Abstract
This article categorizes four kinds of adverse effects to human health caused by ecosystem change: direct, mediated, modulated, and systems failure. The effects are categorized on their scale, complexity, and lag-time. Some but not all of these can be classified as resulting from reduced ecosystem services. The articles also explores the impacts that different socioeconomic–ecologic scenarios are likely to have on human health and how changes to human health may, in turn, influence the unfolding of four different plausible future scenarios. We provide examples to show that our categorization is a useful taxonomy for understanding the complex relationships between ecosystems and human well-being and for predicting how future ecosystem changes may affect human health.
Similar content being viewed by others
INTRODUCTION
The interconnection between ecosystems and human activity is complex, important, and poorly understood. Ecosystems support human health and well-being through their provisioning, regulating, cultural, and supporting services (Butler and others 2003). Shortages of food, fiber, and other ecosystem products adversely affect human health via many direct and indirect pathways. The regulating functions of ecosystems that affect health include the purification of air and fresh water, the reduction of flooding and drought, and range limitation of certain vector-borne diseases. Ecosystems also impact mental well-being through provision of cultural services, for example by providing totemic species and sacred groves, landscapes, and water bodies. These influence the aesthetic, recreational, educational, cultural, and spiritual aspects of the human experience. Ecosystem changes have also altered the epidemiology of communicable and noncommunicable diseases, including through some pathways that would not be considered as arising from a reduced ecosystem regulating service.
This article explores the impact that different plausible future scenarios (Cumming and others 2005; Raskin 2005) may have on health, and it also suggests how changes to health may feedback on and hence modify the course of the future. In doing so, we have categorized the effects of ecosystem change on human health into a useful taxonomy which can help predict which future ecosystem changes will impact human health and how. Although positive scenarios are conceivable, in this article we are mainly concerned with how adverse ecosystem changes and reduced ecosystem services may harm future human health.
Until the very recent past, most human induced ecological changes have had favorable effects on human society and health. Human health, judged by average life expectancy, has increased substantially, as has population size (Riley, 2001; Tuljapurkar and others 2000). The reasons for these increases are well-known and include the mutually reinforcing and interacting elements of improved knowledge, technology, and social organization, including of public health (Horiuchi 2000; Szreter 1999). A fundamental contributory factor has been the increased human capacity to modify ecosystems, for example, by increasing food supplies, by restricting populations of large carnivores, and by providing more fiber for fuel and shelter.
This success is not unqualified. Some adverse effects of our increased capacity to modify ecosystems on human health can already be seen. The transformation of ecosystems to provide certain benefits has reduced the scale and integrity of many ecosystems (Pimentel and others 2000). Reduced ecosystem integrity decreases their ability to provide some ecosystem services, which can, in turn, have negative impacts on human health. This relationship is unlikely to be linear and may contain thresholds beyond which incremental loss of ecosystem services has a disproportionately negative effect on human-health and well-being.
Examples of the negative impacts of ecosystem change on human health abound. National life expectancy has fallen in several countries, including many parts of sub-Saharan Africa, Haiti, Russia, North Korea, and Ethiopia (Farmer and others 2003; Shkolnikov and others 2001; United Nations Population Divisional 1999). Reduced ecosystem services may explain a part of these declines in national life expectancy and thus may be an underrecognized factor in the slowed rate of increase in global life expectancy. The problems of decreased provision of ecosystem services are often unequally distributed, with the majority of the burden falling on the poor. Additionally, poor populations frequently lack the income and other means to substitute or partly compensate for reduced ecosystem services (for example, by boiling microbiologically contaminated water).
In addition to the effect of ecosystem services on human health, human health itself influences access to critical ecosystem services and can modify the environmental impacts of human populations. For example, the AIDS epidemic in sub-Saharan Africa has reduced the provisioning ecosystem service of food supply (de Waal and Whiteside 2003). The high prevalence of yellow fever and malaria delayed the construction of the Panama Canal, and sleeping sickness still limits human settlement and thereby affects human access to ecosystem services in parts of central Africa (Bhalla 2002).
