Abstract
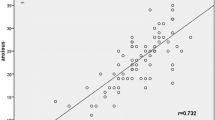
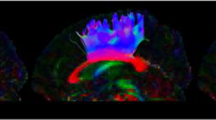
The aim of this study was to explore the relationship between abnormality on susceptibility-weighted imaging (SWI) and newly-developed depression after mild traumatic brain injury. The study registered 200 patients with closed TBI and normal finding at CT and conventional MRI. All patients underwent MRI including conventional MR sequences and SWI. The number and volume of microbleed lesions were semi-automatically outlined and manually counted. All patients were followed up with the Structured Clinical Interview for DSM-IV Axis I Disorders (SCID-IV) within 1 year after TBI. The difference in microbleed lesions on SWI was compared between the depressive and non-depressive groups. The depressive group had a higher rate of abnormality on SWI than did the non-depressive group (p < 0.001). Among patients that had exhibited microbleed lesions, the number and volume of lesions were greater in the depressive group than the non-depressive group (both p < 0.001). These differences in numbers and volume of lesions were found only at the frontal, parietal and temporal lobes (all p < 0.001). Among patients that had exhibited microbleed lesions, the number and volume of lesions in other areas were not significantly different between the depressive and non-depressive groups (all p > 0.05). In conclusion, SWI was useful to identify the microbleed lesions after mild TBI. The distribution range and location of microbleed lesions were correlated with depression after TBI.




Similar content being viewed by others
References
Freire MA (2012) Pathophysiology of neurodegeneration following traumatic brain injury. West Indian Med J 61:751–755
Ponsford J, Sloan S, Snow P (1995) Traumatic brain injury: rehabilitation for everyday adaptive living. Lawrence Erlbaum Associates, Hove
Rao V, Munro CA, Rosenberg P, Ward J, Bertrand M, Degoankar M et al (2010) Neuroanatomical correlates of depression in post traumatic brain injury: preliminary results of a pilot study. J Neuropsychiatry Clin Neurosci 22:231–235
Kraus MF, Susmaras T, Caughlin BP, Walker CJ, Sweeney JA, Little DM (2007) White matter integrity and cognition in chronic traumatic brain injury: a diffusion tensor imaging study. Brain 130:2508–2519
Levin HS, McCauley SR, Josic CP, Boake C, Brown SA, Goodman HS et al (2005) Predicting depression following mild Traumatic brain injury. Arch Gen Psychiatry 62:523–528
Wood RL (2004) Understanding the ‘miserable minority’: a diathesis-stress paradigm for post-concussional syndrome. Brain Inj 18:1135–1153
Carroll L, Cassidy JD, Holm L, Kraus J, Coronado VG, WHO Collaborating Centre Task Force on Mild Traumatic Brain Injury (2004) Methodological issues and research recommendations for mild traumatic brain injury: the WHO Collaborating Centre Task Force on mild traumatic brain injury. J Rehabil Med 43(Suppl):113–125
Bazarian J, McClung J, Shah MN, Cheng YT, Flesher W, Kraus J (2004) Mild traumatic brain injury in the US, 1998–2000. Brain Inj 19:85–91
Mooney G, Speed J (2001) The association between mild traumatic brain injury and psychiatric conditions. Brain Inj 15:865–877
First MB, Spitzer RL, Gibbon M, Williams JBW (2002) Structured clinical interview for DSM-IV-TR axis I disorders, research version, patient edition. Biometrics Research, New York State Psychiatric Institute, New York
Bombardier CH, Fann JR, Temkin NR, Esselman PC, Barber J, Dikmen SS (2010) Rates of major depressive disorder and clinical outcomes following traumatic brain injury. JAMA 303:1938–1945
