Abstract
This review summarizes evidence that commercially available fluoroquinolones used for the treatment of bacterial infections are active against other non-bacterial infectious agents as well. Any of these fluoroquinolones exerts, in parallel to its antibacterial action, antiviral, antifungal, and antiparasitic actions at clinically achievable concentrations. This broad range of anti-infective activities is due to one common mode of action, i.e., the inhibition of type II topoisomerases or inhibition of viral helicases, thus maintaining the selective toxicity of fluoroquinolones inhibiting microbial topoisomerases at low concentrations but mammalian topoisomerases at much higher concentrations. Evidence suggests that standard doses of the fluoroquinolones studied are clinically effective against viral and parasitic infections, whereas higher doses administered topically were active against Candida spp. causing ophthalmological infections. Well-designed clinical studies should be performed to substantiate these findings.
Similar content being viewed by others
Introduction
The history of quinolones began in 1962 with the isolation of a byproduct of chloroquine synthesis by George Yohe Lesher and colleagues [1] at the Sterling-Winthrop Research Institute in Rensselaer, New York; this compound was found to be antibacterially active and was subsequently modified to yield nalidixic acid. Nalidixic acid and chloroquine share structural features being essential for their antibacterial and antiparasitic activity, respectively. Apart from its well-known antimalarial effects [2–4], chloroquine exerts direct antiviral [5–13], antifungal [13–16], and antibacterial effects [13, 17–20]. Furthermore, chloroquine exhibits immunomodulatory activity [21–25] and was found to reverse P-glycoprotein (P-gp)-mediated multidrug resistance, thereby increasing the cytotoxicity of some antineoplastic agents [26–30]. The antimalarial effects of chloroquine are due to its accumulation in acidic food vacuoles of intraerythrocytic trophozoites, thereby preventing hemoglobin degradation and inhibition of a haem polymerase enzyme [3, 4]. The antiviral, antifungal, and antibacterial activities of chloroquine are pH-dependent [10, 14, 16, 18]. This phenomenon is due to the fact that chloroquine is a weak base and, therefore, does not enter the cell if the extracellular fluid or the incubation medium is acidic. Once chloroquine has entered cells, it intercalates into DNA and prevents the introduction of topoisomerase II-mediated DNA breaks. The intercalation of chloroquine into DNA protects cells against epipodophyllotoxins such as etoposide, acting as topoisomerase II poison by hindering the DNA cleavage reaction of this target enzyme [31, 32]. The use of chloroquine in the treatment of some autoimmune diseases and its anti-inflammatory properties may be due to the inhibition of MHC class II antigen presentation; the inhibition of T-cell response may be due to a direct interaction of chloroquine with the cell membrane [22]. Furthermore, chloroquine was found to destabilize indirectly lysosomal and plasma membranes as a result of accumulation within the lysosome, followed by an increase in lysosomal volume; it also sequesters important cell membrane constituents in lysosomes [29]. Chloroquine was found to adsorb to the plasma membrane of yeasts, inhibit competitively the binding of immunoglobulin G to the cell surface, altered phospholipid turnover, and influenced directly but non-specifically the membrane integrity and permeability of renal brush border vesicles, mast cell membranes, and fibroblasts [16, 33–35]. Furthermore, chloroquine blocks the inward rectifier potassium channel Kir2.1; it is bound at the center of the cytoplasmic domain of the channel [36, 37]. These data demonstrate that the congener of fluoroquinolones, i.e., chloroquine, exhibits, apart from its antimalarial activity, pleiotropic actions and interacts with multiple targets.
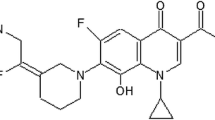
As chloroquine and nalidixic acid share structural features being essential for their activity, it was not surprising that it has been recognized in the late 1980s that nalidixic acid and oxolinic acid derivatives exert trypanocidal and antitumor activities [38]; in the early 1990s, it was described that fluoroquinolones used for the treatment of bacterial infections exert not only an antibacterial but also an antiprotozoal activity [39] and may find applications as antiparasitic, antifungal, or antiviral agents [40]. Furthermore, and in analogy to chloroquine, the activity of antibacterially active fluoroquinolones is pH-dependent [41], and they bind directly to bacterial DNA, i.e., two molecules intercalate at the highly bent DNA gate in the DNA cleavage domain [42–46]. Despite these phenotypic and molecular homologies between chloroquine and fluoroquinolones, the pharmaceuticals industry invested financial and human resources into focused research programs on the application of developmental fluoroquinolones as antibacterials only and into pre- and postmarketing studies supporting the use of fluoroquinolones in the once-granted indications. Studies on the function of an antibacterial agent exerting pleiotropic anti-infective actions have never been performed systematically. Surprisingly, the use of fluoroquinolones in indications other than bacterial infections has never been exploited, although not only nalidixic acid and its congener chloroquine exerts pleiotropic actions but, e.g., β-lactams and aminoglycosides are characterized by a broad range of biological activities too [47, 48], so that a multitude of antimicrobial effects would not have been unusual.
This review summarizes the pleiotropic phenotypes of non-antibacterial actions of fluoroquinolones and addresses the question if the diversity of effects are due to one common mode of action of antibacterially active fluoroquinolones, i.e., inhibition of essential bacterial type II topoisomerases, or if other mechanisms may mediate non-antibacterial activities. Although the complexity and diversity of prokaryotic and eukaryotic topoisomerases is remarkable and little or no sequence homology of amino acids exists, type I and type II topoisomerases share certain structural elements mediating identical functions like DNA relaxation or DNA transport in bacteria, DNA viruses, yeasts, and parasites; the DNA helicase coordinates the directionality of topoisomerase activity; RNA helicases as present, e.g., in hepatitis C virus (HCV) directly interact with double-stranded DNA or RNA and assembles complexes with type II topoisomerases [49–53]. As DNA topoisomerases are ubiquitous enzymes controlling DNA topology, it is conceivable that antibacterially active quinolones may not only inhibit the growth of bacteria at clinically relevant concentrations, but that of other prokaryotic and even eukaryotic organisms as well.