CATEGORIZATION OF CHANGED ECOSYSTEM SERVICES AND ADVERSE HEALTH EFFECTS
A major challenge in this field is to apply real world data to conceptual models (Miranda and others 2002), to validate the models, and to develop approaches that can serve as a vehicle for generating hypothesis-driven research. Although realization of these goals remains distant, the conceptual frameworks which will stimulate data acquisition and analysis in this field are developing (Butler and others, 2003). Figure 1 shows one such framework, linking natural and social systems with human well-being, of which health is an important component.
A conceptual model for integrating natural and social systems with human well-being. (adapted from Miranda and others, 2002)
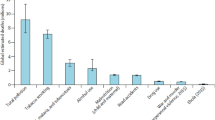
Here we introduce four categories of adverse effects on human health due to ecosystem change as a means to help understand the impacts of the different ecological scenarios on human health and well-being. In ascending order of scale, complexity, and lag-time, we call these adverse effects direct, mediated, modulated, and systems failure (see Table 1). We emphasize that, at their margins, these categories overlap because drivers may differ on temporal and spatial scales. Figure 2 graphically presents these concepts and provides a preliminary attempt to approximate the quantitative impact of the different categories.
Characteristics of four kinds of adverse health effects due to changes in ecosystem services. DALYs (Disability Adjusted Life Years lost) (Murray and Lopez 1997) are a commonly used measure of health impact. Unlike life expectancy, DALYs attempt to also reflect illness. Chronic illnesses that persist for many years are particularly high sources of lost DALYs (Murray and Lopez 1997).
Direct Effects
Direct (adverse) health effects are manifested through the immediate impacts of the loss of a useful ecosystem service, such as the provision of sufficient food, clean water, fertile soil or the restriction of erosion and flooding. Direct effects occur as the result of physical factors but do not include pathogens per se.
Climate change has recently been recognized as causing a substantial change in the Lake Tanganyika ecosystem. The fish catch has decreased due to a climate-related reduction in the nutrient supply (O’Reilly and others 2003). This reduction in ecosystem services places additional economic and nutritional stresses on an already poor and vulnerable human population. Although data to measure the health effect of this reduced catch are unlikely to be available, the effect is probably adverse because it causes reduced income and reduced nutrition (Verschuren 2003). Another example is the collapse of cod fishing in the North Atlantic, which caused widespread unemployment, mental distress, and social dislocation, but little if any true under nutrition because the social mechanisms operating in Canada were able to partially substitute for the lost provisioning services once supplied by the fishery. A third example of a direct health effect from a reduced ecosystem service is the disruption and physical injury caused by flooding. There is increasing recognition that floods are caused by the interaction of climatic and land-use changes (Hellin and others, 1999; Zhang and others, 2000). There is also increasing evidence that mental and physical health is enhanced by contact with nature (Friedman and Thomas 1995). Reduction of the cultural services that ecosystems provide is likely to contribute to the already enormous burden of disease caused by impaired mental health.
Mediated Effects
Compared to direct effects, mediated effects have increased causal complexity and, in some cases, involve pathogens. Some mediated effects have the potential for high rates of illness and death. There is also often a longer lag between the ecosystem change and the health outcome than for direct effects. However, by definition, mediated effects are insufficient in scale to cause the larger-scaled social collapse that we define as a modulated effect.
Many infectious and some chronic diseases fall in this category. The epidemiology of many communicable diseases is related to ecological factors. Some major nonvector-borne diseases, including tuberculosis, measles, and influenza, are thought to have crossed into human populations because of close contact with domesticated animals (McNeil 1976; Daszak and others, 2000; Oxford and others, 2002). Changes to biodiversity may be associated with increased numbers of disease-transmitting insects. Although contested, there are suggestions that malaria may also have become a significant human disease following the development of agriculture (Pennisi 2002; Joy and others 2003).