Jorge RE, Starkstein SE, Arndt S, Moser D, Crespo-Facorro B, Robinson RG (2005) Alcohol misuse and mood disorders following traumatic brain injury. Arch Gen Psychiatry 62:742–749
van Reekum R, Cohen T, Wong J (2000) Can traumatic brain injury cause psychiatric disorders? J Neuropsychiatry Clin Neurosci 12:316–327
Rao V, Mielke M, Xu X, Smith GS, McCann UD, Bergey A et al (2012) Diffusion tensor imaging atlas-based analyses in major depression after mild traumatic brain injury. J Neuropsychiatry Clin Neurosci 24:309–315
Zhou Y, Milham MP, Lui YW, Miles L, Reaume J, Sodickson DK et al (2012) Default-mode network disruption in mild traumatic brain injury. Radiology 265:882–892
Maller JJ, Thomson RH, Pannek K, Rose SE, Bailey N, Lewis PM et al (2012) The (Eigen) value of diffusion tensor imaging to investigate depression after traumatic brain injury. Hum Brain Mapp. doi:10.1002/hbm.22171 (Epub ahead of print)
Tong KA, Ashwal S, Holshouser BA, Shutter LA, Herigault G, Haacke EM et al (2003) Hemorrhagic shearing lesions in children and adolescents with posttraumatic diffuse axonal injury: improved detection and initial results. Radiology 227:332–339
Wang D, Li WB, Wei XE, Li YH, Dai YM (2012) An investigation of age-related iron deposition using susceptibility weighted imaging. PLoS One 7:e50706
Tong KA, Ashwal S, Obenaus A, Nickerson JP, Kido D, Haacke EM (2008) Susceptibility-weighted MR imaging: a review of clinical applications in children. Am J Neuroradiol 29:9–17
Goos JD, van der Flier WM, Knol DL, Pouwels PJ, Scheltens P, Barkhof F et al (2011) Clinical relevance of improved microbleed detection by susceptibility-weighted magnetic resonance imaging. Stroke 42:1894–1900
Beauchamp MH, Beare R, Ditchfield M, Coleman L, Babl FE, Kean M et al (2013) Susceptibility weighted imaging and its relationship to outcome after pediatric traumatic brain injury. Cortex 49:591–598
Gould KR, Ponsford JL, Johnston L, Schönberger M (2011) The nature, frequency and course of psychiatric disorders in the first year after traumatic brain injury: a prospective study. Psychol Med 41:2099–2109
Hart T, Hoffman JM, Pretz C, Kennedy R, Clark AN, Brenner LA (2012) A longitudinal study of major and minor depression following traumatic brain injury. Arch Phys Med Rehabil 93:1343–1349
Paterakis K, Karantanas AH, Komnos A, Volikas Z (2000) Outcome of patients with diffuse axonal injury: the significance and prognostic value of MRI in the acute phase. J Trauma 49:1071–1075
Smith DH, Meaney DF, Shull WH (2003) Diffuse axonal injury in head trauma. J Head Trauma Rehabil 18:307–316
Wallesch CW, Curio N, Kutz S, Jost S, Bartels C, Synowitz H (2001) Outcome after mild-to-moderate blunt head injury: effects of focal lesions and diffuse axonal injury. Brain Inj 15:401–412
Jorge RE, Robinson RG, Moser D, Tateno A, Crespo-Facorro B, Arndt S et al (2004) Major depression following traumatic brain injury. Arch Gen Psychiatry 61:42–50
Ohara K, Nishii R, Nakajima T, Kokai M, Morita Y et al (2004) Alterations of symptoms with borderline personality disorder after fronto-temporal traumatic brain injury. A case study. Seishin Shinkeigaku Zasshi 106:458–466
Acknowledgments
This study is supported by the National Natural Scientific Fund of China (No. 81000609, No. 81271540 and No. 81301213).
Conflict of interest
The authors have no financial interests to disclose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Wang, X., Wei, XE., Li, MH. et al. Microbleeds on susceptibility-weighted MRI in depressive and non-depressive patients after mild traumatic brain injury. Neurol Sci 35, 1533–1539 (2014). https://doi.org/10.1007/s10072-014-1788-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10072-014-1788-3