Antiviral activities of fluoroquinolones
Ciprofloxacin, ofloxacin, levofloxacin, and gatifloxacin were found to be clinically effective in the treatment of the single-stranded RNA HCV and the non-enveloped, encapsulated DNA polyomavirus BK [54–60]. Five and four patients with HCV-induced chronic hepatitis and compensated liver cirrhosis, respectively, were treated with 100 to 900 mg ofloxacin per day for one to eight weeks. In three patients with chronic hepatitis and one patient with compensated liver cirrhosis, HCV RNA decreased at least by 1 log titer [54]. In another study, five patients with chronic HCV were treated with 500 mg ciprofloxacin twice daily (b.i.d.) for 30 days. Serum HCV RNA levels remained largely unchanged in these patients [55]. The latter study indicates that the anti-HCV efficacy of quinolones may be limited in patients with advanced liver cirrhosis. Ciprofloxacin decreased BK peak viral load after hematopoietic stem cell transplantation [56]. A reduction of viremia was demonstrated two months after a 10-day course of gatifloxacin at 400 mg/d in 7 of 10 transplant recipients with active BK virus replication [57]. A retrospective analysis revealed that the use of either ciprofloxacin 250 mg b.i.d. or levofloxacin 250 mg once daily (q.d.) within the first month post transplantation and up to 3 months after transplantation was associated with significantly lower one-year rates of BK viremia [58]. A recent study in nine kidney transplant recipients with persistent BK infection revealed that, three months post ciprofloxacin treatment with 250 mg b.i.d for 30 days, the virus load was cleared completely in three patients and decreased by >50 % in another three patients [59]; patients were not treated with anti-infectives other than fluoroquinolones.
Fluoroquinolones inhibit BK viral replication in vitro. Ofloxacin and levofloxacin inhibited polyomavirus BK replication in primary human kidney cells in a dose-dependent manner, yielding a ~90 % inhibition at 150 μg/ml. BK virus genome replication was reduced by 77 % at 48 h post infection of the kidney cells. At 72 h after inoculation of the kidney cells, the reduction in genome replication and protein expression was less pronounced. A dose-dependent cytostatic effect was noted. In infected cells, 150 mg/L ofloxacin led to a 26 % and 6 % inhibition of cellular DNA replication and total metabolic activity, respectively, while 150 mg/L levofloxacin exhibited a slightly more marked cytostatic effect, particularly in uninfected cells [60]. Ciprofloxacin, moxifloxacin, levofloxacin, ofloxacin, gatifloxacin, and norfloxacin inhibited BK virus replication to 50 % at concentrations ranging from 66.7 to 266.6 mg/L [61]. Ciprofloxacin, ofloxacin, levofloxacin, gatifloxacin, and trovafloxacin inhibited viral replication of simian virus 40 (SV40), another member of the polyomaviridae, in permissive monkey cells, as well as plaque formation, DNA replication, and helicase activity. Ciprofloxacin, levofloxacin, and ofloxacin inhibited “significantly” helicase activity at 0.5, 1.0, and 2.0 mM, whereas trovafloxacin inhibited helicase activity at 50 μM [62, 63]. Recently, it was demonstrated that norfloxacin, ofloxacin, flumequine, enrofloxacin, cinoxacin, enoxacin, fleroxacin, lomefloxacin, balofloxacin, and difloxacin inhibited HCV replication, in particular, hepatoma Huh-7 and Huh-8 cell lines, and HCV NS3 helicase activity. The concentrations inhibiting HCV RNA replication to 50 % ranged from 3.3 to 8.2 μM and those inhibiting helicase activity ranged from 4.1 to 9.9 μM [64].
The clinical studies reviewed above and one recent report of a successful treatment of a kidney retransplant patient with ciprofloxacin (250 mg b.i.d. for 10 days) who needed an overall increase of immunosuppression due to acute rejection [65] suggest that fluoroquinolone treatment of polyomavirus BK infections in transplant patients may be beneficial. Therefore, a study protocol for a randomized controlled clinical trial evaluating the prophylactic efficacy of fluoroquinolones has been designed and is registered at ClinicalTrials.gov under NCT01353339; levofloxacin at a dose of 500 mg q.d. will be administered for 3 months and will be compared to placebo [66]. Another clinical study on the use of ciprofloxacin (250 mg q.d. for 3 months as compared to placebo) for the prevention of BK infections is registered under NCT01789203 [67].
Furthermore, it was demonstrated that ofloxacin [68] and levofloxacin [69] inhibited viral topoisomerase activity of vaccinia virus but not of herpes simplex virus and influenza virus [68]. In agreement with this finding, it was reported that 200 mg/L each of ciprofloxacin, lomefloxacin, ofloxacin, pefloxacin, and rufloxacin inhibited to 50 % the cytopathic effect of herpes simplex virus type 2 at concentrations being equivalent to the cytotoxic effect of the quinolones on the Vero cells [70]. Fluoroquinolones inhibit not only enzymic activity of viral topoisomerases/helicases, but inhibit in vitro human immunodeficiency virus (HIV) reverse transcriptase as well; complete inhibition was observed at concentrations of ciprofloxacin and ofloxacin of 3 μM and norfloxacin of 1 μM, respectively [71–73].
Inhibition of rhinovirus (RV) infection by quinolones is due to the inhibition of cell functions required for viral replication. Levofloxacin pretreatment of not yet infected human tracheal epithelial cells reduced the mRNA level of intercellular adhesion molecule 1 (ICAM-1), a receptor for RV, in the cells and the concentration of the soluble form of ICAM-1 in the supernatant, so that RV infection of the tracheal epithelial cells was significantly reduced. Levofloxacin pretreatment also decreased the number of the acidic endosomes from which RV RNA enters the cytoplasm. Furthermore, levofloxacin pretreatment inhibited the activation of nuclear factor κB proteins. These data suggest that levofloxacin inhibits RV infections first by reducing ICAM-1 expression levels and the number of acidic endosomes, and second by modulating airway inflammation [74]. Fluoroquinolones other than levofloxacin have not been studied in this context.
Antifungal activities of fluoroquinolones
Moxifloxacin and gatifloxacin inhibited, at a concentration of 0.5 % used for topical application in ophthalmology, Candida spp. to >95 % [75]. Gatifloxacin and sparfloxacin showed activity in a qualitative paper disk diffusion test against Trichophyton rubrum, Fusarium solani, and Candida albicans, but not against Saccharomyces cerevisiae [76]. Ciprofloxacin, moxifloxacin, levofloxacin, trovafloxacin, and sitafloxacin enhanced the activities of antifungal agents against Candida albicans and Aspergillus fumigatus [77–84]. Furthermore, ciprofloxacin showed synergism with azoles against Histoplasma capsulatum and Coccidioides posadasii [85], as well as in combination with amphotericin B against Exophiala spinifera [86].