More recently, variant Creutzfeld–Jacob disease, Nipah virus, and Hendra virus illustrate novel infectious diseases that have entered human populations because of changed and more intensive animal feeding and farming practices (Waltner–Toews and Lang 2000). The emergence of Nipah virus may also have been related to bats fleeing from the intense drought and El Niño-related fires in Indonesia (Epstein and others, 2003). The long list of other infectious diseases related to ecosystem change (Patz and others, 2000) includes schistosomiasis (Li and others, 2000), cholera (Pascual and others, 2000), and Lyme disease (Jones and others, 1998; Blockstein 2000).
In many of these cases, the disease has emerged as a result of increased food-producing capacity of ecosystems—a provisioning ecosystem service—for example, by animal domestication, irrigation, dams, and other intensive farming practices. A tradeoff has been the unforeseen increase in the incidence and prevalence of many of these communicable diseases.
Some mediated health effects have also led to migration, while others have prevented the colonization of certain areas. For example, malaria has long restricted human settlement in lowland areas, including the Terai in Nepal, and many parts of equatorial Africa.
Some chronic, noninfectious diseases can also be classified as mediated effects of ecosystem change, including allergies, asthma, and some forms of cancer and chronic lung disease. For example, lung cancer and pulmonary fibrosis have become particularly common in the region around the shrunken Aral Sea, as pesticide-contaminated dust from this human-made desert is inhaled (O’Hara and others 2000). Both long-distance dust transport and more localized air pollution are also related to ecosystem service change and have been linked with a number of diseases, including asthma and atopy (Monteil 2002). There is also increasing evidence that air pollution, often exacerbated by ecosystem change such as land clearing and fires, may aggravate heart disease (Pyne 2002). Future ecosystem change, such as desertification, leading to a decrease in the ecosystem provisioning service of clean air, could thus alter the epidemiology of these diseases.
These diseases are classified as mediated rather than direct because their connection to changed ecosystems is more complex than are direct effects. Direct and mediated health effects are analogous to the direct and indirect health effects of climate change. In that classification, direct (adverse) health effects include phenomena such as heat stroke, while indirect effects include changes to certain vector-borne diseases because of altered patterns of temperature, humidity, and rainfall, and other effects secondary to extreme weather and adverse economic effects.
It is possible that a novel emerging disease could escape from a remote ecosystem to enter the wider human population, as the plague and HIV probably did. However, at least in the case of HIV, its really major (modulated) impact depended on powerful social cofactors, including severe poverty, social practices and taboos, and poor governance (Butler 2000a, 2000b). The ecological factors that underlie the recent SARS outbreak remain unclear (Enserink and Normile 2003), but its origin and amplification in a region of China, characterized by extremely dense populations of humans and domesticated animals and by poor public health services (Anonymous 2003), is consistent with the view that human-dominated ecosystems today harbor more danger to population health than does the “wild” (Oxford and others 2002). A plausible example of this principle could be the widespread transmission of multi-or even omni drug-resistant tuberculosis emerging from a prison (Tanne 1999; Dye and others, 2002). This scenario would have severe economic implications, especially for aviation and other industries perceived as increasing the probability of disease spread.
Modulated Effects
We also identify a larger-scale, more lagged, and more causally complex adverse consequence of adverse ecosystem change, than either direct or mediated effects, which we call a modulated or tertiary effect (Figure 2). These effects include episodes of state failure, or of nascent or realized large-scale social and economic collapse.
The role of environmental factors in the causation of large-scale conflicts, state failure, and social collapse is controversial (Deudney 1991; Gleick 1991; Homer-Dixon 1994; Uvin 1996; Cramer 2002). We agree that causation for the phenomena is complex, but we assert that reduced ecosystem services and other adverse ecosystem changes are frequently a component of the causal webs that lead to these phenomena (Butler and others 2003). This may be of increasing significance in the near future as evidence accrues that ecosystems are being changed more frequently and at larger scales.
