Abstract
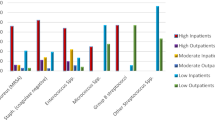
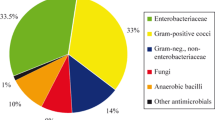
Diabetes mellitus (DM) is one of the most common diseases worldwide, and is a significant risk factor for healthcare-associated infections (HAIs). Our aim in this study was to compare the distributions of HAIs and the causative pathogens between diabetic and non-diabetic patients. In this study, 716 HAIs in 465 diabetic patients and 761 HAIs in 465 non-diabetic patients were evaluated. HAIs in patients with DM were most frequently urinary tract infections (UTIs) [266 infections (37.2 %)], followed by blood stream infections (BSIs) [161 infections (22.5 %)], surgical site infections (SSIs) [127 infections (17.7 %)], pneumonia [107 infections (14.9 %)] and any other infections [161 infections (22.5 %)]. The rates of UTIs, BSIs, SSIs, pneumonia and any other infections were similar between diabetic and non-diabetic patients. In terms of the causative pathogens, Staphylococcus aureus more frequently caused SSIs and Candida spp more frequently caused UTIs in diabetic patients compared with non-diabetic patients. We found no differences in the distribution of HAIs between patients without and with DM. However, S. aureus and Candida spp were more common causative pathogens of SSIs and URTIs, respectively, in diabetic patients than in non-diabetic patients.
Similar content being viewed by others
References
Delamaire M, Maugendre D, Moreno M, Le Goff MC, Allannic H, Genetet B (1997) Impaired leucocyte functions in diabetic patients. Diabet Med 14:29–34
Joshi N, Caputo GM, Weitekamp MR, Karchmer AW (1999) Infections in patients with diabetes mellitus. N Engl J Med 341:1906–1912
Al-Asmary SM, Al-Helali NS, Abdel-Fattah MM, Al-Jabban TM, Al-Bamri AM (2004) Nosocomial urinary tract infection. Risk factors, rates and trends. Saudi Med J 25:895–900
Platt R, Polk BF, Murdock B, Rosner B (1986) Risk factors for nosocomial urinary tract infection. Am J Epidemiol 124:977–985
Drapeau CM, D’Aniello C, Brafa A, Nicastri E, Silvestri A, Nisi G, Petrosillo N (2007) Surgical site infections in plastic surgery: an Italian multicenter study. J Surg Res 143:393–397
Cheadle WG (2006) Risk factors for surgical site infection. Surg Infect 7(Suppl 1):7–11
Erman T, Demirhindi H, Gocer AI, Tuna M, Ildan F, Boyar B (2005) Risk factors for surgical site infections in neurosurgery patients with antibiotic prophylaxis. Surg Neurol 63:107–112
Vilar-Compte D, Mohar A, Sandoval S, de la Rosa M, Gordillo P, Volkow P (2000) Surgical site infections at the National Cancer Institute in Mexico: a case-control study. Am J Infect Control 28:14–20
Vuorisalo S, Haukipuro K, Pokela R, Syrjala H (1998) Risk features for surgical-site infections in coronary artery bypass surgery. Infect Control Hosp Epidemiol 19:240–247
Vardakas KZ, Siempos II, Falagas ME (2007) Diabetes mellitus as a risk factor for nosocomial pneumonia and associated mortality. Diabet Med 24:1168–1171
Harris MI, Hadden WC, Knowler WC, Bennett PH (1987) Prevalence of diabetes and impaired glucose tolerance and plasma glucose levels in U.S. population aged 20–74 year. Diabetes 36:523–534
Masoodi SR, Wani AI, Misgar RA, Gupta VK, Bashir MI, Zargar AH (2007) Pattern of infections in patients with diabetes mellitus: data from a tertiary care medical centre in Indian sub-continent. Diabetes Metab Syndr: Clini Res Rev 1:91–95
Meiland R, Geerlings SE, Hoepelman AI (2002) Management of bacterial urinary tract infections in adult patients with diabetes mellitus. Drugs 62:1859–1868
