Abstract
The aim of this study was to evaluate the effects of electrical stimulation program on pain, disability, and quadriceps strength in the patients with knee osteoarthritis. Fifty women diagnosed as knee osteoarthritis were randomized into two groups as electrical stimulation and biofeedback-assisted isometric exercises. Both of the programs were performed 5 days a week, for a duration of 4 weeks. Outcome measures for pain were visual analogue scale pain score and Western Ontario McMaster osteoarthritis index (WOMAC) pain score. Disability and stiffness were assessed with WOMAC physical function and stiffness score. One repetition maximum (RM) and 10 RM were used for measuring quadriceps strength. In addition, 50 m walking time and 10 steps stairs climbing up-down time were evaluated. Both groups showed significant improvements in pain, physical function, and stiffness scores after the therapy. There were statistically significant improvements in 50 m walking time and 10 steps stairs climbing up-down time and 1 RM and 10 RM values indicating the improvement in muscle strength. In addition, there were no significant differences between the groups after the therapy. We conclude that electrical stimulation treatment was as effective as exercise in knee osteoarthritis and electrical stimulation treatment can be suggested especially for the patients who have difficulty in or contraindications to perform an exercise program.
Similar content being viewed by others
Introduction
Knee osteoarthritis (OA) is a painful condition causing disability and muscle weakness. Radiographic evidence of OA occurs in the majority of people by 65 years of age and in about 80% of those who are more than 75 years of age [1, 2]. Pathologic changes in OA involve the whole joint in the form of focal and progressive hyaline articular cartilage loss with concomitant changes in the bone underneath the cartilage, including development of marginal outgrowths, osteophytes, and increased thickness of the bony envelope (bony sclerosis). Soft-tissue structures in and around the joint are also affected [3]. Knee OA is an important cause of disability in older people due to chronic joint pain, loss of range of motion, and muscle weakness. Exercise therapy aims at reduction of pain and disability. This is achieved through improvement of muscle strength, joint stability, range of joint motion, and aerobic capacity. Certainly, in patients with OA, regular exercise can improve pain control, proprioception, controlled strength, instability, and endurance, all of which improve functional independence [4, 5]. The term of biofeedback (BF) refers to the use of appropriate instrumentation to transduce muscle potentials into auditory or visual signals for the purpose of increasing or decreasing voluntary activity. BF improves the rate of functional recovery of the quadriceps femoris muscle significantly during the muscle strengthening exercises [6].
The mechanism of pain relief with electrical stimulation (ES) is explained by the gate-control theory developed by Melzac and Wall. ES causes facilitation in substantia gelatinosa at the level of medulla spinalis by stimulating A-α and A-β fiber, which do not transmit pain sense and reduces pain sense by inhibiting A-Δ and C fiber which transmit pain sense in presynaptic area. ES increases muscle strength, and decreases joint stiffness and spasm in muscle as well [7].
In this study, we aimed to evaluate the effects of ES program, on pain, disability, and quadriceps strength, functional performance in the patients with knee OA.
Materials and methods
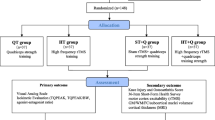
Fifty women aged between 42 and 74 years, who had been diagnosed as knee OA according to American College of Rheumatology (ACR) criteria were enrolled in the study [8]. The patients were informed of the purpose of the study and gave their consent. Standing anteroposterior and lateral radiographs of both knees of each patient were obtained, and the severity of OA in the tibiofemoral compartment was graded according to the criteria of Kellgren-Lawrence by a physiatrist (FC) who was blind to patients’ clinical data [8]. Exclusion criteria were the following: serious medical conditions for which exercise would be contraindicated, neuromuscular or dermatologic disease that involves the lower extremities, exercise program that may cause increase of muscle strength within the previous months, implanted cardiac pacemaker or defibrillator, inflammatory arthropathy, contracture, story of trauma within the previous 6 months, and grade 4 OA.
Patients were randomized into two groups. Each group had 25 participants. Group I received ES, while group II received BF-assisted isometric exercise. All patients came to the outpatient department for ES and exercise treatments. For both groups, 20-min duration therapy was applied 5 days a week. Both groups were treated for 4 weeks. Patients were evaluated before and after the therapy. No dropouts occurred during the trial and all subjects in both groups completed the treatment.
