Abstract
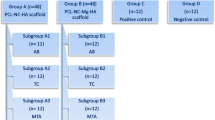
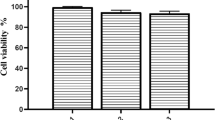
This study aimed to investigate the potential of low-level laser irradiation (LLLI) to promote odontogenic differentiation and biomineralization by dental pulp stem cells (DPSCs) seeded inside bioceramic scaffolds. Mg-based, Zn-doped bioceramic scaffolds, synthesized by the sol–gel technique, were spotted with DPSCs and exposed to LLLI at 660 nm with maximum output power of 140 mw at fluencies (a) 2 and 4 J/cm2 to evaluate cell viability/proliferation by the MTT assay and (b) 4 J/cm2 to evaluate cell differentiation, using real-time PCR (expression of odontogenic markers) and a p-nitrophenylphosphate (pNPP)-based assay for alkaline phosphatase (ALP) activity measurement. Scanning electron microscopy (SEM) and X-ray diffraction (XRD) analysis were used for structural/chemical characterization of the regenerated tissues. Exposure of the DPSCs/scaffold complexes to the proposed LLLI scheme was associated with statistically significant increase of odontogenesis-related markers (bone morphogenetic protein 2 (BMP-2): 22.4-fold, dentin sialophosphoprotein (DSPP): 28.4-fold, Osterix: 18.5-fold, and Runt-related transcription factor 2 (Runx2): 3.4-fold). ALP activity was significantly increased at 3 and 7 days inside the irradiated compared to that in the non-irradiated SC/DPSC complexes, but gradually decreased until 14 days. Newly formed Ca-P tissue was formed on the SC/DPSC complexes after 28 days of culture that attained the characteristics of bioapatite. Overall, LLLI treatment proved to be beneficial for odontogenic differentiation and biomineralization of DPSCs inside the bioceramic scaffolds, making this therapeutic modality promising for targeted dentin engineering.





Similar content being viewed by others
References
Mester E, Mester AF, Mester A (1985) The biomedical effects of laser application. Lasers Surg Med 5:31–39
Amid R, Kadkhodazadeh M, Ahsaie MG, Hakakzadeh A (2014) Effect of low level laser therapy on proliferation and differentiation of the cells contributing in bone regeneration. J Lasers Med Sci 5:163–170
Khan I, Arany P (2014) Biophysical approaches for oral wound healing: emphasis on photobiomodulation. Adva Wound Care 4:724–737
Rola P, Doroszko A, Derkacz A (2014) The use of low-level energy laser radiation in basic and clinical research. Adv Clin Exp Med 23:835–842
Asnaashari M, Safavi NJ (2013) Application of low level lasers in dentistry (endodontic). Lasers Med Sci 4:57–66
Karu TI (2008) Mitochondrial signaling in mammalian cells activated by red and near IR radiation. Photochem Photobiol 84:1091–1099
Lane N (2006) Power games. Nature 443:901–903
Zhang Y, Song S, Fong CC, Tsang CH, Yang Z, Yang M (2003) cDNA microarray analysis of gene expression profiles in human fibroblast cells irradiated with red light. J Invest Dermatol 120:849–857
Smith KC (1991) The photo biological basis of low level laser radiation therapy. Laser Therapy 3:19–24
Huang YY, Chen AC, Carroll JD, Hamblin MR (2009) Biphasic dose response in low level light therapy. Dose Response 7:358–383
Pandeshwa P et al (2015) Photobiomodulation in oral medicine: a review. J Invest Clin Dent: 1–12
Kufler D (2016) Photobiomodulation in promoting wound healing: a review. Regen Med
Gupta A, Dai T, Hamblin MR (2014) Effect of red and near infrared wavelengths on low-level laser (light) therapy-induced healing of partial-thickness dermal abrasion in mice. Lasers Med Sci 29:257–265
