Abstract
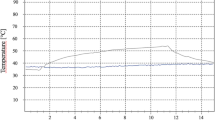
The implant surgery consists of two distinct techniques, the transmucosal, also known as “one-stage” and the “two-stage” technique. Lasers represent a possible aid in implant dentistry, especially in the two-stage technique and its main characteristics are represented by a decreased trauma to bone and soft tissues, a reduction of pain as well as a reduction of the risk of postoperative infections. The aim of this study was to analyze in an animal model the thermal elevation induced by four different laser wavelengths (diode, Nd:YAG, Er:YAG, KTP) during the implant uncovering. Four pig jaws were used to carry out this study. Five implants were placed in each anatomical specimen for a total of 20 fixtures. Four wavelengths (532, 810, 1,064 and 2,940 nm) were used to uncover the implants. Two thermocouples were used to measure temperature changes during laser irradiation at bone level, peri-implant tissues and on the fixture surface The thermocouples were connected with two probes of 1.5 mm in diameter, in order to simultaneously recording two temperature variations. Surface temperature was also checked during all procedures with a thermal camera (Thermovision A 800, Flyr Systems, Stockolm, Sweden) connected to a PC. The mean temperatures of each specimen (five fixtures) were calculated (TM1, mean temperature at the beginning; TM2, mean peak temperature). Furthermore, a record of the temperature at 1 min after the end of the surgical procedure was taken (mean: TM3). All the recorded values were statistically evaluated by one-way analysis of variance (ANOVA). The thermocouples recorded a lower increase in temperature for Er:YAG and KTP laser; Nd:YAG and diode laser produced similar increases characterized by higher values. The thermo-camera pointed out the lower increase for Er:YAG and higher for diode laser. KTP laser resulted faster in uncovering implants and diode laser was the one that needed more time. This ex vivo study showed that laser utilization with the recommended parameters gives no risks of dangerous thermal elevation to the tissues and implants.







Similar content being viewed by others
References
Kreisler M, Kohnen W, Marinello C, Götz H, Duschner H, Jansen B, d’Hoedt B (2002) Bactericidal effect of the Er: YAG laser on dental implant surfaces: an in vitro study. J Periodontol 73(11):1292–8
Romanos GE, Gutknecht N, Dieter S, Schwarz F, Crespi R, Sculean A (2009) Laser wavelengths and oral implantology. Lasers Sci Med 24(6):961–70
Parker S. (2007) Surgical laser use in implantology and endodontics. Br Dent J. 14, 202 (7) :377–86
Lindhe J, Karring T, Lang Niklaus P (2009) Clinical periodontology and oral implantology Vol II, ch. 36–42- Edi. Hermes, Italy
Vanheusden A. (2001) Impression technics in implantology. Rev Belge Med Dent., 56 (3) :189–203. French.
Garg AK, Vicari A (1994) Concepts in impressions for dental implantology. Implant Soc 5(2):11–6
Bornstein E (2003) Combining multiple technologies to perform minimally invasive laser-assisted dental implant surgery. Dent Today 22(6):52–5
Yeh S, Jain K, Andreana S (2005) Using a diode laser to uncover dental implants in second-stage surgery. J Dent 53(6):414–7
Arnabat-Domínguez J, España-Tost AJ, Berini-Aytes L, Gay EC (2003) Erbium: YAG laser application in the second phase of implant surgery: a pilot study of 20 patients. Int J Oral Maxillofac Implants 18(1):104–12
Dörtbudak O, Haas R, Mallath-Pokorny G (2000) Biostimulation of bone marrow cells with a diode soft laser. Clin Oral Implants Res 11(6):540–5
Schwarz F, Aoki A, Sculean A, Becker J. (2009) the impact of laser application on periodontal and peri-implant wound healing. Periodontol; 51:79–108. Review
