Abstract
Purpose
Treatment guidelines for abdominal wound dehiscence (WD) are lacking. The primary aim of the study was to compare suture to mesh repair in WD patients concerning incisional hernia incidence. Secondary aims were to compare recurrent WD, morbidity, mortality and long-term abdominal wall complaints.
Methods
A retrospective chart review of 46 consecutive patients operated for WD between January 2010 and August 2012 was conducted. Physical examination and a questionnaire enquiry were performed in January 2013.
Results
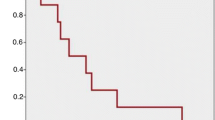
Six patients were treated by vacuum-assisted wound closure and mesh-mediated fascial traction (VAWCM) before definitive closure. Three patients died early resulting in 23 patients closed by suture and 20 by mesh repair. Five sutured, but no mesh repair patients had recurrent WD (p = 0.051) with a mortality of 60 %. Finally, 18 sutured and 21 mesh repair patients were eligible for follow-up. The incidence of incisional hernia was higher for the sutured patients (53 vs. 5 %, p = 0.002), while mesh repair patients had a higher short-term morbidity rate (76 vs. 28 %, p = 0.004). Abdominal wall complaints were rare in both groups.
Conclusions
Suture of WD was afflicted with a high incidence of recurrent WD and incisional hernia formation. Mesh repair overcomes these problems at the cost of more wound complications. VAWCM seems to be an alternative for treating contaminated patients until definitive closure is possible. Long-term abdominal wall complaints are uncommon after WD treatment.


Similar content being viewed by others
References
Bloemen A, van Dooren P, Huizinga BF, Hoofwijk AGM (2011) Randomized clinical trial comparing polypropylene or polydioxanone for midline abdominal wall closure. Br J Surg 98:633–639. doi:10.1002/bjs.7398
Webster C, Neumayer L, Smout R et al (2003) Prognostic models of abdominal wound dehiscence after laparotomy. J Surg Res 109:130–137
Sajid MS, Parampalli U, Baig MK, McFall MR (2011) A systematic review on the effectiveness of slowly-absorbable versus non-absorbable sutures for abdominal fascial closure following laparotomy. Int J Surg 9:615–625. doi:10.1016/j.ijsu.2011.09.006
van Ramshorst GH, Eker HH, Harlaar JJ et al (2010) Therapeutic alternatives for burst abdomen. Surg Technol Int 19:111–119
Meena K, Ali S, Chawla AS et al (2013) A prospective study of factors influencing wound dehiscence after midline laparotomy. SS 04:354–358. doi:10.4236/ss.2013.48070
Cliby WA (2002) Abdominal incision wound breakdown. Clin Obstet Gynecol 45:507–517
Grace RH, Cox S (1976) Incidence of incisional hernia after dehiscence of the abdominal wound. Am J Surg 131:210–212
Garg PK, Jain SK, Kaza RCM et al (2010) Staged closure after complete wound dehiscence: novel technique. Surgeon 8:177–178. doi:10.1016/j.surge.2009.10.012
Muckart DJ, Luvuno FM (1985) Abdominal wound disruption. A conservative approach. J R Coll Surg Edinb 30:47–49
van’t Riet M, De Vos Van Steenwijk PJ, Bonjer HJ et al (2004) Incisional hernia after repair of wound dehiscence: incidence and risk factors. Am Surg 70:281–286
van’t Riet M, de Vos van Steenwijk PJ, Bonjer HJ et al (2007) Mesh repair for postoperative wound dehiscence in the presence of infection: is absorbable mesh safer than non-absorbable mesh? Hernia 11:409–413. doi:10.1007/s10029-007-0240-5
White H, Cook J, Ward M (1977) Abdominal wound dehiscence. A 10-year survey from a district general hospital. Ann R Coll Surg Engl 59:337–341
Madsen G, Fischer L, Wara P (1992) Burst abdomen—clinical features and factors influencing mortality. Dan Med Bull 39:183–185
Mäkelä JT, Kiviniemi H, Juvonen T, Laitinen S (1995) Factors influencing wound dehiscence after midline laparotomy. Am J Surg 170:387–390
Abbott DE, Dumanian GA, Halverson AL (2007) Management of laparotomy wound dehiscence. Am Surg 73:1224–1227
Scholtes M, Kurmann A, Seiler CA et al (2012) Intraperitoneal mesh implantation for fascial dehiscence and open abdomen. World J Surg 36:1557–1561. doi:10.1007/s00268-012-1534-z
