Abstract
Background
The usefulness of magnifying endoscopy with narrow-band imaging (ME-NBI) for undifferentiated-type early gastric cancers (UD-type EGCs) is unclear. The present study examined the accuracy of the diagnostic demarcation of lesions using ME-NBI.
Methods
The study population consisted of 76 patients with UD-type EGC lesions measuring ≤20 mm in diameter using white-light imaging (WLI) and endoscopic ultrasonography and diagnosed as intramucosa and UL(−); all the lesions were confirmed as early gastric cancer based on postoperative pathological examination. All the patients had undergone an initial endoscopic submucosal dissection (ESD) at this hospital between January 2010 and January 2014. After marking with demarcation lines at the utmost oral and anal sites of the lesion using argon plasma coagulation under ME-NBI for intervention, the cases with demarcations that were consistent with the postoperative pathological findings were defined as having been accurately diagnosed. The inflammatory cell infiltration (Updated Sydney System, USS) were also assessed.
Results
The diagnostic demarcations of the lesion were consistent in 62 cases (81.6 %). The accurate diagnosis rate was higher for the USS cases with mild neutrophil and monocyte infiltration (P < 0.05). The addition of ME-NBI to WLI improved the accurate diagnosis rate by 27.6 %.
Conclusion
The use of ME-NBI in diagnostic demarcation of UD-type EGCs is recommended.
Similar content being viewed by others
Introduction
With the extension of indications for endoscopic submucosal dissection (ESD) for undifferentiated-type early gastric cancers (UD-type EGCs) [1–3], an improvement in preoperative diagnostic performance is currently being sought. According to the reports of Gotoda et al. [2] and Hirasawa et al. [3], UD-type EGC is classified under the extended indications for ESD in the Japanese Gastric Cancer Association Guideline [1] insofar as it is an intramucosal carcinoma measuring ≤20 mm in diameter, ulcer scar free, and without invasion into the lymphatic and blood vessels, thereby having a negligible risk of lymph node metastasis. The usefulness of magnifying endoscopy with narrow-band imaging (ME-NBI) in delineating the demarcation of differentiated-type early gastric cancer has been reported [4–6], whereas in UD-type EGCs, the diagnostic delineation of lesion demarcation is difficult because of the presence of proliferative zone extension [7], and the usefulness of ME-NBI is thus unclear for these lesions. There have been reports on ME-NBI findings for UD-type EGCs, and Nakayoshi et al. [8] reported that corkscrew patterns were demonstrated in approximately 90 % of cases. Okada and colleagues investigated the by-growth pattern ME-NBI features of undifferentiated-type carcinomas and documented their post-ESD histopathological findings, indicating a significant expansion of intervening parts (inter-crypt regions) in neoplastic lesions, compared with noncancerous regions [9]. However, whether such expansion of intervening parts might be useful for the diagnostic demarcation of lesions has not been sufficiently explored, and the extent to which ME-NBI might yield an additional effect, compared with routine observation using white-light imaging (WLI), in terms of the diagnostic demarcation of lesions, remains uncertain. This study was conducted to clarify the accuracy of the diagnostic demarcation of lesions using ME-NBI in UD-type EGCs and to assess its additional effect.
Patients and methods
This study is a prospective interventional study. The intervention is marking with demarcation lines at the utmost oral and utmost anal sites of the lesion by argon plasma coagulation (APC) under ME-NBI.