Several but still rare reports of clinical and microbiological cure of fungal keratitis by quinolones have been published; recently, five additional cases of fungal keratitis treated successfully with topical moxifloxacin monotherapy were published [79]. The causative organisms Curvularia spp., Candida parapsilosis, Paecilomyces lilacinum, and Aspergillus fumigatus were treated with moxifloxacin 0.5 %, one drop every half-hour to every hour. All these cases of fungal keratitis were cured with topical moxifloxacin and the pathogens were eliminated [87].
These data demonstrate that topical administration of quinolones, thus generating high target site concentrations, are clinically effective in the treatment of fungal ophthalmological infections.
Topoisomerase II has been identified as the primary target for quinolones in yeast [88, 89], so that the antifungal activities of the fluoroquinolones tested are likely to be mediated by this enzyme. The DNA topoisomerase II isolated from Candida albicans was more susceptible to quinolones than the calf thymus DNA topoisomerase II, despite the fact that both enzymes are of eukaryotic origin [80]. Yeast DNA topoisomerase II selected for resistance to quinolones are characterized by amino acid mutations which are homologous to mutations in gyrA of Escherichia coli [90–92]. These differences between yeast and mammalian type II topoisomerases may explain why fluoroquinolones exhibit an antifungal activity by maintaining in parallel a selective toxicity against prokaryotic topoisomerases.
Antiparasitic activities of fluoroquinolones
Although antibacterially active fluoroquinolones were derived from the antimalaria agent chloroquine, the clinical efficacy of norfloxacin against Plasmodium falciparum was discovered by chance when the agent was used for the treatment of typhoid fever in Indian patients. Norfloxacin was administered to nine hospitalized malaria patients orally with 400 mg norfloxacin b.i.d. for three days; treatment led to disappearance of splenomegaly [93]. Later, another 15 patients with uncomplicated malaria were treated with norfloxacin (ten with 400 mg b.i.d. and five with 800 mg b.i.d.) for three days [94]. This study confirmed that norfloxacin is clinically effective in the treatment of falciparum malaria, but the efficacy of the lower dose was suboptimal. Later, it was demonstrated that norfloxacin is inferior to chloroquine for falciparum malaria. A prospective, randomized trial revealed that the mean parasite clearance time as well as the mean defervescence time were shorter in the chloroquine group [95].
Fluoroquinolones like ciprofloxacin, amifloxacin, enoxacin, norfloxacin, ofloxacin, pefloxacin, grepafloxacin, trovafloxacin, and 16 additional commercially available quinolones exhibit marked in vitro activity and in vivo efficacy against Plasmodium spp. [96–105].
Nalidixic acid and several fluoroquinolones like ciprofloxacin, norfloxacin, enoxacin, ofloxacin, fleroxacin, clinafloxacin, pefloxacin, and sparfloxacin exerted an antitrypanosomal in vitro and in vivo effect at micromolar concentrations [38, 106–116].
In addition, nalidixic acid, norfloxacin, ofloxacin, moxifloxacin, gatifloxacin, lomefloxacin, and some more fluoroquinolones inhibited growth of the microsporidia Encephalitozoon intestinalis and Vittaforma corneae to 50 % at concentrations ranging from 0.9 to 98.4 μM [112]. Furthermore, ciprofloxacin caused a 50 % growth inhibition of Babesia microti, B. bigemina, B. caballi, B. equi, and B. bovis at concentrations of 2.5 to 15.8 μM [113]. Fluoroquinolones exerted antitoxoplasma activities as well. Moxifloxacin, gatifloxacin, trovafloxacin, and grepafloxacin were the most active agents, inhibiting growth of T. gondii to 50 % at concentrations ranging from 0.4 to 5.1 mg/L, while ciprofloxacin was poorly active, with a 50 % inhibitory concentration value of 79.4 mg/L [116].
The parasites of the phylum Apicomplexa, i.e., Plasmodium spp., Toxoplasma spp., Babesia spp., and Leishmania spp. are characterized by the absence of organelles like mitochondria, but they have acquired a plastid by endosymbiosis of a green alga. The apicoplast is a non-photosynthetic plastid in which several essential biosynthetic pathways are sequestered, so that interactions with these biosynthetic functions cause deleterious effects. Elimination of the plastid or total inhibition of its function results in a “delayed death”, i.e., the parasites grow and evade normally within and from the first host cell, but their replication is halted immediately after the invasion of a new host cell. The apicoplast harbors a circular DNA and bacterial type DNA gyrase. Ciprofloxacin induced cleavage of apicoplast DNA in P. falciparum, without targeting nuclear DNA [117–119]. Exposure of Toxoplasma gondii to ciprofloxacin resulted in a decrease of the apicoplast genome copy number during replication [120]. Although it was discussed that differences in the role of apicoplasts in Toxoplasma and Plasmodium may exist [121], the apicoplast DNA gyrases isolated from both species were inhibited by almost identical concentrations; the apicoplast DNA gyrase isolated from Plasmodium falciparum is inhibited by ciprofloxacin concentrations ranging from 7 to 38 μM and trovafloxacin inhibits apicoplast DNA gyrase activity isolated from Toxoplasma gondii and Plasmodium falciparum, respectively, at 30 μM [102, 117–121]. Consequently, prokaryotic type II DNA topoisomerase of apicomplexan protozoa are effectively targeted by fluoroquinolones.
Indirect effects
It has been summarized previously that fluoroquinolones are active in preclinical infection models against quinolone-resistant bacteria as well as Candida albicans infections [122, 123]. Furthermore, levofloxacin was active against RV infections [74]. These phenomena were found to be directly correlated to the immunomodulatory activities of fluoroquinolones [122, 123]. Mechanisms underlying the various immunomodulatory effects of fluoroquinolones include an effect on intracellular cyclic adenosine-3,5-monophosphate and phosphodiesterases, as well as an effect on transcription factors and also a triggering effect on the eukaryotic equivalent of bacterial SOS response with its ensuing intracellular events [124].