There is compelling evidence that reduced ecosystem services were a causal factor for several large-scale social collapses and catastrophes, from both archeological sources (Weiss and Bradley 2001) and more recent history. Two ancient cases are the collapse of the ancient Mesopotamian and the Mayan civilizations, contributed to, respectively, by increased salinity (Jacobsen and Adams 1958) and drought (Haug and others 2003). Two more recent examples are the Irish famine of the 1840s and the Rwandan genocide in 1994. The Irish famine was caused by the spread of a potato fungus (Wilson 1995) interacting with a refusal by the British government to supply an effective substitute, such as famine relief (Sen 2000, pp 170–5). The Rwandan genocide also occurred as a result of the interaction of multiple factors, including poor governance, long-standing ethnic hatred, and rapid population growth. The violence was inflicted mainly by a large number of unemployed young men (Mesquida and Weiner 1996; Potts 1999), displaced from a livelihood in farming because of the shortage of fertile arable land, thus losing a key ecosystem service (André and Platteau 1998; Butler-2000a).
In these examples adverse health effects are likely to be larger than those from mediated effects, although in some cases state failure may be limited to small populations, such as for the people of Easter Island or the Norse in medieval Greenland.
Inevitably, ecosystem service changes that contribute to modulated effects will be embedded in a mosaic of social, economic, and political cofactors. In turn, many of these cofactors are likely to have at least partial ecosystem change-dependent causation. Depending on the knowledge, bias, and experience of the observer, the causal role of ecological factors in state failure may sometimes be underestimated, or even totally denied. For example, Rotberg (2002) identifies the roots of state failure as based in ethnic, religious, linguistic, or other intercommunal enmity. He argues that state failure is “man-made, not merely accidental nor—fundamentally—caused geographically, environmentally, or externally.” We do not claim that reduced ecosystem services or other ecosystem changes that lead to adverse health effects are always a “fundamental” factor in state failure, but they are often important and usually identifiable. The enmity that Rotberg refers to often arises over the distribution of diminishing per capita ecosystem services. There may be increasing recognition of this. For example, O’Reilly and others (2003) concludes, in discussing the potential for further reduction in the ecosystem provisioning service of Lake Tanganyika, that “the human implications of such subtle, but progressive, environmental changes are potentially dire in this densely populated region of the world, where large lakes are essential natural resources for regional economies.”
Ecosystem services as a significant element in state failure may be underrecognized due to our tendency to discount the future possibility of thresholds or emergence. Thresholds refer to sudden, nonlinear changes that result from a small increment and that are not intuitively predictable without prior experience (Alley and others 2003; Waldrop 1992; May 1999). Emergence refers to the new property that becomes apparent beyond the threshold. Modulated and systems failure effects (described below) are emergent phenomena that become apparent when linked socioecological systems pass a threshold, caused by the interaction of numerous social, political, and ecological elements.
Systems Failure
We also describe an even larger scale phenomenon than state failure, as a result of coalescing, interacting modulated effects. We call this phenomenon “systems failure.” The increasing connections that insulate diverse human communities from scarcity also create large-scale vulnerabilities, magnifiable by feedbacks such as collapsed global trade, terrorism, technological breakdown, and radiating failure of institutions and governance. Collapse could occur on a regional, continental, or even global scale. It is also possible, however, that a reverse state, “systems success,” could occur.
Large-scale epidemics exacerbated by chronic food insecurity, poor governance, and wide-scale conflict are plausible elements of this pathway. Drug-resistant bacteria, in part driven by the excessive use of antibiotics in animal husbandry, could contribute to this, as could the emergence of new viruses. However, we stress that novel infectious agents are unlikely to lead to modulated or systems failure effects without significant cofactors. Only modulated and systems failure effects are likely to be of sufficient scale to alter the unfolding of the various ecological and socioeconomic scenarios that are described elsewhere in this issue of Ecosystems.
SCENARIOS AND HEALTH
Cumming and others (2005) and Raskin (2005, this issue) review several socioecological scenarios that may unfold over this century. Although all plausible futures are influenced by the same driving forces, these forces evolve in different ways in the different scenarios. Demographic, economic, political, cultural, and social factors — including health — are codependent so that each factor will continually influence other factors. Each scenario will influence and be influenced by ecological factors as well. Just as in the past, the future world will contain a mixture of familiar and novel situations. Scenarios seek to coalesce these myriad possibilities into a limited number of theme futures that have strongly plausible elements.