Greenburg AG, Saik RP, Peskin GW (1979) Wound dehiscence. Pathophysiology and prevention. Arch Surg 114:143–146
van Ramshorst GH, Eker HH, van der Voet JA et al (2013) Long-term outcome study in patients with abdominal wound dehiscence: a comparative study on quality of life, body image, and incisional hernia. J Gastrointest Surg 17:1477–1484. doi:10.1007/s11605-013-2233-2
Rogmark P, Petersson U, Bringman S et al (2013) Short-term outcomes for open and laparoscopic midline incisional hernia repair: a randomized multicenter controlled trial: The ProLOVE (prospective randomized trial on open versus laparoscopic operation of ventral eventrations) trial. Ann Surg. doi:10.1097/SLA.0b013e31828fe1b2
Petersson U, Acosta S, Bjorck M (2007) Vacuum-assisted wound closure and mesh-mediated fascial traction—a novel technique for late closure of the open abdomen. World J Surg 31:2133–2137. doi:10.1007/s00268-007-9222-0
Bjarnason T, Montgomery A, Hlebowicz J et al (2011) Pressure at the bowel surface during topical negative pressure therapy of the open abdomen: an experimental study in a porcine model. World J Surg 35:917–923. doi:10.1007/s00268-010-0937-y
Acosta S, Bjarnason T, Petersson U et al (2011) Multicentre prospective study of fascial closure rate after open abdomen with vacuum and mesh-mediated fascial traction. Br J Surg 98:735–743. doi:10.1002/bjs.7383
Israelsson LA, Jonsson T (1993) Suture length to wound length ratio and healing of midline laparotomy incisions. Br J Surg 80:1284–1286
Millbourn D, Cengiz Y, Israelsson LA (2009) Effect of stitch length on wound complications after closure of midline incisions: a randomized controlled trial. Arch Surg 144:1056–1059. doi:10.1001/archsurg.2009.189
Muysoms FE, Miserez M, Berrevoet F et al (2009) Classification of primary and incisional abdominal wall hernias. Hernia 13:407–414. doi:10.1007/s10029-009-0518-x
Korenkov M, Paul A, Sauerland S et al (2001) Classification and surgical treatment of incisional hernia. Results of an experts’ meeting. Langenbecks Arch Surg 386:65–73
Clay L, Franneby U, Sandblom G et al (2012) Validation of a questionnaire for the assessment of pain following ventral hernia repair—the VHPQ. Langenbecks Arch Surg 397:1219–1224. doi:10.1007/s00423-012-0932-x
Pavlidis TE, Galatianos IN, Papaziogas BT et al (2001) Complete dehiscence of the abdominal wound and incriminating factors. Eur J Surg 167:351–354. doi:10.1080/110241501750215221 (discussion 355)
Berrevoet F, Vanlander A, Sainz-Barriga M et al (2013) Infected large pore meshes may be salvaged by topical negative pressure therapy. Hernia 17:67–73. doi:10.1007/s10029-012-0969-3
Kosins AM, Scholz T, Cetinkaya M, Evans GRD (2013) Evidence-based value of subcutaneous surgical wound drainage: the largest systematic review and meta-analysis. Plast Reconstr Surg 132:443–450. doi:10.1097/PRS.0b013e3182958945
Suissa D, Danino A, Nikolis A (2011) Negative-pressure therapy versus standard wound care: a meta-analysis of randomized trials. Plast Reconstr Surg 128:498e–503e
Ingargiola MJ, Daniali LN, Lee ES (2013) Does the application of incisional negative pressure therapy to high-risk wounds prevent surgical site complications? A systematic review. Eplasty 13:e49
Hollinsky C, Sandberg S, Kocijan R (2007) Preliminary results with the reinforced tension line: a new technique for patients with ventral abdominal wall hernias. Am J Surg 194:234–239. doi:10.1016/j.amjsurg.2006.09.045
Conflict of interest
PP declares no conflict of interest. AM declares no conflict of interest. UP declares conflict of interest not directly related to the submitted work (honorarium for lectures arranged by KCI).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Petersson, P., Montgomery, A. & Petersson, U. Wound dehiscence: outcome comparison for sutured and mesh reconstructed patients. Hernia 18, 681–689 (2014). https://doi.org/10.1007/s10029-014-1268-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10029-014-1268-y