Alipanah Y, Asnaashari M, Anbari F (2011) The effect oflow level laser (GaAlAs) therapy on the post-surgicalhealing of full thickness wounds in rabbits. Med Laser Appl 26:133–138
Saygun I, Karacay S, Serdar M, Ural AU, Sencimen M, Kurtis B (2008) Effects of laser irradiation on the release of basic fibroblast growth factor (bFGF), insulin like growth factor-1 (IGF-1), and receptor of IGF-1 (IGFBP3) from gingival fibroblasts. Lasers Med Sci 23:211–215
Fabre HSC, Navarro RL, Oltramari-Navarro PVP, Oliveira RF, Pires-Oliveira DAA et al (2015) Anti-inflammatory and analgesic effects of low-level laser therapy on the postoperative healing process. J PhysTher Sci 27(6):1645–1648
Zecha JA, Raber-Durlacher JE, Nair RG, Epstein JB, Elad S, Hamblin MR et al (2016) Low-level laser therapy/photobiomodulation in the management of side effects of chemoradiation therapy in head and neck cancer: part 2: proposed applications and treatment protocols. Support Care Cancer 24:2793–2805
Egusa H, Sonoyama W, Nishimura M, Atsuta I, Akiyama K (2012) Stem cells in dentistry—part I: stem cell sources. J Prosthodont Res 56:151–165
Goudouri OM, Theodosoglou E, Kontonasaki E, Will J, Chrissafis K et al (2014) Development of highly porous scaffolds based on bioactive silicates for dental tissue engineering. Mater Res Bull 49:399–404
Qu T, Jing J, Jiang Y, Taylor RJ, Feng JQ, Geiger B, Liu X (2014) Magnesium-containing nanostructured hybrid scaffolds for enhanced dentin regeneration. Tissue Eng Part A 20:2422–2433
Theodorou GS, Kontonasaki E, Theocharidou A, Bakopoulou A, Bousnaki M, Hatjichristou C (2016) Synthesis and study of biomimetic ceramic scaffolds towards dental stem cell differentiation and calcified dental tissue engineering. Inter J Biomater, ID 3858301
Huang Y, Jin X, Zhang X, Sun H, Tu J, Tang T, Chang J, Dai K (2009) In vitro and in vivo evaluation of akermanite bioceramics for bone regeneration. Biomaterials 30:5041–5048
Manzano-Moreno FJ, Medina-Huertas R, Ramos-Torrecillas J, Garcνa-Martνnez O, Ruiz C et al (2015) The effect of low-level diode laser therapy on early differentiation of osteoblast via BMP-2/TGF-β1 and its receptors. J Cranio-Maxillo-Facial Surg 43:1926–1932
Bakopoulou A, Leyhausen G, Volk J, Papachristou E, Koidis P, Geurtsen W (2015) Wnt/β-catenin signaling regulates dental pulp stem cells’ responses to pulp injury by resinous monomers. Dent Mater 31:542–555
Chen S, Gluhak-Heinrich J, Wang YH, Wu YM, Chuang HH et al (2009) Runx2, osx, and dspp in tooth development. J Dent Res 88:904–909
Kontonasaki E, Bakopoulou A, Theocharidou A, Theodorou GS, Papadopoulou L et al (2015) Effective cell growth potential of Mg-based bioceramic scaffolds towards targeted dentin regeneration. Balk J Dent Med 19:75–85
Karu TI, Kolyakov SF (2005) Exhact action spectra for cellular responses relevant to phototherapy. Photomed Laser Surg 23:355–361
Giannelli M, Chellini F, Sassoli C, Francini F, Pini A et al (2013) Photoactivation of bone marrow mesenchymal stromal cells with diode laser: effects and mechanisms of action. J Cell Physiol 228:172–181
Cerdeira CD, Brigagão RPL, Carli ML, de Souza Ferreira C, Moraes GOI, Hadad H, Hanemann JAC, Hamblin MR, Sperandio FF (2016) Low-level laser therapy stimulates the oxidative burst in human neutrophils and increases their fungicidal capacity. J Biophotonics 1–9 /. doi: 10.1002/jbio.201600035
Arany PR (2016) Craniofacial wound healing with photobiomodulation therapy: new insights and current challenges. J Dent Res: 1–8. doi: 10.1177/0022034516648939
Kushibiki T, Hirasawa T, Okawa S, Ishihara M (2015) Low reactive level laser therapy for mesenchymal stromal cells therapies. Stem Cells Int: 864-974