Ronald A, Ludwig E (2001) Urinary tract infections in adults with diabetes. Int J Antimicrob Agents 17:287–292
Gorter KJ, Hak E, Zuithoff NP, Hoepelman AI, Rutten GE (2010) Risk of recurrent acute lower urinary tract infections and prescription pattern of antibiotics in women with and without diabetes in primary care. Fam Pract 27(4):379–385
Czaja CA, Rutledge BN, Cleary PA, Chan K, Stapleton AE, Stamm WE (2009) Urinary tract infections in women with type 1 diabetes mellitus: survey of female participants in the epidemiology of diabetes interventions and complications study cohort. J Urol 181(3):1129–1134
Geerlings SE, Stolk RP, Camps MJ, Netten PM, Hoekstra JB, Bouter KP, Bravenboer B, Collet JT, Jansz AR, Hoepelman AI (2000) Asymptomatic bacteriuria may be considered a complication in women with diabetes. Diabetes Mellitus Women Asymptomatic Bacteriuria Utrecht Study Group. Diabetes Care 23:744–749
Hoepelman AI, Meiland R, Geerlings SE (2003) Pathogenesis and management of bacterial urinary tract infections in adult patients with diabetes mellitus. Int J Antimicrob Agents 22(Suppl 2):35–43
Rassias AJ, Givan AL, Marrin CA, Whalen K, Pahl J, Yeager MP (2002) Insulin increases neutrophil count and phagocytic capacity after cardiac surgery. Anesth Analg 94:1113–1119
King JT Jr, Goulet JL, Perkal MF, Rosenthal RA (2011) Glycemic control and infections in patients with diabetes undergoing noncardiac surgery. Ann Surg 253(1):158–165
Horcajada JP, Moreno I, Velasco M, Martínez JA, Moreno-Martínez A, Barranco M, Vila J, Mensa J (2003) Community-acquired febrile urinary tract infection in diabetics could deserve a different management: a case-control study. J Intern Med 254:280–286
Guler S, Ural O, Findik D, Arslan U (2006) Risk factors for nosocomial candiduria. Saudi Med J 27:1706–1710
Alvarez-Lerma F, Nolla-Salas J, León C, Palomar M, Jordá R, Carrasco N, Bobillo F (2003) Candiduria in critically ill patients admitted to intensive care medical units. Intensive Care Med 29:1069–1076
Colodner R, Nuri Y, Chazan B, Raz R (2008) Community-acquired and hospital-acquired candiduria: comparison of prevalence and clinical characteristics. Eur J Clin Microbiol Infect Dis 27:301–305
Calvet HM, Yoshikawa TT (2001) Infections in diabetes. Infect Dis Clin North Am 15:407–421
Anderson DJ, Chen LF, Schmader KE, Sexton DJ, Choi Y, Link K, Sloane R, Kaye KS (2008) Poor functional status as a risk factor for surgical site infection due to methicillin-resistant Staphylococcus aureus. Infect Control Hosp Epidemiol 29(9):832–839
Lipsky BA, Tabak YP, Johannes RS, Vo L, Hyde L, Weigelt JA (2010) Skin and soft tissue infections in hospitalised patients with diabetes: culture isolates and risk factors associated with mortality, length of stay and cost. Diabetologia 53(5):914–923
Muñoz P, Hortal J, Giannella M, Barrio JM, Rodríguez-Créixems M, Pérez MJ, Rincón C, Bouza E (2008) Nasal carriage of S. aureus increases the risk of surgical site infection after major heart surgery. J Hosp Infect 68:25–31
Author information
Authors and Affiliations
Corresponding author
Additional information
Some results of this study were presented at the Sixth Congress of the International Federation of Infection Control, İstanbul, Turkey, October 13–16, 2005.
Rights and permissions
About this article
Cite this article
Erben, N., Ozgunes, I., Aksit, F. et al. Healthcare-associated infections and the distribution of causative pathogens in patients with diabetes mellitus. Eur J Clin Microbiol Infect Dis 32, 821–825 (2013). https://doi.org/10.1007/s10096-013-1816-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10096-013-1816-x