncurative gastric ESD patients with high risk of metastasis such as those with lymphovascular invasion or a positive VM with submuscosal invasion.
References
Gotoda T, Yanagisawa A, Sasako M, Ono H, Nakanishi Y, Shimoda T, et al. Incidence of lymph node metastasis from early gastric cancer: estimation with a large number of cases at two large centers. Gastric Cancer. 2000;3:219–25.
Ono H, Kondo H, Gotoda T, Shirao K, Yamaguchi H, Saito D, et al. Endoscopic mucosal resection for treatment of early gastric cancer. Gut. 2001;48:225–9.
Hirasawa T, Gotoda T, Miyata S, Kato Y, Shimoda T, Taniguchi H, et al. Incidence of lymph node metastasis and the feasibility of endoscopic resection for undifferentiated-type early gastric cancer. Gastric Cancer. 2009;12:148–52.
Japanese Gastric Cancer Association. Japanese gastric cancer treatment guidelines 2010 (ver. 3). Gastric Cancer. 2011;14:113–23.
Oda I, Gotoda T, Hamanaka H, Eguchi T, Saito Y, Matsuda T, et al. Endoscopic submucosal dissection for early gastric cancer: technical feasibility, operation time and complications from a large consecutive series. Dig Endosc. 2005;17:54–8.
Oda I, Saito D, Tada M, Iishi H, Tanabe S, Oyama T, et al. A multicenter retrospective study of endoscopicresection for early gastric cancer. Gastric Cancer. 2006;9:262–70.
Isomoto H, Shikuwa S, Yamaguchi N, Fukuda E, Ikeda K, Nishiyama H, et al. Endoscopic submucosal dissection for early gastric cancer: a large-scale feasibility study. Gut. 2009;58:331–6.
Hoteya S, Iizuka T, Kikuchi D, Yahagi N. Benefits of endoscopic submucosal dissection according to size and location of gastric neoplasm, compared with conventional mucosal resection. J Gastroenterol Hepatol. 2009;24:1102–6.
Nonaka S, Oda S, Nakaya T, Kusano C, Suzuki H, Yoshinaga S, et al. Clinical impact of a strategy involving endoscopic submucosal dissection for early gastric cancer: determining the optimal pathway. Gastric Cancer. 2011;14:56–62.
Toyonaga T, Man-I M, East JE, Nishino E, Ono W, Hirooka T, et al. 1,635 endoscopic submucosal dissection cases in the esophagus, stomach, and colorectum: complication rates and long-term outcomes. Surg Endosc. 2013;27:1000–8.
Oda I, Oyama T, Abe S, Ohnita K, Kosaka T, Hirasawa K, et al. Preliminary results of multicenter questionnaire study on long-term outcomes of curative endoscopic submucosal dissection for early gastric cancer. Dig Endosc. 2014;26:214–9.
Kosaka T, Endo M, Toya Y, Abiko Y, Kudara N, Inomata M, et al. Long-term outcomes of endoscopic submucosal dissection for early gastric cancer: a single-center retrospective study. Dig Endosc. 2014;26:183–91.
Ohnita K, Isomoto H, Shikuwa S, Yajima H, Minami H, Matsushima K, et al. Early and long-term outcomes of endoscopic submucosal dissection for early gastric cancer in a large patient series. Exp Ther Med. 2014;7:594–8.
Suzuki H, Oda I, Abe S, Sekiguchi M, Mori G, Nonaka S, et al. High rate of 5-year survival among patients with early gastric cancer undergoing curative endoscopic submucosal dissection. Gastric Cancer. 2016;19:198–205.
Oda I, Gotoda T, Sasako M, Sano T, Katai H, Fukagawa T, et al. Treatment strategy after non-curative endoscopic resection of early gastric cancer. Br J Surg. 2008;95:1495–500.
Yang HJ, Kim SG, Lim JH, Choi J, Im JP, Kim JS, et al. Predictors of lymph node metastasis in patients with non-curative endoscopic resection of early gastric cancer. Surg Endosc. 2015;29:1145–55.
Ishii S, Yamashita K, Kato H, Nishizawa N, Ushiku H, Mieno H, et al. Predictive factors for lymph node metastasis in additional gastrectomy after endoscopic resection of cT1aN0 gastric cancer. Surg Today. 2015. doi:10.1007/s00595-015-1281-5.
Ryu KW, Choi IJ, Doh YW, Kook MC, Kim CG, Park HJ, et al. Surgical indication for non-curative endoscopic resection in early gastric cancer. Ann Surg Oncol. 2007;14:3428–34.
