Abstract
Purpose
The Lichtenstein technique (LT) has been recognized as the standard treatment for inguinal hernia in adults owing to the high recurrence rates of tissue-based repairs. However, Desarda technique (DT) appeared as promising tissue-based repair that provided low incidence of recurrence without the need for implanting prosthetic or foreign materials in the inguinal canal. This meta-analysis of randomized controlled trials (RCTs) comparing DT and LT for primary inguinal hernia in adults aimed to determine which technique had better clinical outcome regarding recurrence and complication rates.
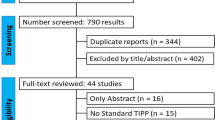
Methods
A systematic literature search for RCTs comparing between DT and LT was conducted using electronic databases and Google scholar service. Patients’ characteristics, technical details, recurrence and complication rates, and time to resume daily activities were extracted from the original studies and analyzed.
Results
Six RCTs comprising 2159 patients (89% males) were included. No significant difference in the incidence of recurrence between both techniques was detected (OR = 0.946; P = 0.91). The overall complication rate of LT was significantly higher than DT (OR = 1.86; P < 0.001). LT had significantly higher rates of seroma formation and surgical site infection (OR = 2.17; P = 0.007) and (OR = 2.17; P = 0.029), respectively. Postoperative pain, operation time, and time to resume normal activities were comparable in both groups.
Conclusion
Both DT and LT provided satisfactory treatment for primary inguinal hernia with low recurrence rates and acceptable rates of complications that were significantly less after DT. More well-designed RCTs with longer follow-up are required for further validation of the DT.





Similar content being viewed by others
References
Awad SS, Fagan SP (2004) Current approaches to inguinal hernia repair. Am J Surg 188(6A Suppl):9S–16S
Primatesta P, Goldacre MJ (1996) Inguinal hernia repair: incidence of elective and emergency surgery, readmission and mortality. Int J Epidemiol 25:835–839
Scott NW, McCormack K, Graham P, Go PM, Ross SJ, Grant AM (2002) Open mesh versus non-mesh for repair of femoral and inguinal hernia. Cochrane Database Syst Rev (4):CD002197
Simons MP, Aufenacker T, Bay-Nielsen M et al (2009) European Hernia Society guidelines on the treatment of inguinal hernia in adult patients. Hernia 13:343–403
Lichtenstein IL, Shulman AG, Amid PK et al (1989) The tension free hernioplasty. Am J Surg 157:88–193
Amid PK, Shulman AG, Lichtenstein IL (1996) Open ‘‘tension free’’ repair of inguinal hernias: the Lichtenstein technique. Eur J Surg 162:447–453
Robert E (2001) Condon, groin pain after hernia repair. Ann Surg 233(1):8
D’Amore L, Gossetti F, Vermeil V et al (2008) Long-term discomfort after plug and patch hernioplasty. Hernia 12:445–446
Hamy A, Paineau J, Savigny JL et al (1997) Sigmoid perforation, an exceptional late complication of peritoneal prosthesis for treatment of inguinal hernia. Int Surg 82:307–308
Sakorafas GH, Halikias I, Nissotakis C et al (2001) Open tension free repair of inguinal hernias; the Lichtenstein technique. BMC Surg 1:3
Amato B, Moja L, Panico S, Persico G, Rispoli C, Rocco N, Moschetti I (2009) Shouldice technique versus other open techniques for inguinal hernia repair. Cochrane Database Syst Rev 7(4):CD001543. doi:10.1002/14651858.CD001543.pub3
Desarda MP (2001) New method of inguinal hernia: a new solution. ANZ J Surg 71:241–244
Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JP, Clarke M, Devereaux PJ, Kleijnen J, Moher D (2009) The PRISMA statement for reporting systematic reviews and metaanalyses of studies that evaluate healthcareinterventions: explanation and elaboration. BMJ 21(339):b2700
Manyilirah W, Kijjambu S, Upoki A, Kiryabwire J (2012) Comparison of non-mesh (Desarda) and mesh (Lichtenstein) methods for inguinal hernia repair among black African patients: a short-term double-blind RCT. Hernia 16(2):133–144 Epub 2011 Oct 8
Szopinski J, Dabrowiecki S, Pierscinski S, Jackowski M, Jaworski M, Szuflet Z (2012) Desarda versus Lichtenstein technique for primary inguinal hernia treatment: 3-year results of a randomized clinical trial. World J Surg 36(5):984–992
Rodríguez P, Herrera P, Gonzalez O, Alonso J, Blanco H (2013) A randomized trial comparing lichtenstein repair and no mesh desarda repair for inguinal hernia: a study of 1382 patients. East Central Afr J Surg 18(2):18–25
Youssef T, El-Alfy K, Farid M (2015) Randomized clinical trial of Desarda versus Lichtenstein repair for treatment of primary inguinal hernia. Int J Surg 20:28–34
Bhatti I, Ishaqu H, Ahmad Z, Dar U (2015) Desarda’s versus lichtenstein technique of hernia repair. Pak J Med Health Sci 9(4):1331
Ahmad I, Dwivedi AC, Srivastava SK, Singh HP, Singh AK (2016) randomized trial comparing Lichenstein and Desarda technique for open inguinal hernia repair—a study of 100 patient. J Dent Med Sci 15(3):17–20. doi:10.9790/0853-1503081720
Higgins JP, Altman DG, Gøtzsche PC, Jüni P, Moher D, Oxman AD, Savovic J, Schulz KF, Weeks L, Sterne JA, Cochrane Bias Methods Group, Cochrane Statistical Methods Group (2011) The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ 18(343):d5928