Fluoroquinolones are routinely prescribed for the treatment of coronavirus-associated severe acute respiratory syndrome (SARS) or opportunistic bacterial infections in HIV-positive patients. Upon elimination of the bacterial pathogen or exclusion of bacterial pathogens, antibiotic therapy can be withdrawn. However, patients may benefit from the immunomodulatory activities of fluoroquinolones, but their effect on the course of SARS or acquired immune deficiency syndrome (AIDS) is undetermined.
Although it is well documented that nalidixic acid and fluoroquinolones modulate immune responses by the modulation of intracellular signaling cascades, it is unknown which mechanism(s) may trigger signal transduction. It has been demonstrated that, in analogy to chloroquine, fluoroquinolones bind to and insert into pro- and eukaryotic membranes, respectively, thereby altering their fluidity [116]. Changes in membrane fluidity may be sensed by the immunocompetent cells, so that gene expression may be controlled according to the signals triggered. Furthermore, it can be hypothesized that fluoroquinolones exert direct anti-infective activities due to their physicochemical interactions with membranes, thus making the organisms leaky, followed by cell death. This latter aspect has never been addressed systematically.
Conclusions
Any fluoroquinolone used for the treatment of bacterial infections exerts, in parallel to its antibacterial action, antiviral, antifungal, and antiparasitic actions at clinically achievable concentrations. This broad range of anti-infective activities is due to one common mode of action, i.e., the inhibition of type II topoisomerases, thus maintaining the selective toxicity of fluoroquinolones inhibiting microbial topoisomerases and eukaryotic topoisomerases of prokaryotic origin at low concentrations but mammalian topoisomerases at much higher concentrations. There is strong evidence that the broad range of anti-infective activities translates into the clinical arena. However, anti-infective activities other than antibacterial activities have never been evaluated systematically. This may be due to the strategy of both the pharmaceutical industry and regulatory authorities to develop an agent on the basis of its application, i.e., its use as an antibacterial agent. Therefore, the antiviral or antifungal activities of fluoroquinolones have, so far, not been exploited systematically; two controlled studies evaluating the antiviral effects of fluoroquinolones have been initiated recently. The clinical evaluation of their antifungal and antiparasitic effects is justifiable and would be opportune. Traditionally, clinical studies are designed on the basis of a monocausal microbe–outcome association, i.e., the presence of one bacterial species at the site of infection indicates pathogenicity. Consequently, an anti-infective agent is considered to be effective if this single species is eradicated from the focus of infection. However, infections may be polymicrobial or chronically ill patients may suffer from opportunistic infections; HIV-positive patients represent an extreme example for the acquisition of opportunistic infections caused in parallel by viruses, bacteria, and/or parasites. Such patients could, in theory, benefit from treatment with agents which exert a broad range of anti-infective activities. A multifactorial analysis of the outcome of infectious diseases would be necessary. The corresponding outcome measures are quantifiable and can be linked to pharmacokinetics and overall clinical efficacy. In summary, based on one common mode of action, fluoroquinolones being commercially available as antibacterial agents are active against viruses, fungi, and parasites too, so this class of agents is probably representative of broad-spectrum anti-infectives in its true sense.
References
Lesher GY, Froelich EJ, Gruett MD, Bailey JH, Brundage RP (1962) 1,8-Naphthyridine derivatives. A new class of chemotherapeutic agents. J Med Pharm Chem 5:1063–1065
Slater AF, Cerami A (1992) Inhibition by chloroquine of a novel haem polymerase enzyme activity in malaria trophozoites. Nature 355:167–169
Slater AF (1993) Chloroquine: mechanism of drug action and resistance in Plasmodium falciparum. Pharmacol Ther 57:203–235
Ginsburg H, Famin O, Zhang J, Krugliak M (1998) Inhibition of glutathione-dependent degradation of heme by chloroquine and amodiaquine as a possible basis for their antimalarial mode of action. Biochem Pharmacol 56:1305–1313
Savarino A, Gennero L, Sperber K, Boelaert JR (2001) The anti-HIV-1 activity of chloroquine. J Clin Virol 20:131–135
Savarino A, Gennero L, Chen HC, Serrano D, Malavasi F, Boelaert JR, Sperber K (2001) Anti-HIV effects of chloroquine: mechanisms of inhibition and spectrum of activity. AIDS 15:2221–2229
Savarino A, Boelaert JR, Cassone A, Majori G, Cauda R (2003) Effects of chloroquine on viral infections: an old drug against today’s diseases? Lancet Infect Dis 3:722–727
Savarino A, Di Trani L, Donatelli I, Cauda R, Cassone A (2006) New insights into the antiviral effects of chloroquine. Lancet Infect Dis 6:67–69
Vincent MJ, Bergeron E, Benjannet S, Erickson BR, Rollin PE, Ksiazek TG, Seidah NG, Nichol ST (2005) Chloroquine is a potent inhibitor of SARS coronavirus infection and spread. Virol J 2:69. doi:10.1186/1743-422X-2-69
