Abstract
Purpose
Nerve identification during open inguinal hernia herniorrhaphy has been suggested as one of the factors that may reduce the risk of development of persistent postherniorrhaphy pain. In this prospective study, we evaluated whether intraoperative inguinal nerve identification influenced the risk of development of persistent postherniorrhaphy pain, sensory dysfunction in the groin and functional ability score after open hernia repair.
Methods
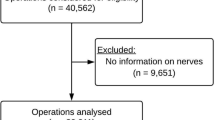
A total of 244 men with a primary inguinal hernia underwent open Lichtenstein repair in a high-volume hernia surgery centre, where information on inguinal nerve identification was registered during operation. Before the operation and 6 months postoperatively, functional pain-related impairment was assessed with Activities Assessment Scale and pain intensity scores with Numeric Rating Scale (NRS 0–10). Quantitative sensory testing in the groin was performed before operation and 6 months postoperatively, in order to investigate intraoperative inguinal nerve damage.
Results
The intraoperative nerve identification rates for the iliohypogastric, ilioinguinal and genitofemoral nerves were 94.7, 97.5 and 21.3 %, respectively. Thirty-nine patients (16.0 %) had substantial pain-related functional impairment at 6 months follow-up. There was no difference in risk of development of substantial pain-related functional impairment in patients with identification compared with non-identification of the iliohypogastric nerve (P = 1.0), the ilioinguinal nerve (P = 0.59), the genitofemoral nerve (P = 0.40) or all nerves (P = 0.52). There were no differences in regard to sensory loss in the groin area or in regard to improvement in functional outcome following surgery, between patients with and without nerve identification.
Conclusions
Although intraoperative inguinal nerve identification should be aimed at, other factors may contribute to the risk of nerve damage and persistent pain after open groin hernia repair.
Similar content being viewed by others
References
Aasvang E, Kehlet H (2005) Chronic postoperative pain: the case of inguinal herniorrhaphy. Br J Anaesth 95:69–76
Nienhuijs S, Staal E, Strobbe L, Rosman C, Groenewoud H, Bleichrodt R (2007) Chronic pain after mesh repair of inguinal hernia: a systematic review. Am J Surg 194:394–400
Kehlet H, Jensen TS, Woolf CJ (2006) Persistent postsurgical pain: risk factors and prevention. Lancet 367:1618–1625
Kehlet H (2008) Chronic pain after groin hernia repair. Br J Surg 95:135–136
Ferzli GS, Edwards E, Al-Khoury G, Hardin R (2008) Postherniorrhaphy groin pain and how to avoid it. Surg Clin North Am 88:203-xi
Aasvang EK, Brandsborg B, Jensen TS, Kehlet H (2010) Heterogeneous sensory processing in persistent postherniotomy pain. Pain 150:237–242
Reinpold WM, Nehls J, Eggert A (2011) Nerve management and chronic pain after open inguinal hernia repair: a prospective two phase study. Ann Surg 254:163–168
Smeds S, Lofstrom L, Eriksson O (2010) Influence of nerve identification and the resection of nerves ‘at risk’ on postoperative pain in open inguinal hernia repair. Hernia 14:265–270
Alfieri S, Rotondi F, Di GA et al (2006) Influence of preservation versus division of ilioinguinal, iliohypogastric, and genital nerves during open mesh herniorrhaphy: prospective multicentric study of chronic pain. Ann Surg 243:553–558
Wijsmuller AR, van Veen RN, Bosch JL et al (2007) Nerve management during open hernia repair. Br J Surg 94:17–22
Langeveld HR, van’t Riet M, Weidema WF et al (2010) Total extraperitoneal inguinal hernia repair compared with Lichtenstein (the LEVEL-Trial): a randomized controlled trial. Ann Surg 251:819–824
McCarthy M Jr, Jonasson O, Chang CH et al (2005) Assessment of patient functional status after surgery. J Am Coll Surg 201:171–178
Aasvang EK, Gmaehle E, Hansen JB et al (2010) Predictive risk factors for persistent postherniotomy pain. Anesthesiology 112:957–969
Amid PK (2004) Lichtenstein tension-free hernioplasty: its inception, evolution, and principles. Hernia 8:1–7
Breivik H, Borchgrevink PC, Allen SM et al (2008) Assessment of pain. Br J Anaesth 101:17–24
Alfieri S, Amid PK, Campanelli G et al (2011) International guidelines for prevention and management of post-operative chronic pain following inguinal hernia surgery. Hernia 15:239–249
Lange JF, Wijsmuller AR, van Geldere D (2009) Feasibility study of three-nerve-recognizing Lichtenstein procedure for inguinal hernia. Br J Surg 96:1210–1214
Ndiaye A, Diop M, Ndoye JM et al (2007) Anatomical basis of neuropathies and damage to the ilioinguinal nerve during repairs of groin hernias. (about 100 dissections). Surg Radiol Anat 29:675–681
Wijsmuller AR, Lange JF, Kleinrensink GJ et al (2007) Nerve-identifying inguinal hernia repair: a surgical anatomical study. World J Surg 31:414–420
Rab M, Ebmer AJ, Dellon AL (2001) Anatomic variability of the ilioinguinal and genitofemoral nerve: implications for the treatment of groin pain. Plast Reconstr Surg 108:1618–1623
Klaassen Z, Marshall E, Tubbs RS, Louis RG Jr, Wartmann CT, Loukas M (2011) Anatomy of the ilioinguinal and iliohypogastric nerves with observations of their spinal nerve contributions. Clin Anat 24:454–461
Malekpour F, Mirhashemi SH, Hajinasrolah E, Salehi N, Khoshkar A, Kolahi AA (2008) Ilioinguinal nerve excision in open mesh repair of inguinal hernia–results of a randomized clinical trial: simple solution for a difficult problem? Am J Surg 195:735–740
Bartlett DC, Porter C, Kingsnorth AN (2007) A pragmatic approach to cutaneous nerve division during open inguinal hernia repair. Hernia 11:243–246
Akita K, Niga S, Yamato Y, Muneta T, Sato T (1999) Anatomic basis of chronic groin pain with special reference to sports hernia. Surg Radiol Anat 21:1–5
Acknowledgments
The research leading to these results is part of the Europain Collaboration, which has received support from the Innovative Medicines Initiative Joint Undertaking, under grant agreement no 115007, resources of which are composed of financial contribution from the European Union's Seventh Framework Programme (FP7/2007-2013) and EFPIA companies’ in kind contribution. The study was also supported by a grant from the Lundbeck Foundation.
Conflict of interest
None declared.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Bischoff, J.M., Aasvang, E.K., Kehlet, H. et al. Does nerve identification during open inguinal herniorrhaphy reduce the risk of nerve damage and persistent pain?. Hernia 16, 573–577 (2012). https://doi.org/10.1007/s10029-012-0946-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10029-012-0946-x