Hay JM, Boudet MJ, Fingerhut A et al (1995) Shouldice inguinal hernia repair in the male adult: the gold standard? A multicentral controlled trial in 1578 patients. Ann Surg 222:719–727
Shouldice EB (2003) The Shouldice repair for groin hernias. Surg Clin North Am 83:1163–1187
Junge K, Rosch R, Klinge U et al (2006) Risk factors related to recurrence in inguinal hernia repair: a retrospective analysis. Hernia 10:309–315
National Institute of Clinical Excellence(NICE) (2004) Final appraisal determination, laparoscopic surgery for inguinal hernia repair. London
Amid PK (2004) Lichtenstein tension-free hernioplasty: its inception, evolution, and principles. Hernia 8:1–7
Kurzer M, Belsham PA, Kark AE (2003) The Lichtenstein repair for groin hernias. Surg Clin North Am 83:1099–1117
Verstraete L, Becaus N, Swannet H, Ceelen W, Duchateau L, Speybroeck N (2015) Long term outcome after lichtenstein hernia repair using general, locoregional or local anaesthesia. Acta Chir Belg 115(2):136–141
Zieren J, Beyersdorff D, Beier KM et al (2001) Sexual function and testicular perfusion after inguinal hernia repair with mesh. Am J Surg 181(3):204–206
Kulacoglu H (2011) Current options in inguinal hernia repair in adult patients. Hippokratia 15(3):223–231
Earle DB, Mark LA (2008) Prosthetic material in inguinal hernia repair: how do I choose? Surg Clin North Am 88(1):179–201
Losanoff JE, Millis JM (2006) Aponeurosis instead of prosthetic mesh for inguinal hernia repair: neither physiological nor new. Hernia 10(2):1981–1999
Desarda MP (2003) Surgical physiology of inguinal hernia repair—a study of 200 cases. BMC Surgery. 3:2. doi:10.1186/1471-2482-3-2
Desarda MP (2006) Physiological repair of inguinal hernia: a new technique (study of 860 patients). Hernia 10(2):143–146 Epub 2005 Dec 9
Desarda MP, Ghosh DN (2006) Comparative study of open mesh repair and Desarda’s nomesh repair in a district hospital in India. East Central Afr J Surg 11(2):18–34
Mitura K, Romańczuk M (2008) Comparison between two methods of inguinal hernia surgery–Lichtenstein and Desarda. Pol Merkur Lekarski 24(143):392–395
Klinge U, Zheng H, Si ZY et al (1999) Synthesis of type I and III collagen, expression of fibronectin and matrix metalloproteinases1 and 13 in hernia sac of patients with inguinal hernia. Int J Surg Investig 1:219–227
Zheng H, Si Z, Kasperk R et al (2002) Recurrent inguinal hernia: disease of the collagen matrix? World J Surg 26:401–408
Rutkow IM, Robbins AW (1993) Demographic, classificatory, and socioeconomic aspects of hernia repair in the United States. Surg Clin North Am 73(3):413–426
Taylor EW, Duffy K, Lee K, Hill R, Noone A, Macintyre I, King PM, O’Dwyer PJ (2004) Surgical site infection after groin hernia repair. Br J Surg 91(1):105–111
(1986) Classification of chronic pain. Descriptions of chronic pain syndromes and definitions of pain terms. Prepared by the International Association for the Study of Pain, Subcommittee on Taxonomy. Pain Suppl 3:S1-226
Alfieri S, Amid PK, Campanelli G et al (2011) International guidelines for prevention and management of postoperative chronic pain following inguinal hernia surgery. Hernia 15:239–249
BayNielsen M, Perkins FM, Kehlet H (2001) Pain and functional impairment 1 year after inguinal herniorrhaphy: a nationwide questionnaire study. Ann Surg 233:1–7
de Goede B, Klitsie PJ, van Kempen BJ, Timmermans L, Jeekel J, Kazemier G, Lange JF (2013) Meta-analysis of glue versus sutured mesh fixation for Lichtenstein inguinal hernia repair. Br J Surg 100(6):735–742. doi:10.1002/bjs.9072
McCormack K, Wake B, Perez J, Fraser C, Cook J, McIntosh E, Vale L, Grant A (2005) Laparoscopic surgery for inguinal hernia repair: systematic review of effectiveness and economic evaluation. Health Technol Assess 9(14):1–203
Löfgren J, Nordin P, Ibingira C, Matovu A, Galiwango E, Wladis A (2016) A randomized trial of low-cost mesh in groin hernia repair. N Engl J Med 374(2):146–153
Jones P, Jones S, Guarnieri F, Moscatelli F, Smaldone W, Nwamba C, Desarda M (2015) Inguinal hernia—mesh vs non mesh. Hernia 19(Suppl 1):S265–S266
Author information
Authors and Affiliations
Contributions
Sameh Emile designed the study, shared in acquisition and analysis of data, and drafted the manuscript. Hossam Elfeki shared in acquisition and analysis of data, drafting and critical revision of the manuscript. Both authors approved the final version of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
No conflict of interest to be declared by the authors.
Ethical approval
This article did not require ethical approval of any kind.
Human and animal rights
This article does not contain any studies with human participants or animals performed by any of the authors.
Informed consent
This article does not include patients, and therefore informed consent was not applicable.
Rights and permissions
About this article
Cite this article
Emile, S.H., Elfeki, H. Desarda’s technique versus Lichtenstein technique for the treatment of primary inguinal hernia: a systematic review and meta-analysis of randomized controlled trials. Hernia 22, 385–395 (2018). https://doi.org/10.1007/s10029-017-1666-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10029-017-1666-z