Di Trani L, Savarino A, Campitelli L, Norelli S, Puzelli S, D’Ostilio D, Vignolo E, Donatelli I, Cassone A (2007) Different pH requirements are associated with divergent inhibitory effects of chloroquine on human and avian influenza A viruses. Virol J 4:39. doi:10.1186/1743-422X-4-39
Naarding MA, Baan E, Pollakis G, Paxton WA (2007) Effect of chloroquine on reducing HIV-1 replication in vitro and the DC-SIGN mediated transfer of virus to CD4+ T-lymphocytes. Retrovirology 4:6. doi:10.1186/1742-4690-4-6
Keyaerts E, Li S, Vijgen L, Rysman E, Verbeeck J, Van Ranst M, Maes P (2009) Antiviral activity of chloroquine against human coronavirus OC43 infection in newborn mice. Antimicrob Agents Chemother 53:3416–3421
Rolain JM, Colson P, Raoult D (2007) Recycling of chloroquine and its hydroxyl analogue to face bacterial, fungal and viral infections in the 21st century. Int J Antimicrob Agents 30:297–308
Harrison TS, Griffin GE, Levitz SM (2000) Conditional lethality of the diprotic weak bases chloroquine and quinacrine against Cryptococcus neoformans. J Infect Dis 182:283–289
Khan MA, Jabeen R, Nasti TH, Mohammad O (2005) Enhanced anticryptococcal activity of chloroquine in phosphatidylserine-containing liposomes in a murine model. J Antimicrob Chemother 55:223–228
Doi S, Tanabe K, Watanabe M, Yoshimura M (1988) Chloroquine, a lysosomotropic agent, inhibits zygote formation in yeast. Arch Microbiol 151:20–25
Ciak J, Hahn FE (1966) Chloroquine: mode of action. Science 151:347–349
Acheampong YB (1988) Kinetics of bacteriostatic activity of chloroquine on Staphylococcus aureus. Indian J Pharm Sci 50:40–42
Smith KT, Dawes IW (1989) The preferential inhibition of Bacillus subtilis spore outgrowth by chloroquine. Arch Microbiol 152:251–257
Wolf R, Baroni A, Greco R, Donnarumma G, Ruocco E, Tufano MA, Ruocco V (2002) Quinine sulfate and bacterial invasion. Ann Clin Microbiol Antimicrob 1:5
Ramos-Avila A, Ventura-Gallegos JL, Zentella-Dehesa A, Machuca-Rodríguez C, Moreno-Altamirano MM, Narváez V, Legorreta-Herrera M (2007) Immunomodulatory role of chloroquine and pyrimethamine in Plasmodium yoelii 17XL infected mice. Scand J Immunol 65:54–62
Schultz KR, Gilman AL (1997) The lysosomotropic amines, chloroquine and hydroxychloroquine: a potentially novel therapy for graft-versus-host disease. Leuk Lymphoma 24:201–210
Cooper RG, Magwere T (2008) Chloroquine: novel uses & manifestations. Indian J Med Res 127:305–316
Yi AK, Peckham DW, Ashman RF, Krieg AM (1999) CpG DNA rescues B cells from apoptosis by activating NFkappaB and preventing mitochondrial membrane potential disruption via a chloroquine-sensitive pathway. Int Immunol 11:2015–2024
Thomé R, Moraes AS, Bombeiro AL, dos Santos Farias A, Francelin C, da Costa TA, Di Gangi R, Barbosa dos Santos LM, Rodrigues de Oliveira AL, Verinaud L (2013) Chloroquine treatment enhances regulatory T cells and reduces the severity of experimental autoimmune encephalomyelitis. PLoS One 8(6):e65913. doi:10.1371/journal.pone.0065913
Vezmar M, Georges E (2000) Reversal of MRP-mediated doxorubicin resistance with quinoline-based drugs. Biochem Pharmacol 59:1245–1252
Zamora JM, Pearce HL, Beck WT (1988) Physical-chemical properties shared by compounds that modulate multidrug resistance in human leukemic cells. Mol Pharmacol 33:454–462
Klohs WD, Steinkampf RW (1988) The effect of lysosomotropic agents and secretory inhibitors on anthracycline retention and activity in multiple drug-resistant cells. Mol Pharmacol 34:180–185
Lee CM, Tannock IF (2006) Inhibition of endosomal sequestration of basic anticancer drugs: Influence on cytotoxicity and tissue penetration. Br J Cancer 94:863–869
Zhao H, Cai Y, Santi S, Lafrenie R, Lee H (2005) Chloroquine-mediated radiosensitization is due to the destabilization of the lysosomal membrane and subsequent induction of cell death by necrosis. Radiat Res 164:250–257
Jensen PB, Sørensen BS, Sehested M, Grue P, Demant EJ, Hansen HH (1994) Targeting the cytotoxicity of topoisomerase II-directed epipodophyllotoxins to tumor cells in acidic environments. Cancer Res 54:2959–2963
Langer SW, Schmidt G, Sørensen M, Sehested M, Jensen PB (1999) Inhibitors of topoisomerase II as pH-dependent modulators of etoposide-mediated cytotoxicity. Clin Cancer Res 5:2899–2907
Schneider YJ, Trouet A (1981) Effect of chloroquine and methylamine on endocytosis of fluorescein-labelled controlled IgG and of anti-(plasma membrane) IgG by cultured fibroblasts. Eur J Biochem 118:33–38
Pecivová J, Drábiková K, Nosál R (1994) Effect of chloroquine on mast cell membranes. Agents Actions 41(Suppl):C43–C44
Chesney RW, Budreau AM (1995) Chloroquine, a novel inhibitor of amino acid transport by rat renal brush border membrane vesicles. Amino Acids 8:141–158
Rodríguez-Menchaca AA, Navarro-Polanco RA, Ferrer-Villada T, Rupp J, Sachse FB, Tristani-Firouzi M, Sánchez-Chapula JA (2008) The molecular basis of chloroquine block of the inward rectifier Kir2.1 channel. Proc Natl Acad Sci U S A 105:1364–1368
Noujaim SF, Stuckey JA, Ponce-Balbuena D, Ferrer-Villada T, López-Izquierdo A, Pandit SV, Sánchez-Chapula JA, Jalife J (2011) Structural bases for the different anti-fibrillatory effects of chloroquine and quinidine. Cardiovasc Res 89:862–869
Betbeder D, Hutchison DW, Baltz T, Cros S (1988) Trypanocidal and antitumor activities of nalidixic and oxolinic acid derivatives. Med Sci Res 16:141–142
Furet YX, Pechère JC (1991) Newly documented antimicrobial activity of quinolones. Eur J Clin Microbiol Infect Dis 10:249–254