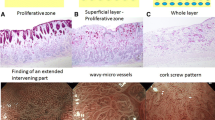
Seventy-six cancer lesions measuring ≤20 mm in diameter and diagnosed as M and UL(−) during routine observation (WLI) and endoscopic ultrasound (EUS) examination, and that were proven to be early cancers upon postoperative pathological examination were selected from among cases of UD-type EGCs which underwent an endoscopic resection for the first time at this hospital between January 2010 and January 2014, were included in this study. Preoperative endoscopic images and histopathological slides were reviewable for all the lesions. The present observations were performed by three specialists certified by the Japan Gastroenterological Endoscopy Society, each with more than 10 years of experience performing endoscopies. Recognition of the target lesion demarcation was performed using magnifying endoscopy (GIF-H260Z; Olympus, Tokyo, Japan) with WLI, followed by photographic recording. The lesion was then diagnostically demarcated using ME-NBI based on findings such as a widening of intervening parts (Fig. 1) and weave-like microvessels and corkscrew patterns [8, 9] (Fig. 2), with subsequent marking with demarcation lines (DL) at the utmost oral and utmost anal sites of the lesion by APC (Fig. 3). The inter-crypt distance was measured from the center of one crypt to the center of an adjacent crypt. Through collation with postoperative pathological data, the rate of accurate diagnosis was calculated by defining accurate diagnosis as the consistency of the utmost oral and anal demarcation lines of the lesion with those found in the pathological examination (Fig. 4). Cases with consistency of either the utmost rostral or the utmost anal demarcation line alone were regarded as inconsistent cases. Each resected tissue specimen was sectioned at 2-mm intervals, so that the acceptable error for accurate diagnosis was set at ≤1 mm. Our pre-ESD exploratory protocol is composed of the evaluation of the lesion and biopsies from the peri-lesional area using WLI, chromoendoscopy, and ME-NBI to delineate the required extent of the ESD. Endoscopic ultrasound examination was added to this protocol in cases in which the depth of tumor invasion was a concern. On the day of ESD, the extent of the lesion was precisely diagnosed and determined using ME-NBI, and APC marking was then performed along the demarcation line. The primary aim of this approach was to ascertain to what extent the lesion could be accurately diagnosed using ME-NBI, and the pre-ESD examinations did not have any direct impact upon the diagnostic delineation of the lesion at the time of ESD. The proliferative zone extension distance, inter-crypt (intervening part) distance, and inflammatory cell infiltration in individual cases were also assessed. The proliferative zone extension distance is the mean distance. The proliferative zone extension distance and the inter-crypt distance were measured using light microscopy at a magnification of 100×. For the proliferative zone extension distance, the extent of the APC-marked region was measured. Regarding the inter-crypt distance, the distances of the intervening part in a cancerous region and that in a noncancerous region were measured at five to ten sites, respectively, and their means were then calculated to determine the cancerous to noncancerous region ratio. Inflammatory cell infiltration was assessed in the following four categories: mononuclear cells infiltration, neutrophils infiltration, atrophy, and intestinal epithelial metaplasia, according to the classification in the Updated Sydney System (USS) [10]. The lesions were graded for each category into two groups, i.e., a normal/mild group and a moderate/marked group, and the accurate diagnosis rate was calculated for each group. Regarding the additional effect of ME-NBI to WLI, WLI endoscopic photographs were reviewed to delineate diagnostically the utmost oral and the utmost anal demarcations, whereby the accurate diagnosis rate was calculated. A correct WLI diagnosis was defined as a WLI-diagnosed extent that coincided with the extent determined on pathological tissue slides, as was the case with ME-NBI. This criterion means that none of the cases had a correct WLI diagnosis but a false ME-NBI diagnosis; hence, a correct WLI diagnosis coincided with a correct ME-NBI diagnosis. Accordingly, the diagnosis can be considered correct if the WLI-diagnosed extent coincides with the ME-NBI-based APC marking positions. Therefore, we determined whether a correct diagnosis had been made by determining the WLI-diagnosed extent and then collating these results with the ME-NBI-based APC marking positions. The person who evaluated the WLI images was unaware of the results of the pathological examinations and diagnosed the lesion extent based solely on the still images.