Feng J, Sun Q, Liu L, Xing D (2015) Photoactivation of TAZ via Akt/GSK3β signaling pathway promotes osteogenic differentiation. Int J Biochem Cell Biol 66:59–68
Pan K, Sun Q, Zhang J, Ge S, Li S, Zhao Y et al (2010) Multilineage differentiation of dental follicle cells and the roles of Runx2 over-expression in enhancing osteoblast/cementoblast-related gene expression in dental follicle cells. Cell Prolif 43:219–228
Hoppe A, Gόldal NS, Boccaccini A (2011) A review of the biological response to ionic dissolution products from bioactive glasses and glass-ceramics. Biomaterials 32:2757–2774
Hoppe A, Mouriρo V, Boccaccini A (2013) Therapeutic inorganic ions in bioactive glasses to enhance bone formation and beyond. Biomater Sci 1:254–256
Goel A, Kapoor S, Tilocca A, Rajagopal RR, Ferreira JMF (2013) Structural role of zinc in biodegradation of alkali-free bioactive glasses. J Mater Chem B 1:3073–3082
Engel KW, Khan I, Arany PR (2016) Cell lineage responses to photobiomodulation therapy. J Biophotonics. doi:10.1002/jbio.201600025
Eduardo F, Bueno D, Freitas P, Marques M, Passos Bueno M (2008) Stem cell proliferation under low intensity laser irradiation: a preliminary study. Lasers Surg Med 40:433–438
Hou JF, Zhang H, Yuan X, Li J, Wei YJ, Hu SS (2008) In vitro effects of low-level laser irradiation for bone marrow mesenchymal stem cells: proliferation, growth factors secretion and myogenic differentiation. Lasers Surg Med 40:726–733
Wu JY, Wang YH, Wang GJ, Ho ML, Wang CZ, Yeh ML, Chen CH (2012) Low-power GaAlAs laser irradiation promotes the proliferation and osteogenic differentiation of stem cells via IGF1 and BMP2. PLoS One 7:e44027
Pyo SJ, Song WW, Kim IR, Park BS, Kim CH et al (2013) Low-level laser therapy induces the expressions of BMP-2, osteocalcin, and TGF-β1 in hypoxic-cultured human osteoblasts. Lasers Med Sci 28:543–550
Hirata S, Kitamura C, Fukushima H, Nakamich I, Abiko Y, Terashita M, Jimi E (2010) Low-level laser irradiation enhances bmp-induced osteoblast differentiation by stimulating the BMP/Smad signaling pathway. J Cel Biochem 111:1445–1452
Soleimani M, Abbasnia E, Fathi M, Sahraei H, Fathi Y, Kaka G (2012) The effects of low-level laser irradiation on differentiation and proliferation of human bone marrow mesenchymal stem cells into neurons and osteoblasts—an in vitro study. Lasers Med Sci 27:423–430
de Villiers JA, Houreld NN, Abrahamse H (2015) Influence of low intensity laser irradiation on isolated human adipose derived stem cells over 72 hours and their differentiation potential into smooth muscle cells using retinoic acid. Stem Cell Rev 201(7):869–882
Acknowledgments
This study was conducted under the action Excellence II (Project: 5105) and funded by the European Union (EU) and National Resources.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics statement
All donors provided their written consent to participate in the study. The written consent form had been approved by the ethics committee of the School of Dentistry, of the Aristotle University of Thessaloniki. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional ethics committee and with the 1964 Helsinki declaration and its later amendments.
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Theocharidou, A., Bakopoulou, A., Kontonasaki, E. et al. Odontogenic differentiation and biomineralization potential of dental pulp stem cells inside Mg-based bioceramic scaffolds under low-level laser treatment. Lasers Med Sci 32, 201–210 (2017). https://doi.org/10.1007/s10103-016-2102-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10103-016-2102-9