ES group
The patient was seated on the treatment chair with the hip at 90° and knee at 60° of flexion. The ankle of the patient was stabilized with a 5-kg load to prevent the isotonic contractions of the quadriceps muscle. Two of the four electrodes were placed on rectus femoris and vastus medialis muscles and the other two were placed on the vastus lateralis muscles’ motor points (Endomed-CV 405). The asymmetric biphasic wave was applied with the frequency of 50 Hz and 200 μs of phase time. The intensity of the current was arranged separately one by one for each patient until apparent muscle contraction was established (70–120 mA). The stimulation was applied as 10 s of contraction and 10 s of relaxation.
BF exercise group
The patient seated with the hip at 90° and knee at 25–30° of flexion. Two superficial electrodes (Enraf Myomed-432) were placed sequentially over the patient’s rectus femoris, vastus medialis, and vastus lateralis muscles. The patients were asked to perform an isometric contraction. The patient was asked to suppress her knee on the rolled pillow that was placed under the knee and hold it contracted in that position for 10 s. Fifty s of relaxation was given to the patient. The patient was asked to try to increase the visual and auditory signals that she perceived at every contraction.
Outcome measures for pain were visual analogue scale (VAS) pain score in activity, at night, at rest and Western Ontario McMaster osteoarthritis index (WOMAC) pain score [9].
Disability and stiffness were assessed with WOMAC physical function and stiffness score. One repetition maximum (RM) and 10 RM were used for measuring quadriceps strength [10, 11]. 1 RM and 10 RM performed bilaterally. Objective assessment of functional performance was obtained by timing the patients walking as fast as they could for 50 m, ascent and descent of a straight flight of stairs consisting of 10 steps.
Statistical analyses
Results were expressed as mean value±SD. Within-group and between-group differences were investigated. Wilcoxon signed rank test was used for within-group change. Mann-Whitney U test was used for the comparison of the groups. P values less than 0.05 were considered statistically significant.
Results
The mean age of the ES group and BF group were 54.76±20 years and 54.68±1.77 years, respectively. Body mass index (BMI) was 32.69±0.70 for the ES group and 32.77±0.89 for the BF group. There was no significant difference between the groups in terms of age and BMI (p>0.05). Clinical and demographic features of ES group and BF-assisted isometric exercise group are described in Table 1.
Pain
Both groups showed significant improvements in VAS and WOMAC pain scores. There was no statistically significant difference between the groups after the therapy (p>0.05) (Table 2).
Physical function and stiffness
There were also significant improvements for WOMAC physical function and stiffness scores in both groups. Statistically significant differences could not be demonstrated between the groups (p>0.05) (Table 2).
Functional performance
There were statistically significant improvements in 50 m walking time and 10 steps stairs climbing up-down time (p<0.001 and p<0.001, respectively). There was no statistically significant difference between the groups after the therapy (p>0.05) (Table 2).
Muscle strength
1 RM and 10 RM values improved significantly at the end of 4 weeks, compared with pretreatment values of both treatments. No statistically significant difference was observed between the groups after the therapy (p>0.05) (Table 2).
Discussion
Osteoarthritis of the knee is reported to be a major health problem worldwide. OA of the knee results to more disability and clinical symptoms than any other joint [12]. Quadriceps weakness may be etiologically related to the initiation, the progression, or both, of pathologic changes in some persons with OA of the knee. In knee OA, the pain and dysfunction cause a reflex inhibition on the quadriceps femoris muscle. This arthrogenous muscle inhibition has been attributed to alter afferent input from the diseased joint and consequent reduction in efferent motor neuron stimulation of the quadriceps [13]. Whether muscle inhibition is a precursor of quadriceps atrophy remains to be determined. Quadriceps weakness precedes and may be of pathogenetic importance in the development of knee pain and disability. In addition, because quadriceps action serves as a brake, retarding the rate of descent of the leg at the end of the swing phase of gait, quadriceps weakness could accelerate damage to articular cartilage in the knee [14, 15]. Treatments have generally targeted pain assuming that disability would improve as a direct result of improvement in pain. However, there is evidence suggesting that determinants of pain and disability differ. Treatments have been more successful at decreasing pain rather than preventing disability. Many of the factors that lead to disability can be improved with exercise [5]. Regular exercise can improve pain control, proprioception, strength, instability, and endurance, all of which improve functional independence [4]. In many studies significant improvement in WOMAC pain and WOMAC physical function scores, increase in the strength of the quadriceps and a significant improvement in the periods of functional performances such as walking and climbing stairs are observed with regular exercise [1, 16–20].