Undifferentiated-type early gastric cancer invasion collated with magnifying endoscopy (ME)–narrow-band imaging (NBI) findings. a A carcinoma confined to the proliferative zone is shown to have an expanded intervening part using ME-NBI. b A carcinoma extending from the superficial layer into the proliferative zone is visualized as exhibiting weave-like microvessels using ME-NBI. c A carcinoma involving the whole layer of the mucosa is visualized as having a corkscrew pattern using ME-NBI
Actual argon plasma coagulation (APC) markings. The dotted line indicates a tumor border region as viewed under white-light imaging (WLI). The arrow points to a tumor border region as viewed using magnifying endoscopy with NBI (ME-NBI). a Tumor border at the utmost rostral site under WL. b Demarcation line as viewed using ME-NBI (coinciding with a). c A higher-magnification view of b. d An APC marking placed on the demarcation line. e Tumor border at the utmost anal site under WL. f Demarcation line as viewed using ME-NBI (inconsistent with e). g A higher-magnification view of f. h An APC marking placed on the demarcation line
Postendoscopic submucosal dissection (ESD) histopathological specimen from patient in Fig. 3. The APC marking coincided with the cancerous–noncancerous border on the histopathological slide
Furthermore, the accurate diagnosis rate using ME-NBI was also calculated and was regarded as an additional effect to the accurate diagnosis rate obtained using WLI alone.
In endoscopic therapy for UD-type EGCs, patients were provided with an explanation of the merits and demerits of ESD and gave their informed consent before the operation. An in-hospital consensus has been secured as to the extended therapeutic indications of ESD for UD-type EGCs. This study was approved by the Institutional Review Board of Cancer Institutional Hospital (IRB No. 2014-1048).
Statistical analysis
A comparison between the two groups was performed using the Fisher exact test. The mean and standard deviation of the tumor diameter and the proliferative zone extension distance were calculated and evaluated using the t test and the F test; if the resulting data failed to show a homogeneity of variance, these were evaluated using the Mann–Whitney U test. Any differences were considered to be statistically significant when P < 0.05. The statistical analysis was performed using StatView software, Version 5.0 (SAS Institute, Cary, NC, USA).
Results
Of the 76 lesions that were examined, the diagnostic demarcation by APC marking using ME-NBI was consistent with the histopathological delineation in 62 cases (81.6 %) and was inconsistent in 14 cases (18.4 %). The lesions measured 9.95 ± 6.36 mm in diameter in the accurately diagnosed cases and 19.07 ± 2.75 mm in the misdiagnosed cases; the latter group had a significantly larger tumor size (P < 0.0001). Cases with deep invasion were more frequent among the misdiagnosed cases, although the significance of the difference was relatively weak, and incomplete resections were significantly more frequent among the misdiagnosed cases. The term “complete resection” here denotes an R0 resection, but not a curative resection. As a rule, we regard an R0 resection as a complete resection, provided the intended intervention is an R0 resection, even if the lesion is positive for vascular invasion with SM invasion and/or UL measuring >20 mm in diameter. Conversely, the term “incomplete resection” here means a horizontal (lateral) or vertical margin-positive case and is synonymous in this paper with a horizontal margin-positive case, because the present series did not include any vertical margin-positive cases. Thus, the complete resection rate of 85.5 % in this article refers to the rate of horizontal margin-negative cases. No significant difference was observed between the groups with respect to the proliferative zone extension distance. The mean inter-crypt distance in the proliferative zone extended region in the accurately diagnosed cases was about 1.91 times as long as that in the surrounding normal mucosa, whereas the distance in the misdiagnosed cases was about 1.22 times as long; this difference was statistically significant (P < 0.0001) (Table 1). When compared in terms of background mucosal characteristics according to the Updated Sydney System and grading, no significant differences in atrophy or intestinal epithelial metaplasia were observed between the two groups. However, cases with milder neutrophil and mononuclear cell infiltration had a significantly higher accurate diagnosis rate (P < 0.05) (Table 2). As for the effect of adding ME-NBI data to WLI data, a diagnosis was feasible using WLI alone in 41 cases (53.9 %) and was not feasible or difficult in 35 cases (46.1 %). Among the infeasible or difficult cases, a diagnosis was obtained using ME-NBI in 21 cases (27.6 %), but the diagnosis remained infeasible or difficult in 14 cases (18.5 %). Thus, addition of ME-NBI improved the accurate diagnosis rate by 27.6 %, and the integrated accurate diagnosis rate for UD-type EGCs using ME-NBI and WLI was 81.5 % (Fig. 5).