Although there are dozens of names for the existing environmental scenarios, most can be categorized into a surprisingly small group of core pathways, as described by Cumming and others (this issue). The names of the four scenarios considered in this article are market forces, reformed market, value change, and higher fences (see Table 2). It is difficult to succinctly describe these scenarios, but a number of axes can be identified along which they vary. For example, there is a spectrum identifiable between comparative economic deregulation (market forces) to a neo-Keynesian model, here called reformed market. Another spectrum can be identified between a concerted attempt to protect existing ecosystem services (the “value change” scenario) and a laissez faire approach to ecosystems and the nonliving environment, such as climate change (the “market forces” scenario). A third spectrum is identifiable between trade deregulation (“reformed market”) and continuing or even increased protectionism (“higher fences”). As well, the trend of global income distribution can be predicted from these scenarios, from a continuing increase (“higher fences”) to a marked decrease (“reformed market” and “value change”).
The state of health for high- and low-income populations can be predicted, largely consequent to the anticipated change in income for each group. Three of these scenarios, as very briefly described, are essentially optimistic, because they all assume an increase in income for high- and low-income populations. However, in the higher-fences world, it is conceivable that incomes will decline for populations that currently have a low income, and the increased global inequality in this scenario could exacerbate tensions between low and income populations.
Cumming and others (2005) examine the assumptions made about ecosystem resilience in each of four scenarios and find that the outcome of different scenarios is influenced by this resilience. Table 2 lists some key terms concerning health for both high- and low-income populations in these four scenarios. It also shows our estimation of the probability of changes in the “health gap,” that is, the gap between high- and low-income populations with respect to health. At present, for example, the burden of disease from diarrhea (of which nearly 90% can be attributed to unsafe water, poor sanitation, and hygiene) is over 100 times higher in the least developed countries than in developed ones. The health gaps between high- and low-income populations have been systematically estimated using a measure called “disability adjusted life years” which accounts for total years of life lost because of disease and also for partial years of life lost because of disability (World Health Report 2002).
It is likely that in three of the four scenarios the health gap will decrease. This is because three of these scenarios assume gradual socioeconomic convergence between populations that are currently rich and poor. These scenarios postulate continued advances in science, technology, and the dissemination of information and expertise.
The response to the SARS outbreak illustrates the potential for a coordinated response to events that are perceived as sufficiently threatening. If convergence between rich and poor populations occurs, then coordinated responses to numerous health problems that continue to affect poor populations are likely. Advances could improve new vaccines, attention to “orphan” diseases, and distribution of the improved seeds and agricultural techniques needed to enhance food security.
In these scenarios the health of high-income populations is also likely to improve, though not as rapidly as for low-income populations. In only one scenario — called “barbarization” (Raskin, this issue) or “higher fences” (Cumming and others, this issue) — is the health gap likely to increase. In this scenario, poor populations are increasingly ignored by the remaining population. Food security of the poor is likely to further diminish, perhaps leading to positive feedbacks as malnutrition impairs cognitive development and further hinders education and the chance of skillful social and political responses. In this scenario the health of high-income populations is unlikely to be ideal: we identify obesity, diabetes, and anxiety as likely to increase, with their negative effects only partially countered by improved medical technology.
Modulated effects could sabotage even optimistic scenarios. Table 3 provides an estimation of the chance of systems failure, depending on assumptions concerning the resilience of ecosystems and the linked socioeconomic system. Cumming and others (2005) have defined ecosystem resilience as the capacity to absorb anthropogenic impacts without the loss of essential structure or functions. We suggest that it is meaningful to assume that human populations are characterized by social resilience, which modifies their capacity to effectively deal with stress (Carpenter and others 2001). From a public health perspective, resilience may be defined as the capacity of society to respond to problems and challenges, over the short and long term, in ways that protect and advance public health, over the short and long term. Affluence, education, social cooperation, technological capability, and flexibility are important determinants of the size of social buffers and human resilience. We suggest that systems failure effects are more likely to occur in the market-forces and higher-fences scenarios, because inequality between high- and low-income populations is likely to be the greatest in these scenarios.