Although there are many reports about the effectiveness of exercise in patients with knee OA, studies showing the effectiveness of ES treatment are limited. In this study, we aimed to investigate the effect of ES on pain and disability in knee OA as an alternative treatment. Electrical stimulation causes an increase in the muscle strength with the changes in the muscle fibers and the capillary system. It also prevents the muscle atrophy due to the prolonged immobilization [21]. Besides improving the muscle strength, ES also decreases the pain and increases the functional performance due to the gate-control theory of Melzack and Wall [21, 22]. Pekindil at al [22] applied alternative biphasic waves in 75–85 Hz frequency on the quadriceps muscles of 16 healthy women between the ages of 21–45 for 20 days. They found an increase in the muscle strength. In their study, Selkowitz et al. [23] aimed to determine if training isometrically with ES alone would significantly increase isometric strength of the quadriceps femoris muscle and they found an increase in the isometric muscle strength of the quadriceps muscle. Gaines at al. [24], examined effects of a home-based, 12-week neuromuscular electrical stimulation (NMES) of the quadriceps femoris to decrease knee pain in older adults with OA of the knee and their results suggested that NMES improved pain in a short time after stimulation. We also found decrease in pain, and a significant increase in muscle strength and functional performance in ES group.
BF techniques are used in neural and muscular rehabilitation effectively because they facilitate the formation of contraction. They also increase the motivation and cooperation of the patient for the treatment and thus they are recommended in exercise protocols [6]. In a study by Lucca and Recchiuti [25], one of the groups performed isometric exercise and received electromyographic BF, and the other group performed isometric exercise without BF. The combination of BF and isometric exercise was shown to produce greater gains in muscle strength than isometric exercise alone over a 19-day training period. Levitt et al. [6] assessed the effectiveness of isometric exercise and EMG BF in the rehabilitation of 51 patients after knee surgery. They found that patients given EMG BF during postoperative exercise demonstrated significantly greater extensor torque and quadriceps muscle fiber recruitment than the patients given exercise alone. These studies showed that EMG BF-exercise combination could be advised as a treatment for strengthening the muscle. They determined that the motivation of the patients was better when they performed exercise with BF during the treatment. Therefore, we also performed isometric exercise with BF to increase the motivation of the patients.
There is variation in the content and duration of the ES treatment in the literature. Length of the ES treatment ranged from 3 to 12 weeks and the frequency ranged from 50 to 85 Hz [22–24]. In their study, Valli et al. [26] investigated the effect of low intensity ES on quadriceps strength, and found an increase of muscle strength beginning at the third day. The amount and duration of our therapy were in agreement with previously published studies.
In the literature, there are limited studies about the effects of ES on disability and physical performance in knee OA. We observed that ES was effective as an exercise program in knee OA. We observed not only a decrease in pain, but also an increase in quadriceps strength and improvement in physical function and functional performance. So, we can recommend ES treatment for the patients who have difficulty in or contraindications to perform an exercise program. A limitation of our study is lack of long-term observation. Because we evaluated the patients only at the end of the therapy, it is not clear whether the improvements were maintained in the long term. Further studies are needed to clarify the long-term effects of ES and the clinical significance of continuation of exercises.