Moy PK, Weinlaender M, Kennedy EB (1989) Modifications of soft-tissue surgical techniques for placement and uncovering of osseointegrated implants. Dent Clin North Am 33(4):665–81
Barber HD, Seckinger RJ, Silverrstein K, Abughazaleh K (1996) Comparison of soft tissue healing and osseointegration of IMZ implants placed in one- stage and two stage techniques: a pilot study. Implant Dent Spring 5(1):11–4
Martin E (2004) Lasers in dental implantology. Dent Clin North Am 48(4):999–1015
Arnabat-Domínguez J, Bragado-Novel M, España-Tost AJ, Berini-Aytes L, Gay-Escoda C (2010) Advantages and esthetic results of erbium, chromium: yttrium-scandium-gallium-garnet laser application in second-stage implant surgery in patients with insufficient gingival attachment: a report of three cases. Lasers Sci Med 25(3):459–64
Deppe H, Horch HH. (2007) Laser applications in oral surgery and implant dentistry. Lasers Med Sci., 22 (4) :217–21. Epub 2007 Feb. 1. Review
Yeh S, Jain K, Andreana S (2005) Using a diode laser to uncover dental implants in second-stage surgery. J Dent 53(6):414–7
Wilcox CW, Wilwerding TM, Watson P, Morris JT (2001) Use of electrosurgery and lasers in the presence of dental implants. Int J Oral Maxillofac Implants 16(4):578–82
Vassalli M, Giannelli M (2003) Effect of Nd: YAG laser on titanium dental implants studied by AFM. Ital J Anat Embryol 108(4):195–203
Schwarz F, Rothamel D, Becker J. (2003) Influence of an Er: YAG laser on the surface structure of titanium implants. Schweiz Monatsschr Zahnmed., 113 (6) :660–71. French, Germany
Park CY, Kim SG, Kim MD, Eom TG, Yoon JH, Ahn SG (2005) Surface properties of endosseous dental implants after Nd: Yag and CO2 laser treatment at various energies. J Oral Maxillofac Surg 63(10):1522–7
Kusek ER. (2006) Use of the YSGG laser in dental implant surgery: scientific rationale and case reports. Dent Today; 25 (10): 98, 100, 102–3
Joob Fancsaly A, Divinyi T, Fazekas A, Peto G, Karacs A. (2000) Surface treatment of dental implants with high-energy laser beam. Fogorv Sz.; 93 (6) :169–80. Hungarian
Romanos GE, Everts H, Nentwig GH (2000) Effects of diode and Nd: YAG laser irradiation on titanium discs: a scanning electron microscope examination. J Periodontol 71(5):810–5
Kreisler M, Al Hay H, D’Hoedt B (2003) Temperature changes induced by 809-nm GaAlAs laser at the implant-bone interface during simulated surface decontamination. Clin Oral Implants Res 14(1):91–6
Oyster DK, Parker WB, Gher ME (1995) CO2 lasers and temperature changes of titanium implants. J Periodontol 66(12):1017–24
Mouhyi J, Sennerby L, Nammour S, Guillaume P, Van Reck J (1999) Temperature increases during decontamination of titanium surface using CO2 laser. Clin Oral Implants Res 10(1):54–61
Wooten CA, Sullivan SM, Supure S (1999) Heat generation by superpulsed CO2 laser on plasma-sprayed titanium implants: an in vitro study. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 88(5):544–8
Kreisler M, Götz H, Duschner H (2002) Effect of Nd: YAG, Ho: YAG, Er: YAG, CO2, and GaAIAs laser irradiation on surface properties of endosseous dental implants. Int J Oral Maxillofac Implants 17(2):202–11
Fornaini C, Rocca JP, Merigo E, Meleti M, Manfredi M, Nammour S, Vescovi P (2012) Low energy KTP laser in oral soft tissue surgery: a 52 patients clinical study. Med Oral Patol Oral Cir Bucal 17(2):e287–91
Esposito M, Grusovin MG, Maghaireh H, Coulthard P, Worthington HV. (2007) Interventions for replacing missing teeth: management of soft tissues for dental implants. Cochrane Database Syst Rev. 18;(3):CD006697. Review. Update in: Cochrane Database Syst Rev. 2012;2:CD006697
Gómez-Santos L, Arnabat-Domínguez J, Sierra-Rebolledo A, Gay-Escoda C (2010) Thermal increment due to ErCr: YSGG and CO2 laser irradiation of different implant surfaces. A pilot study. Med Oral Patol Oral Cir Bucal 15(5):e782–e787