The most optimistic future for human health is likely to be if both ecological and social systems prove highly resilient. In this case both major ecosystem and social services are likely to be preserved even if ecosystem changes (currently perceived by many as adverse) continue to occur at a high rate. On the other hand, the chance of further modulated or even systems failure effects occurring is increased if ecosystem and social systems prove to be brittle. Because the size of ecosystem service buffers is falling and the extent of ecosystem service resilience is uncertain, it is prudent to reduce further ecosystem damage as rapidly as possible. However, it is also prudent to conduct this in a way that minimizes harm to human health.
Continuing tradeoffs are likely to be required. For example, improving the health of populations in Indonesia may require further clearing of forests to generate more income. But this process cannot be continued indefinitely. On the other hand, excessively strict protection of the surviving ecosystems could reduce the size of the socioeconomic buffer, thus perhaps increasing the long-term risk of a modulated effect. In reality, economic and social forces make an extremely rapid transition to full protection of surviving ecosystems unlikely, but it may be just as risky to delay protection in response to only short-term socioeconomic concerns.
CONCLUSION
The causal relationship between ecosystem service change and impact upon human health remains incompletely understood. We have explored how ecosystem services impact human health and have proposed that adverse ecological changes can interact and feedback with dysfunctional social responses, leading to the development of states that we have termed mediated and systems failure. We have grouped the myriad possible interactions and cascading responses between ecosystem services and public health into four categories, a previously undescribed taxonomy which might help us better comprehend how ecosystem change and human health interact to affect the way the future unfolds.
We believe that this is an important conceptual advance that will be useful for understanding the relationship between human health and changes in ecosystem services. Continued analysis of cases studies, using both quantitative and qualitative methods, will advance our understanding of these relationships. Several regions of the world, characterized by substantial ecological and social stresses, may be useful “natural laboratories” for this purpose, including sub-Saharan Africa, Indonesia, and Northern India.
Direct and mediated effects, although they may lead to some important changes to the path of the future, are unlikely to seriously compromise the development of regional or global civilization. Despite occasional and localized setbacks, human health is likely to generally improve if future ecosystem changes result only in events such as occasional flooding, periodic disease outbreaks, and episodes of air pollution.
On the other hand, modulated and systems failure effects, if they occur, have the power to alter the course of society in significant ways. If negative this will cause substantial harm to human health and well-being, and, by exacerbating poor governance, could also further erode ecosystem services. Such events could derail even the most optimistic scenario. However, we do not deny the chance that positive systems effects could emerge, especially if ecosystem and social resilience remain high.
Current trends toward an increasingly large environmental footprint, further climate change, depletion of fossil fuels, and the erosion of existing ecological and social buffers are disturbing and unlikely to be sustainable (McMichael 2001). On the other hand, the increasing capacity to conceptualize, diagnose, and modify the global environment gives hope that humanity will self-organize in ways that can sustain both its social and ecological functions (Crutzen 2002).