References
Hurley MV, Scott DL (1998) Improvements in quadriceps sensorimotor function and disability of patients with knee osteoarthritis following a clinically practicable exercise regime. Br J Rheumatol 37:1181–1187
Cooper C (1998) Epidemiology. In: Klippel JH, Dieppe PA (eds) Rheumatology, 2nd edn. Mosby, London, pp 8.2.1–8.2.8
Felson DT, Lawrence RC, Dieppe PA et al (2000) Systemic risk factors for osteoarthritis. In: Felson DT (ed) Osteoarthritis: new insights. Part 1: the disease and its risk factors. Ann Intern Med 133:635–646
Petrella RJ (2000) Is exercise effective treatment of osteoarthritis of the knee? Br J Sports Med 34:326–331
Baker K, McAlindon T (2000) Exercise for knee osteoarthritis. Curr Opin Rheumatol 12:456–463
Levitt R, Deisinger JA, JR Wall et al (1995) EMG feedback-assisted postoperative rehabilitation of minor arthroscopic knee surgeries. J Sports Med Phys Fitness 35:218–23
Liberson WT (1984) Electrotherapy In: Asa P Ruskın (ed) Current therapy. Physiatry. Saunders, Philadelphia, pp 161–191
Flores RH, Hochberg MC (1998) Definition and classification of osteoarthritis. In: Brandt K, Doherty M, Lohmander LS (eds) Osteoarthritis. Oxford University Press, New York, pp 1–12
Evcik D, Sonel B (2002) Effectiveness of a home-based exercise therapy and walking program on osteoarthritis of the knee. Rheumatol Int 22:103–106
Elliott KJ, Sale C, Cable NT (2002) Effects of resistance training and detraining on muscle strength and blood lipid profiles in postmenopausal women. Br J Sports Med 36:340–344
Hakkinen K, Kraemer WS, Pakarinen A et al (2002) Effects of heavy resistance power training on maximal strength, muscle morphology and hormonal response patterns in 65–75 years old men and women. Can J Appl Physiol 27:213–231
Rogind H, Bibow-Nielsen B, Jensen B et al (1998) The effects of a physical training program on patients with osteoarthritis of the knees. Arch Phys Med Rehabil 79:1421–1427
Rutherford OM, Jones DA, Newham DJ (1986) Clinical and experimental application of the percutaneous twitch superimposition technique for the study of human muscle activation. J Neuro Neurosurg Psychiatry 49:1288–1291
Maurer BT, Stern AG, Kinossian B et al (1999) Osteoarthritis of the knee: isokinetic quadriceps exercise versus and educational intervention. Arch Phys Med Rehabil 80:1293–1299
Slemenda C, Brandt KD, Heilman DK et al (1997) Quadriceps weakness and osteoarthritis of the knee. Ann Intern Med 127:97–104
Fisher NM, Gresham G, Pendergast DR (1993) Effects of a quantitative progressive rehabilitation program applied unilaterally to the osteoarthritic knee. Arch Phys Med Rehabil 74:1319–1326
Mohr T, Carlson B, Sulentıc C et al (1985) Comparison of isometric exercise and high volt stimulation on quadriceps femoris muscle strength. Phys Ther 65:606–612
Kuptniratsaikul V, Tosayanonda O, Nilganuwong S et al (2002) The efficacy of a muscle exercise program to improve functional performance of the knee in patients with osteoarthritis. J Med Assoc Thai 85:33–40
Deyle GD, Henderson NE, Matekel RL et al (2000) Effectiveness of manual physical therapy and exercise in osteoarthritis of the knee. A randomized, controlled trial. Ann Intern Med 132:173–181
O’Reilly SC, Muir KR, Doherty M (1999) Effectiveness of home exercise on pain and disability from osteoarthritis of the knee: randomized controlled trial. Ann Rheum Dis 58:15–19
Mysiw WJ, Jackson RD (2000) Electrical stimulation. In: Braddom RL (ed) Physical medicine and rehabilitation, 2nd edn. Saunders, Philadelphia, pp 459–487
Pekindil Y, Sarıkaya A, Birtane M et al (2001) 99mTc-Sestamibi muscle scintigraphy to asses the response to neuromuscular electrical stimulation of normal quadriceps femoris muscle. Ann Nucl Med 15:397–401
Selkowıtz DM (1985) Improvement in isometric strength of the quadriceps femoris muscle after training with electrical stimulation. Phys Ther 65:186–195
Gaines JM, Metter EJ, Talbot LA (2004) The effect of neuromuscular electrical stimulation on arthritis knee pain in older adults with osteoarthritis of the knee. Appl Nurs Res 17:201–206
Lucca JA, Recchiuti SJ (1983) Effect of electromyographic biofeedback on an isometric strengthening program. Phys Ther 63:200–203
Valli P, Boldrini L, Bianchedi D et al (2002) Effect of low intensity electrical stimulation on quadriceps muscle voluntary maximal strength. J Sports Med Phys Fitness 42:425–430
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Durmuş, D., Alaylı, G. & Cantürk, F. Effects of quadriceps electrical stimulation program on clinical parameters in the patients with knee osteoarthritis. Clin Rheumatol 26, 674–678 (2007). https://doi.org/10.1007/s10067-006-0358-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10067-006-0358-3