Segev S, Rubinstein E (1998) Future aspects. In: Kuhlmann J, Dalhoff A, Zeiler H-J (eds) Handbook of experimental pharmacology, vol. 127: quinolone antibacterials. Springer-Verlag, Berlin, Heidelberg, New York, pp 455–477
Eliopoulos GM, Eliopoulos CT (1993) Activity in vitro of the quinolones. In: Hooper DC, Wolfson JS (eds) Quinolone antimicrobial agents, 2nd edn. ASM Press, Washington, DC, pp 161–193
Shen LL (1993) Quinolone–DNA interaction. In: Hooper DC, Wolfson JS (eds) Quinolone antimicrobial agents, 2nd edn. ASM Press, Washington, DC, pp 77–95
Palù G, Valisena S, Peracchi M, Palumbo M (1988) Do quinolones bind to DNA? Biochem Pharmacol 37:1887–1888
Shen LL (1989) A reply: “Do quinolones bind to DNA?”—Yes. Biochem Pharmacol 38:2042–2044
Laponogov I, Sohi MK, Veselkov DA, Pan XS, Sawhney R, Thompson AW, McAuley KE, Fisher LM, Sanderson MR (2009) Structural insight into the quinolone–DNA cleavage complex of type IIA topoisomerases. Nat Struct Mol Biol 16:667–669
Wohlkonig A, Chan PF, Fosberry AP, Homes P, Huang J, Kranz M, Leydon VR, Miles TJ, Pearson ND, Perera RL, Shillings AJ, Gwynn MN, Bax BD (2010) Structural basis of quinolone inhibition of type IIA topoisomerases and target-mediated resistance. Nat Struct Mol Biol 17:1152–1153
Hamilton-Miller JMT (1999) beta-lactams: variations on a chemical theme, with some surprising biological results. J Antimicrob Chemother 44:729–734
Dalhoff A (1987) Pleiotropic actions of aminoglycosides.In: Döring G, Holder IA, Botzenhart K (eds) Antibiotics and chemotherapy. Basic research and clinical aspects of Pseudomonas aeruginosa. Karger, Basel, pp 182–204
Champoux JJ (2001) DNA topoisomerases: structure, function, and mechanism. Annu Rev Biochem 70:369–413
Corbett KD, Berger JM (2004) Structure, molecular mechanisms, and evolutionary relationships in DNA topoisomerases. Annu Rev Biophys Biomol Struct 33:95–118
Pommier Y, Leo E, Zhang HL, Marchand C (2010) DNA topoisomerases and their poisoning by anticancer and antibacterial drugs. Chem Biol 17:421–433
Forterre P, Gadelle D (2009) Phylogenomics of DNA topoisomerases: their origin and putative roles in the emergence of modern organisms. Nucleic Acids Res 37:679–692. doi:10.1093/nar/gkp032
Chen SH, Chan NL, Hsieh TS (2013) New mechanistic and functional insights into DNA topoisomerases. Annu Rev Biochem 82:139–170
Takada A, Takase S, Tsutsumi M, Sawada M (1993) Effects of ofloxacin for type C hepatitis. Int Hepatol Commun 1:272–277
Kojima H, Kaita KDE, Hawkins K, Uhanova J, Minuk GY (2002) Use of fluoroquinolones in patients with chronic hepatitis C virus-induced liver failure. Antimicrob Agents Chemother 46:3280–3282
Leung AY, Chan MT, Yuen KY, Cheng VC, Chan KH, Wong CL, Liang R, Lie AK, Kwong YL (2005) Ciprofloxacin decreased polyoma BK virus load in patients who underwent allogeneic hematopoietic stem cell transplantation. Clin Infect Dis 40:528–537
Chandraker A, Ali S, Drachenberg CB, Wali R, Hirsch H, DeCaprio J, Ramos E (2004) Use of fluoroquinolones to treat BK infection in renal transplant recipients [Abstract]. Am J Transplant 4:587
Gabardi S, Waikar SS, Martin S, Roberts K, Chen J, Borgi L, Sheashaa H, Dyer C, Malek SK, Tullius SG, Vadivel N, Grafals M, Abdi R, Najafian N, Milford E, Chandraker A (2010) Evaluation of fluoroquinolones for the prevention of BK viremia after renal transplantation. Clin J Am Soc Nephrol 5:1298–1304
Arroyo D, Chandran S, Vagefi PA, Wojciechowski D (2014) Adjuvant ciprofloxacin for persistent BK polyomavirus infection in kidney transplant recipients. J Transplant 2014:107459. doi:10.1155/2014/107459
Sharma BN, Li R, Bernhoff E, Gutteberg TJ, Rinaldo CH (2011) Fluoroquinolones inhibit human polyomavirus BK (BKV) replication in primary human kidney cells. Antiviral Res 92:115–123
Randhawa PS (2005) Anti-BK virus activity of ciprofloxacin and related antibiotics. Clin Infect Dis 41:1366–1367
Ali S, Chandraker A, DeCaprio J (2003) Inhibition of polyoma helicase activity by quinolones. J Am Soc Nephrol 14:43A
Ali SH, Chandraker A, DeCaprio J (2007) Inhibition of simian virus 40 large T antigen helicase activity by fluoroquinolones. Antivir Ther 12:1–6
Khan IA, Siddiqui S, Rehmani S, Kazmi SU, Ali SH (2012) Fluoroquinolones inhibit HCV by targeting its helicase. Antivir Ther 17:467–476
Umbro I, Anzivino E, Tinti F, Zavatto A, Bellizzi A, Rodio DM, Mancini C, Pietropaolo V, Mitterhofer AP (2013) Possible antiviral effect of ciprofloxacin treatment on polyomavirus BK replication and analysis of non-coding control region sequences. Virol J 10:274
Humar A, Gill J, Johnston O, Fergusson D, House AA, Lebel L, Cockfield S, Kim SJ, Zaltzman J, Cantarovich M, Karpinski M, Ramsay T, Knoll GA (2013) Quinolone prophylaxis for the prevention of BK virus infection in kidney transplantation: study protocol for a randomized controlled trial. Trials 14:185
Patel SJ (2014) Ciprofloxacin for prevention of BK infection. ClinicalTrials.gov identifier: NCT01789203, last updated June 24, 2014, last visited October 8, 2014
Ikeda S, Yazawa M, Nishimura C (1987) Antiviral activity and inhibition of topoisomerase by ofloxacin, a new quinolone derivative. Antiviral Res 8:103–113
Kamau E, Grove A (2004) Fluoroquinolone-dependent DNA supercoiling by vaccinia topoisomerase I. J Mol Biol 342:479–487
Pessina A, Mineo E, Gribaldo L, Neri MG (1992) Lack of in vitro antiviral activity of fluoroquinolones against herpes simplex virus type 2. Arch Virol 122:263–269