Additional effect of ME-NBI. Diagnosis with white-light imaging (WLI) was feasible in 41 cases (53.9 %), whereas it was difficult or not feasible for 35 lesions (46.1 %). With magnifying endoscopy combined with NBI (ME-NBI), the diagnosis became feasible for 21 (27.6 %) of these lesions, and the accurate diagnosis rate increased to 81.5 % because of this additive effect
Discussion
The diagnostic demarcation of lesions can be difficult in patients with UD-type EGCs because the proliferative zone extension does not resemble that observed in differentiated-type early gastric cancers [7]. According to reports describing ESD for UD-type EGCs, in fact, the surgical margin-positive rate ranged from 1.7 % to 52.6 % and the curative resection rate ranged from 63.9 % to 82.5 %; hence, both these parameters suggest noticeable inter-institutional differences [11–18]. The curative resection rate has been reported to be 91.1 % for differentiated-type early gastric cancers [19], which seems to be higher than that for UD-type EGCs. A simple comparison of the curative resection rate cannot be performed using the present data because some noncurative resections that were performed because of the size/depth of the tumor and/or the presence of vascular invasion were included; in the afore-described previously reported ESD cases of UD-type EGCs, the surgical margin-positive rate was lower even if the DL was not accurately diagnosed because a perilesional biopsy had been performed or because ESD had been performed by securing a margin ≥10 mm around the lesion [11–18]. Hence, the diagnostic demarcation was accurate among the cases that were regarded as complete resection cases. Nevertheless, the present investigation involved stricter conditions for accurate diagnosis in that DL markings by APC and errors within a 1-mm margin were defined as requirements for accurate diagnosis and were used in the present series. Although a detailed report concerning the accuracy of the diagnostic demarcation of UD-type EGCs has not yet been published, the present results demonstrate that an accurate diagnosis rate of 81.6 % might be achievable using ME-NBI. The accurate diagnostic demarcation rate attained using ME-NBI was considered to be appreciably high, considering that the accurate diagnostic demarcation rate using WLI was 53.9 % and that the aforementioned surgical margin-positive rate was achieved using ESD for UD-type EGCs. Therefore, the present data suggest that the diagnostic capability for UD-type EGCs may be enhanced using the ME-NBI technique, and the use of ME-NBI for the diagnostic delineation of UD-type EGCs lesions before ESD is recommended. Complete resection cases and cases with lesions ≤10 mm were more frequent, the mean inter-crypt distance was longer, and the background mucosal inflammation was milder among the accurately diagnosed cases compared with the misdiagnosed cases. Cell growth potential is reportedly enhanced as a reaction in terms of inflammatory cell infiltration [20–22], and this would imply pronounced cellular mitotic activities via DNA synthesis. In other words, the more pronounced the inflammatory cell infiltration, the greater the likelihood of tumor growth, suggesting that the extension range eventually becomes widened, resulting in an increased tumor diameter. Therefore, it can be inferred that the tumor diameter was significantly smaller in the accurately diagnosed cases inasmuch as the inflammation was milder in those cases. This point was probably reflected in the finding that complete resection cases were significantly more frequent among the cases with milder inflammation. The milder inflammation of the surrounding mucosa implied a relative scarcity of mononuclear cells and neutrophils intruding into the intervening parts, enabling the inter-crypt distance of the surrounding non-carcinomatous mucosa to be retained and causing a distinction from the carcinomatous intervening parts that were extended as a result of the malignant cell intrusion. Consequently, the DL was readily recognizable using ME-NBI. As a matter of fact, the present results suggested that the accurate diagnosis rate increased progressively with an increasing disparity in the inter-crypt distance between the cancerous region and the noncancerous region, because the cancerous/noncancerous region ratio of the inter-crypt distance was about 1.22 times in the misdiagnosed cases compared with about 1.91 times in the accurately diagnosed cases. It follows that it would be difficult to delineate diagnostic demarcation, even using ME-NBI, in cases with a narrower inter-crypt distance in the cancerous region because of the scarcity of cancer cells as well as in cases with pronounced inflammatory cell infiltration, resulting in diagnostic limitations in a little less than 20 % of cases. This finding stresses the need for pretreatment biopsies in surrounding regions, as stated in the Guidelines of the Japanese Gastric Cancer Association [1].