Son SY, Park JY, Ryu KW, Eom BW, Yoon HM, Cho SJ, et al. The risk factors for lymph node metastasis in early gastric cancer patients who underwent endoscopic resection: is the minimal lymph node dissection applicable? A retrospective study. Surg Endosc. 2013;27:3247–53.
Choi JY, Jeon SW, Cho KB, Park KS, Kim ES, Park CK, et al. Non-curative endoscopic resection does not always lead to grave outcomes in submucosal invasive early gastric cancer. Surg Endosc. 2015;29:1842–9.
Yamanouchi K,Ogata S, Sakata Y, Tsuruoka N, Shimoda R, Nakayama A, et al. Effect of additional surgery after noncurative endoscopic submucosal dissection for early gastric cancer. Endosc Int Open. 2016;4(1):E24–9.
Hoteya S, Iizuka T, Kikuchi D, Ogawa O, Mitani T, Matsui A, et al. Clinicopathological outcomes of patients with early gastric cancer after non-curative endoscopic submucosal dissection. Digestion. 2016;93:53–8.
Noh GY, Ku HR, Kim YJ, Park SC, Kim J, Han CJ, et al. Clinical outcomes of early gastric cancer with lymphovascular invasion or positive vertical resection margin after endoscopic submucosal dissection. Surg Endosc. 2015;29:2583–9.
Han JP, Hong SJ, Kim HK, Lee YN, Lee TH, Ko BM, et al. Risk stratification and management of non-curative resection after endoscopic submucosal dissection for early gastric cancer. Surg Endosc. 2016;30:184–9.
Kang MS, Hong SJ, Kim DY, Han JP, Choi MH, Kim HK, et al. Long-term outcome after endoscopic submucosal dissection for early gastric cancer: focusing on a group beyond the expanded indication. J Dig Dis. 2015;16:7–13.
Japanese Gastric Cancer Association. Japanese classification of gastric carcinoma: 3rd English edition. Gastric Cancer. 2011;14:101–12.
Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40:373–83.
Sasako M, Kinoshita T, Maruyama K. Prognosis of early gastric cancer. Stomach Intest. 1993;28:139–46 (abstract in English).
Gotoda T, Sasako M, Ono H, Katai H, Sano T, Shimoda T. Evaluation of the necessity for gastrectomy with lymph node dissection for patients with submucosal invasive gastric cancer. Br J Surg. 2001;88:444–9.
Okamura T, Tsujitani S, Korenaga D, Haraguchi M, Baba H, Hiramoto Y, et al. Lymphadenectomy for cure in patients with early gastric cancer and lymph node metastasis. Am J Surg. 1988;155:476–80.
Sekiguchi M, Oda I, Taniguchi H, Suzuki H, Morita S, Fukagawa T, et al. Risk stratification and predictive risk-scoring model for lymph node metastasis in early gastric cancer. J Gastroenterol 2016;51:961–70.
Sako A, Kitayama J, Ishikawa M, Yamashita H, Nagawa H. Impact of immunohistochemically identified lymphatic invasion on nodal metastasis in early gastric cancer. Gastric Cancer. 2006;9:295–302.
Oda I, Shimazu T, Ono H, Tanabe S, Iishi H, Kondo H, et al. Design of Japanese multicenter prospective cohort study of endoscopic resection for early gastric cancer using Web registry (J-WEB/EGC). Gastric Cancer. 2012;15:451–4.
Kurokawa Y, Hasuike N, Ono H, Boku N, Fukuda H. A phase II trial of endoscopic submucosal dissection for mucosal gastric cancer: Japan Clinical Oncology Group study JCOG0607. Jpn J Clin Oncol. 2009;39:464–6.
Takizawa K, Takashima A, Kimura A, Mizusawa J, Hasuike N, Ono H, et al. A phase II clinical trial of endoscopic submucosal dissection for early gastric cancer of undifferentiated type: Japan Clinical Oncology Group study JCOG1009/1010. Jpn J ClinOncol. 2013;43:87–91.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Human rights statement and informed consent
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1964 and later versions. Informed consent or substitute for it was obtained from all patients for their being included in the study.
Animal studies
This article does not contain any studies with human or animal subjects performed by any of the authors.
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Suzuki, H., Oda, I., Abe, S. et al. Clinical outcomes of early gastric cancer patients after noncurative endoscopic submucosal dissection in a large consecutive patient series. Gastric Cancer 20, 679–689 (2017). https://doi.org/10.1007/s10120-016-0651-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10120-016-0651-z