Gurtler L, Eberle J, Deinhardt F (1989) Inhibition of HIV reverse transcriptase by 4-quinolones. In: Proceedings of the 5th International Conference on AIDS, Montreal, Canada, June 1989, abstract no. C624
Grohe K, Dummer W, Rossen K, Paessens A (1991) Quinolone carboxylic acid derivatives, process for their preparation and their use. Patent number 0422485 A2
Grohe K, Dummer W, Rossen K, Paessens A (1993) Quinolone carboxylic acid derivatives and their use as antiviral agents. Patent number US5217972 A
Yamaya M, Nishimura H, Hatachi Y, Yasuda H, Deng X, Sasaki T, Mizuta K, Kubo H, Nagatomi R (2012) Levofloxacin inhibits rhinovirus infection in primary cultures of human tracheal epithelial cells. Antimicrob Agents Chemother 56:4052–4061
Ozdek SC, Miller D, Flynn PM, Flynn HW (2006) In vitro antifungal activity of the fourth generation fluoroquinolones against Candida isolates from human ocular infections. Ocul Immunol Inflamm 14:347–351
Sultana N, Naz A, Khan B, Arayne MS, Mesiak MA (2010) Synthesis, characterization, antibacterial, antifungal, and immunomodulating activities of gatifloxacin derivatives. Med Chem Res 19:1210–1221
Stergiopoulou T, Meletiadis J, Sein T, Papaioannidou P, Tsiouris I, Roilides E, Walsh TJ (2009) Comparative pharmacodynamic interaction analysis between ciprofloxacin, moxifloxacin and levofloxacin and antifungal agents against Candida albicans and Aspergillus fumigatus. J Antimicrob Chemother 63:343–348
Stergiopoulou T, Meletiadis J, Sein T, Papaioannidou P, Tsiouris I, Roilides E, Walsh TJ (2008) Isobolographic analysis of pharmacodynamic interactions between antifungal agents and ciprofloxacin against Candida albicans and Aspergillus fumigatus. Antimicrob Agents Chemother 52:2196–2204
Stergiopoulou T, Meletiadis J, Sein T, Papaioannidou P, Walsh TJ, Roilides E (2011) Synergistic interaction of the triple combination of amphotericin B, ciprofloxacin, and polymorphonuclear neutrophils against Aspergillus fumigatus. Antimicrob Agents Chemother 55:5923–5929
Sugar AM, Liu XP, Chen RJ (1997) Effectiveness of quinolone antibiotics in modulating the effects of antifungal drugs. Antimicrob Agents Chemother 41:2518–2521
Petrou MA, Rogers TR (1988) In-vitro activity of antifungal agents in combination with four quinolones. Drugs Exp Clin Res 14:9–18
Deren YT, Özdek S, Kalkanci A, Akyürek N, Hasanreisoğlu B (2010) Comparison of antifungal efficacies of moxifloxacin, liposomal amphotericin B, and combination treatment in experimental Candida albicans endophthalmitis in rabbits. Can J Microbiol 56:1–7
Yalçin B, Kalkanci A, Gürelik F, Fidan I, Kustimur S, Ozdek S (2010) In vitro synergistic effect of moxifloxacin and amphotericin B combination against Candida strains. Mikrobiyol Bul 44:65–70
Nakajima R, Kitamura A, Someya K, Tanaka M, Sato K (1995) In vitro and in vivo antifungal activities of DU-6859a, a fluoroquinolone, in combination with amphotericin B and fluconazole against pathogenic fungi. Antimicrob Agents Chemother 39:1517–1521
Brilhante RSN, Caetano EP, Sidrim JJ, Cordeiro RA, Camargo ZP, Fechine MAB, Lima RAC, Castelo Branco DSCM, Marques FJF, Mesquita JRL, Lima DT, Monteiro AJ, Rocha MFG (2013) Ciprofloxacin shows synergism with classical antifungals against Histoplasma capsulatum var. capsulatum and Coccidioides posadasii. Mycoses 56:397–401
Vitale RG, Afeltra J, de Hoog GS, Rijs AJ, Verweij PE (2003) In vitro activity of amphotericin B and itraconazole in combination with flucytosine, sulfadiazine and quinolones against Exophiala spinifera. J Antimicrob Chemother 51:1297–1300
Matoba AY (2012) Fungal keratitis responsive to moxifloxacin monotherapy. Cornea 31:1206–1209
Shen LL, Baranowski J, Fostel J, Montgomery DA, Lartey PA (1992) DNA topoisomerases from pathogenic fungi: targets for the discovery of antifungal drugs. Antimicrob Agents Chemother 36:2778–2784
Elsea SH, Osheroff N, Nitiss JL (1992) Cytotoxicity of quinolones toward eukaryotic cells. Identification of topoisomerase II as the primary cellular target for the quinolone CP-115,953 in yeast. J Biol Chem 267:13150–13153
Hsiung Y, Elsea SH, Osheroff N, Nitiss JL (1995) A mutation in yeast TOP2 homologous to a quinolone-resistant mutation in bacteria. Mutation of the amino acid homologous to Ser83 of Escherichia coli gyrA alters sensitivity to eukaryotic topoisomerase inhibitors. J Biol Chem 270:20359–20364
Strumberg D, Nitiss JL, Rose A, Nicklaus MC, Pommier Y (1999) Mutation of a conserved serine residue in a quinolone-resistant type II topoisomerase alters the enzyme–DNA and drug interactions. J Biol Chem 274:7292–7301
Dong J, Walker J, Nitiss JL (2000) A mutation in yeast topoisomerase II that confers hypersensitivity to multiple classes of topoisomerase II poisons. J Biol Chem 275:7980–7987
Sarma PS (1989) Norfloxacin: a new drug in the treatment of falciparum malaria. Ann Intern Med 111:336–337
Tripathi KD, Sharma AK, Valecha N, Kulpati DD (1993) Curative efficacy of norfloxacin in falciparum malaria. Indian J Med Res 97:176–178
McClean KL, Hitchman D, Shafran SD (1992) Norfloxacin is inferior to chloroquine for falciparum malaria in northwestern Zambia: a comparative clinical trial. J Infect Dis 165:904–907
Hamzah J, Skinner-Adams T, Davis TME (2000) In vitro antimalarial activity of trovafloxacin, a fourth-generation fluoroquinolone. Acta Trop 74:39–42
Yeo AET, Rieckmann KH (1994) Prolonged exposure of Plasmodium falciparum to ciprofloxacin increases anti-malarial activity. J Parasitol 80:158–160