This study has some other limitations. In this study, the ME-NBI diagnosis was performed onsite, but the WLI diagnosis was made by reviewing still images. As stated in the Patients and Methods, this difference was thought to have a minimal influence, because the diagnosis was thought to be correct insofar as the WLI-diagnosed extent coincided with the position of the ME-NBI-based APC-marked region. The present investigation was a single-center study. The lesions were demarcated using APC on the utmost oral and utmost anal sides in this study, but lesion demarcation may be difficult at some other sites or may be more readily accomplished elsewhere.
Although this study was performed at a single center, the results were considered to be notable because our medical institution is a high-volume center where ESD for gastric cancer is performed on more than 300 patients annually, and the subjects included in the present series had been accumulated over 4 years; therefore, these cases were considered to be suitable for an evaluation of relatively uncommon UD-type EGC cases. As well, the present study was considered to be significant because the predetermined placement of markings at the utmost oral and utmost anal sites of the lesion delineation enabled the preclusion of the selective sampling of regions that were readily accessible or difficult to access when demarcating the lesion.
In conclusion, the acceptable error was set at 1 mm because the aim of this study was to clarify the diagnostic accuracy of ME-NBI. If ME-NBI could be shown to have a high diagnostic accuracy, it would enable a more precise determination of the size of a lesion and would prove useful for determining whether ESD is indicated in a particular case. The diagnostic capability for UD-type EGCs may be enhanced using the ME-NBI, and the use of ME-NBI for the diagnostic delineation of UD-type EGCs lesions before to ESD is recommended.
References
Japanese gastric cancer treatment guidelines. Japanese Gastric Cancer Association (ver. 3). Gastric Cancer. 2010;2011(14):113–23.
Gotoda T, Yanagisawa A, Sasako M, Ono H, Nakanishi Y, Shimoda T, et al. Incidence of lymph node metastasis from early gastric cancer: estimation with a large number of cases at two large centers. Gastric Cancer. 2000;4:219–25.
Hirasawa T, Gotoda T, Miyata S, Kato Y, Shimoda Taniguchi H, et al. Incidence of lymph node metastasis and the feasibility of endoscopic resection for undifferentiated-type early gastric cancer. Gastric Cancer. 2009;12:148–52.
Yao K, Iwashita A, Tanabe H, Nagahama T, Matsui T, Ueki T, et al. Novel zoom endoscopy technique for diagnosis of small flat gastric cancer: a prospective, blind study. Clin Gastroenterol Hepatol. 2007;5:869–78.
Yao K, Iwashita A, Kikuchi Y, Yao T, Matsui T, Tanabe H, et al. Novel zoom endoscopy technique for visualizing the microvascular architecture in gastric mucosa. Clin Gastroenterol Hepatol. 2005;7:S23–6.
Yao K, Anagnostopoulos GK, Ragunath K. Magnifying endoscopy for diagnosing and delineating early gastric cancer. Endoscopy. 2009;5:462–7.
Ninomiya Y, Yanagisawa A, Kato Y, Tomimatsu H. Unrecognizable intramucosal spread of diffuse-type mucosal gastric carcinomas of less than 20 mm in size. Endoscopy. 2000;8:604–8.
Nakayoshi T, Tajiri H, Matsuda K, Kaise M, Ikegami M, Sasaki H, et al. Magnifying endoscopy combined with narrow band imaging system for early gastric cancer: correlation of vascular pattern with histopathology (including video). Endoscopy. 2004;12:1080–4.