Sun H, Mikula E, Kurtz RM, Juhasz T (2010) Temperature increase in human cadaver retina during direct illumination by femtosecond laser pulses. J Refract Surg 26(4):272–277
George J, Bensafi A, Schmitt AM, Black D, Dahan S, Loche F, Lagarde JM (2008) Validation of a non-contact technique for local skin temperature measurements. Skin Res Technol 14(4):381–384
Wang X, Ishizaki NT, Matsumoto K (2005) Healing process of skin after CO2 laser ablation at low irradiance: a comparison of continuous-wave and pulsed mode. Photomed Laser Surg 23(1):20–26
Romanos G, Pelekanos S, Strub JR (1995) Effects of Nd: YAG laser on wound healing processes: clinical and immunohistochemical findings in rat skin. Lasers in Surgery and Medicine 16:368–379
Romeo U, Libotte F, Palaia G, Del Vecchio A, Tenore G, Visca P, Nammour S, Polimeni A (2012) Histological in vitro evaluation of the effects of Er: YAG laser on oral soft tissues. Lasers Med Sci 27(4):749–53
Romeo U, Palaia G, Del Vecchio A, Tenore G, Gambarini G, Gutknecht N, De Luca M (2010) Effects of KTP laser on oral soft tissues. An in vitro study. Lasers Med Sci 25(4):539–43
G. Palaia, A. Del Vecchio, A. Impellizzeri, G. Tenore, P. Visca, F. Libotte, C. Russo, and U. Romeo (2014): Histological ex vivo evaluation of peri-incisional thermal effect created by a new-generation CO2 superpulsed laser. The Scientific World Journal, ID 345685
Niemz MH (2007) Laser-tissue interactions. Fundamentals and applications. 3rd edn, Springer
Sperandio FF, Meneguzzo DT, Ferreira LS, da Ana PA, Azevedo LH, de Sousa SC (2011) Different air–water spray regulations affect the healing of Er, Cr: YSGG laser incisions. Lasers Med Sci 26(2):257–265
Merigo E, Clini F, Fornaini C, Oppici A, Paties C, Zangrandi A, Fontana M, Rocca JP, Meleti M, Manfredi M, Cella L, Vescovi P (2013) Laser-assisted surgery with different wavelengths: a preliminary ex vivo study on thermal increase and histological evaluation. Lasers Med Sci 28(2):497–504
Oelgiesser D, Blasbalg J, Ben-Amar A (2003) Cavity preparation by Er-YAG laser on pulpal temperature rise. Am J Dent 16(2):96–98
Martins GR, Cavalcanti BN, Rode SM (2006) Increases in intrapulpal temperature during polymerization of composite resin. J Prosthet Dent 96(5):328–331
Sulieman M, Rees JS, Addy M (2006) Surface and pulp chamber temperature rises during tooth bleaching using a diode laser: a study in vitro. Br Dent J 200(11):631–634
Augustin G, Davila S, Mihoci K, Udiljak T, Vedrina DS, Antabak A (2008) Thermal osteonecrosis and bone drilling parameters revisited. Arch Orthop Trauma Surg 128(1):71–77
Augustin G, Davila S, Udiljak T, Vedrina DS, Bagatin D (2009) Determination of spatial distribution of increase in bone temperature during drilling by infrared thermography: preliminary report. Arch Orthop Trauma Surg 129(5):703–709
El-Kholey KE. (2013) Efficacy and safety of a diode laser in second-stage implant surgery: a comparative study. Int J Oral Maxillofac Surg. 6. pi:S0901-5027 (13) 01113-2
Miserendino LJ, Abt E, Wigdor H, Miserendino CA (1993) Evaluation of thermal cooling mechanisms for laser application to teeth. Lasers Surg Med 13(1):83–88
Geminiani A, Caton JG, Romanos GE (2011) Temperature change during non-contact diode laser irradiation of implant surfaces. Lasers Med Sci 27(2):339–342
Di Bernardo BE, Reyes J, Chen B (2009) Evaluation of tissue thermal effects from 1064/1320-nm laser-assisted lipolysis and its clinical implications. J Cosmet Laser Ther 11(2):62–69
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Fornaini, C., Merigo, E., Vescovi, P. et al. Different laser wavelengths comparison in the second-stage implant surgery: an ex vivo study. Lasers Med Sci 30, 1631–1639 (2015). https://doi.org/10.1007/s10103-014-1623-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10103-014-1623-3