Bryskier A, Labro MT (1990) Quinolones and malaria: an avenue for the future. Quinolones Bull 6:1–4
Divo AA, Sartorelli AC, Patton CL, Bia FJ (1988) Activity of fluoroquinolone antibiotics against Plasmodium falciparum in vitro. Antimicrob Agents Chemother 32:1182–1186
Mahmoudi N, Ciceron L, Franetich JF, Farhati K, Silvie O, Eling W, Sauerwein R, Danis M, Mazier D, Derouin F (2003) In vitro activities of 25 quinolones and fluoroquinolones against liver and blood stage Plasmodium spp.. Antimicrob Agents Chemother 47:2636–2639
Watt G, Shanks GD, Edstein MD, Pavanand K, Webster HK, Wechgritaya S (1991) Ciprofloxacin treatment of drug-resistant falciparum malaria. J Infect Dis 164:602–604
Salmon D, Deloron P, Gaudin C, Malhotra K, Lebras J, Pocidalo JJ (1990) Activities of pefloxacin and ciprofloxacin against experimental malaria in mice. Antimicrob Agents Chemother 34:2327–2330
Keiser J, Burri C (2001) Evaluation of quinolone derivatives for antitrypanosomal activity. Trop Med Int Health 6:369–389
Nenortas E, Burri C, Shapiro TA (1999) Antitrypanosomal activity of fluoroquinolones. Antimicrob Agents Chemother 43:2066–2068
Nenortas E, Kulikowicz T, Burri C, Shapiro TA (2003) Antitrypanosomal activities of fluoroquinolones with pyrrolidinyl substitutions. Antimicrob Agents Chemother 47:3015–3017
Gonzales-Perdomo M, de Castro SL, Meirelles MN, Goldenberg S (1990) Trypanosoma cruzi proliferation and differentiation are blocked by topoisomerase II inhibitors. Antimicrob Agents Chemother 34:1707–1714
Croft SL, Hogg J (1988) Limited activity of bacterial DNA topoisomerase II inhibitors against Leishmania donovani and Trypanosoma cruzi amastigotes in vitro. Trans R Soc Trop Med Hyg 82:856
Raether W, Seidenath H, Hofmann J (1989) Potent antibacterial fluoroquinolones with marked activity against Leishmania donovani in vivo. Parasitol Res 75:412–413
Sanguigni S, Marangi M, Gramiccia M, Orsini S, Paparo BS, Nicodemo G, Gradoni L (1993) Ciprofloxacin in the treatment of leishmaniasis. G Mal Infett Parassit 45:447–449
Savoia D, Biglino S, Cestaro A, Zucca M (1993) In vitro and in vivo activity of some fluoroquinolones on two Leishmania species. Eur Bull Drug Res 2:135–138
Romero IC, Saravia NG, Walker J (2005) Selective action of fluoroquinolones against intracellular amastigotes of Leishmania (Viannia) panamensis in vitro. J Parasitol 91:1474–1479
Didier ES, Bowers L, Stovall ME, Kuebler D, Mittleider D, Brindley PJ, Didier PJ (2005) Antimicrosporidial activity of (fluoro)quinolones in vitro and in vivo. Folia Parasitol (Praha) 52:173–181
Aboulaila M, Munkhjargal T, Sivakumar T, Ueno A, Nakano Y, Yokoyama M, Yoshinari T, Nagano D, Katayama K, El-Bahy N, Yokoyama N, Igarashi I (2012) Apicoplast-targeting antibacterials inhibit the growth of Babesia parasites. Antimicrob Agents Chemother 56:3196–3206
Khan AA, Slifer T, Araujo FG, Remington JS (1996) Trovafloxacin is active against Toxoplasma gondii. Antimicrob Agents Chemother 40:1855–1859
Khan AA, Araujo FG, Brighty KE, Gootz TD, Remington JS (1999) Anti-Toxoplasma gondii activities and structure–activity relationships of novel fluoroquinolones related to trovafloxacin. Antimicrob Agents Chemother 43:1783–1787
Gozalbes R, Brun-Pascaud M, Garcia-Domenech R, Galvez J, Girard PM, Doucet JP, Derouin F (2000) Anti-toxoplasma activities of 24 quinolones and fluoroquinolones in vitro: prediction of activity by molecular topology and virtual computational techniques. Antimicrob Agents Chemother 44:2771–2776
Chavalitshewinkoon-Petmitr P, Worasing R, Wilairat P (2001) Partial purification of mitochondrial DNA topoisomerase II from Plasmodium falciparum and its sensitivity to inhibitors. Southeast Asian J Trop Med Public Health 32:733–738
Weissig V, Vetro-Widenhouse TS, Rowe TC (1997) Topoisomerase II inhibitors induce cleavage of nuclear and 35-kb plastid DNAs in the malarial parasite Plasmodium falciparum. DNA Cell Biol 16:1483–1492
Prusty D, Dar A, Priya R, Sharma A, Dana S, Choudhury NR, Rao NS, Dhar SK (2010) Single-stranded DNA binding protein from human malarial parasite Plasmodium falciparum is encoded in the nucleus and targeted to the apicoplast. Nucleic Acids Res 38:7037–7053
Fichera ME, Roos DS (1997) A plastid organelle as a drug target in apicomplexan parasites. Nature 390:407–409
Goodman CD, Su V, McFadden GI (2007) The effects of anti-bacterials on the malaria parasite Plasmodium falciparum. Mol Biochem Parasitol 152:181–191
Dalhoff A (2005) Immunomodulatory activities of fluoroquinolones. Infection 33(Suppl 2):55–70
Dalhoff A, Shalit I (2003) Immunomodulatory effects of quinolones. Lancet Infect Dis 3:359–371
Dalhoff A, Döring G (1987) Action of quinolones on gene expression and bacterial membranes. In: Döring G, Holder IA, Botzenhart K (eds) Antibiotics and chemotherapy. Basic research and clinical aspects of Pseudomonas aeruginosa. Karger, Basel, Switzerland, pp 205–214
Conflict of interest
The author declares that he has no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Dalhoff, A. Antiviral, antifungal, and antiparasitic activities of fluoroquinolones optimized for treatment of bacterial infections: a puzzling paradox or a logical consequence of their mode of action?. Eur J Clin Microbiol Infect Dis 34, 661–668 (2015). https://doi.org/10.1007/s10096-014-2296-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10096-014-2296-3