Okada K, Fujisaki J, Kasuga A, Omae M, Hirasawa T, Ishiyama A, et al. Diagnosis of undifferentiated-type early gastric cancers by magnification endoscopy with narrow-band imaging. J Gastroenterol Hepatol. 2011;26:1262–9.
Dixon MF, Genta RM, Yardley JH, Correa P. Classification and grading of gastritis. The Updated Sydney System. International Workshop on the Histopathology of Gastritis, Houston 1994. Am J Surg Pathol. 1996;20:1161–81.
Kamada K, Tomatsuri N, Yoshida N. Endoscopic submucosal dissection for undifferentiated early gastric cancer as the expanded indication lesion. Digestion. 2012;85:111–5.
Okada K, Fujisaki J, Yoshida T, Ishikawa H, Suganuma T, Kasuga A, et al. Long-term outcomes of endoscopic submucosal dissection for undifferentiated-type early gastric cancer. Endoscopy. 2012;44:122–7.
Abe S, Oda I, Suzuki H, Nonaka S, Yoshinaga S, Odagaki T, et al. Short- and long-term outcomes of endoscopic submucosal dissection for undifferentiated early gastric cancer. Endoscopy. 2013;45:703–7.
Yamamoto Y, Fujisaki J, Hirasawa T, Ishiyama A, Yoshimoto K, Ueki N, et al. Therapeutic outcomes of endoscopic submucosal dissection of undifferentiated-type intramucosal gastric cancer without ulceration and preoperatively diagnosed as 20 mm or less in diameter. Dig Endosc. 2010;22:112–8.
Kim YY, Jeon SW, Kim J, Park JC, Cho KB, Park KS, et al. Endoscopic submucosal dissection for early gastric cancer with undifferentiated histology: could we extend the criteria beyond? Surg Endosc. 2013;12:4656–62.
Kang HY, Kim SG, Kim JS, Jung HC, Song IS. Clinical outcomes of endoscopic submucosal dissection for undifferentiated early gastric cancer. Surg Endosc. 2010;24:509–16.
Kim JH, Lee YC, Kim H, Song KH, Lee SK, Cheon JH, et al. Endoscopic resection for undifferentiated early gastric cancer. Gastrointest Endosc. 2009;69:e1–9.
Park YD, Chung YJ, Chung HY, Yu W, Bae HI, Jeon SW, et al. Factors related to lymph node metastasis and the feasibility of endoscopic mucosal resection for treating poorly differentiated adenocarcinoma of the stomach. Endoscopy. 2008;40:7–10.
Yamaguchi N, Isomoto H, Fukuda E, Ikeda K, Nishiyama H, Akiyama M, et al. Clinical outcomes of endoscopic submucosal dissection for early gastric cancer by indication criteria. Digestion. 2009;80:173–81.
Uemura N, Okamoto S, Yamamoto S, Matsumura N, Yamaguchi S, Yamakido M, et al. Helicobacter pylori infection and the development of gastric cancer. N Engl J Med. 2001;345:784–9.
Ito M, Tanaka S, Takata S, Oka S, Imagawa S, Ueda H, et al. Morphological changes in human gastric tumors after eradication therapy of Helicobacter pylori in a short-term follow-up. Aliment Pharmacol Ther. 2005;21:559–66.
Tanaka A, Kamada T, Inoue K, Shiotani A, Kusunoki H, Manabe N, et al. Histological evaluation of patients with gastritis at the high risk of developing gastric cancer using a conventional index. Pathol Res Pract. 2011;207:354–8.
Conflict of interest
There is no conflict of interest in this study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Horiuchi, Y., Fujisaki, J., Yamamoto, N. et al. Accuracy of diagnostic demarcation of undifferentiated-type early gastric cancers for magnifying endoscopy with narrow-band imaging: endoscopic submucosal dissection cases. Gastric Cancer 19, 515–523 (2016). https://doi.org/10.1007/s10120-015-0488-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10120-015-0488-x