Abstract
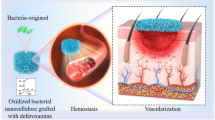
The efficacy of skin regeneration devices consisting of nonwoven filters and peripheral blood cells was investigated for wound healing. We previously found that human peripheral blood cells enhanced their production of growth factors, such as transforming growth factor β1 (TGF-β1) and vascular endothelial growth factor, when they were captured on nonwoven filters. Cells on biodegradable filters were expected to serve as a local supply of growth factors and cell sources when they were placed in wounded skin. Nonwoven filters made of biodegradable polylactic acid (PLA) were cut out as 13-mm disks and placed into cell-capturing devices. Mouse peripheral blood was filtered, resulting in PLA filters with mouse peripheral blood cells (m-PBCs) at capture rates of 65.8 ± 5.2 %. Then, the filters were attached to full-thickness surgical wounds in a diabetic db/db mouse skin for 14 days as a model of severe chronic wounds. The wound area treated with PLA nonwoven filters with m-PBCs (PLA/B+) was reduced to 8.5 ± 12.2 % when compared with day 0, although the non-treated control wounds showed reduction only to 60.6 ± 27.8 %. However, the PLA filters without m-PBCs increased the wound area to 162.9 ± 118.7 %. By histopathological study, the PLA/B+ groups more effectively accelerated formation of epithelium. The m-PBCs captured on the PLA filters enhanced keratinocyte growth factor (FGF-7) and TGF-β1 productions in vitro, which may be related to wound healing. This device is useful for regeneration of wounded skin and may be adaptable for another application.



Similar content being viewed by others
References
Hori H, Iwamoto U, Niimi G, Shinzato M, Hiki Y, Tokushima Y, Kawaguchi K, Ohashi A, Nakai S, Yasutake M, Kitaguchi N. Appropriate nonwoven filters effectively capture human peripheral blood cells and mesenchymal stem cells, which show enhanced production of growth factors. J Artif Organs. 2015;18:55–63.
Barrientos S, Stojadinovic O, Golinko MS, Brem H, Tomic-Canic M. Growth factors and cytokines in wound healing. Wound Repair Regen. 2008;16:585–601.
Mast BA, Schultz GS. Interactions of cytokines, growth factors, and proteases in acute and chronic wounds. Wound Repair Regen. 1996;4:411–20.
Robson MC. The role of growth factors in the healing of chronic wounds. Wound Repair Regen. 1997;5:12–7.
Akita S, Akino K, Imaizumi T, Hirano A. A basic fibroblast growth factor improved the quality of skin grafting in burn patients. Burns. 2005;31:855–8.
Rubin JS, Bottaro DP, Chedid M, Miki T, Ron D, Cheon G, Taylor WG, Fortney E, Sakata H, Finch PW, et al. Keratinocyte growth factor. Cell Biol Int. 1995;19:399–411.
Tsuboi R, Sato C, Kurita Y, Ron D, Rubin JS, Ogawa H. KGF (FGF-7) stimulates migration and plasminogen activator activity of normal human keratinocytes. J Invest Dermatol. 1993;101:49–53.
Staiano-Coico L, Krueger JG, Rubin JS, D’limi S, Vallat VP, Valentino L, Fahey T 3rd, Hawes A, Kingston G, Madden MR, et al. Human keratinocyte growth factor effects in a porcine model of epidermal wound healing. J Exp Med. 1993;178:865–78.
Penn JW, Grobbelaar AO, Rolfe KJ. The role of the TGF-β family in wound healing, burns and scarring: a review. Int J Burns Trauma. 2012;2:18–28.
Edelman ER, Nugent MA, Karnovsky MJ. Perivascular and intravenous administration of basic fibroblast growth factor: vascular and solid organ deposition. Proc Natl Acad Sci USA. 1993;90:1513–7.
Schultz GS, Sibbald RG, Falanga V, Ayello EA, Dowsett C, Harding K, Romanelli M, Stacey MC, Teot L, Vanscheidt W. Wound bed preparation: a systematic approach to wound management. Wound Repair Regen. 2003;11:S1–28.
Jain R, Agarwal A, Kierski PR, Schurr MJ, Murphy CJ, McAnulty JF, Abbott NL. The use of native chemical functional groups presented by wound beds for the covalent attachment of polymeric microcarriers of bioactive factors. Biomaterials. 2013;34:340–52.
Michaels J, Churgin SS, Blechman KM, Greives MR, Aarabi S, Galiano RD, Gurtner GC. db/db mice exhibit severe wound-healing impairments compared with other murine diabetic strains in a silicone-splinted excisional wound model. Wound Repair Regen. 2007;15:665–70.
Galiano RD, Michaels J 5th, Dobryansky M, Levine JP, Gurtner GC. Quantitative and reproducible murine model of excisional wound healing. Wound Repair Regen. 2004;12:485–92.
Stroman PW, Dorvil JC, Marois Y, Poddevin N, Guidoin R. In vivo time course studies of the tissue responses to resorbable polylactic acid implants by means of MRI. 1999:42;210–4.
Roberts AB, Sporn MB, Assoian RK, Smith JM, Roche NS, Wakefield LM, Heine UI, Liotta LA, Falanga V, Kehrl JH, et al. Transforming growth factor type β: rapid induction of fibrosis and angiogenesis in vivo and stimulation of collagen formation in vitro. Proc Natl Acad Sci USA. 1986;83:4167–71.
Riedel K1, Riedel F, Goessler UR, Germann G, Sauerbier M. Tgf-beta antisense therapy increases angiogenic potential in human keratinocytes in vitro. Arch Med Res. 2007:38;45–51.
Acknowledgments
The authors thank Ms. Mikiko Ariga of Asahi Kasei Fibers Corporation for providing the nonwoven filters. The authors thank Ms. Miwa Sakata, and Mr. Masaya Yamamoto, Kazuki Kawamura and Tomoya Oguri for their technical assistance. This work was partly supported by a research grant from Asahi Kasei Corporation and JSPS KAKENHI Grant Number 25410232.
Conflict of interest
Mikitomo Yasutake, General Manager, and Ushio Iwamoto, Chief Researcher, are employees of Asahi Kasei Corporation Co., Ltd. (Cell Therapy Technology, Healthcare R&D Center) and have the stock of the company. Yasuo Tokushima is an employee of Asahi Kasei Medical Co., Ltd. (Manager of Scientific and Technical Department, Japan Operation Division, Blood Purification Business Unit), and has the stock of Asahi Kasei Corporation Co., Ltd. Nobuya Kitaguchi has the stock of Asahi Kasei Corporation Co., Ltd. Nobuya Kitaguchi and Hideo Hori received the research funding from Asahi Kasei Corporation Co., Ltd. The other authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding authors
Additional information
U. Iwamoto and H. Hori contributed equally.
Rights and permissions
About this article
Cite this article
Iwamoto, U., Hori, H., Takami, Y. et al. A novel cell-containing device for regenerative medicine: biodegradable nonwoven filters with peripheral blood cells promote wound healing. J Artif Organs 18, 315–321 (2015). https://doi.org/10.1007/s10047-015-0845-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10047-015-0845-x