References
RB Alley J Marotzke WD Nordhaus JT Overpeck DM Peteet RA Pielke RT Pierrehumbert PB Rhines TF Stocker LD Talley JM Wallace (2003) ArticleTitleAbrupt climate change Science 299 2005–10 Occurrence Handle10.1126/science.1081056 Occurrence Handle12663908
C André JP Platteau (1998) ArticleTitleLand relations under unbearable stress: Rwanda caught in the Malthusian trap J Econ Behav Org 34 1–47 Occurrence Handle10.1016/S0167-2681(97)00045-0
InstitutionalAuthorNameAnonymous (2003) ArticleTitleEmerging stronger from the China crisis [editorial] Lancet 361 1311
N Bhalla (2002) ArticleTitlePan African group takes lead against the tsetse fly Lancet 359 686 Occurrence Handle10.1016/S0140-6736(02)07843-1 Occurrence Handle11879881
DE Blockstein (1998) ArticleTitleLyme disease and the passenger pigeon? Science 279 1831 Occurrence Handle10.1126/science.279.5358.1831c Occurrence Handle9537894
CD Butler (2000a) ArticleTitleEntrapment: global ecological and/or local demographic? Reflections upon reading the BMJ’s “six billion day” special issue Ecosyst Health 6 171–80 Occurrence Handle10.1046/j.1526-0992.2000.006003171.x
CD Butler (2000b) ArticleTitleHIV and AIDS, poverty, and causation Lancet 356 1445–6 Occurrence Handle10.1016/S0140-6736(05)74091-5
CD Butler R Chambers K Chopra P Dasgupta A Duraiappah P Kumar AJ McMichael N Wen-Yuan (2003) Ecosystems and human well-being Ecosystems and Human Well-being. A Framework for Assessment: A framework for Assessment. Millennium Ecosystem Assessment Island Press Washington DC 71–84
S Carpenter B Walker JM Anderies N Abel (2001) ArticleTitleFrom metaphor to measurement: resilience of what to what? Ecosystems 4 765–81 Occurrence Handle10.1007/s10021-001-0045-9
C Cramer (2002) ArticleTitleHomo Economicus goes to war: methodological individualism, rational choice and the political economy of war World Dev 30 1845–64 Occurrence Handle10.1016/S0305-750X(02)00120-1
PJ Crutzen (2002) ArticleTitleGeology of mankind Nature 415 23 Occurrence Handle10.1038/415023a Occurrence Handle11780095
G Cumming J Alcamo O Sala R Swart EM Bennett M Zurek (2005) ArticleTitleAre existing global scenarios consistent with ecological feedbacks? Ecosystems 8 XXX–XXX
P Daszak AA Cunningham AD Hyatt (2000) ArticleTitleInfectious diseases of wildlife—threats to biodiversity and human health Science 287 443–9 Occurrence Handle10.1126/science.287.5452.443 Occurrence Handle10642539
A Waal Particlede A Whiteside (2003) ArticleTitleNew variant famine: AIDS and food crisis in southern Africa Lancet 362 1234–7 Occurrence Handle10.1016/S0140-6736(03)14548-5 Occurrence Handle14568749
D Deudney (1991) ArticleTitleEnvironment and security: Muddled thinking Bull At Sci 47 22–9
C Dye BG Williams MA Espinal MC Raviglione (2002) ArticleTitleErasing the world’s slow stain: strategies to beat multidrug-resistant tuberculosis Science 295 2042–6 Occurrence Handle10.1126/science.1063814 Occurrence Handle11896268
M Enserink D Normile (2003) ArticleTitleSearch for SARS origins stalls Science 302 706–7
PR Epstein E Chivian K Frith (2003) ArticleTitleConservation: our health depends on it [editorial] Emerging diseases threaten conservation Environ Health Perspect 111 IssueID10 A506–7 Occurrence Handle12896863
P Farmer MCS Fawzi P Nevil (2003) ArticleTitleUnjust embargo of aid for Haiti Lancet 361 420–2 Occurrence Handle10.1016/S0140-6736(03)12380-X Occurrence Handle12573389
E Friedman SA Thomas (1995) ArticleTitlePet ownership, social support, and one-year survival after acute myocardial infarction in the cardiac arrhythmia suppression trial (CAST) Am Cardiol 76 1213–7 Occurrence Handle10.1016/S0002-9149(99)80343-9
PH Gleick (1991) ArticleTitleEnvironment and security: The clear connections Bull At Sci 47 16–22
GH Haug D Günther LC Peterson DM Sigman KA Hughen B Aeschlimann (2003) ArticleTitleClimate and the collapse of Maya civilization Science 299 1731–5 Occurrence Handle10.1126/science.1080444 Occurrence Handle12637744
J Hellin M Haigh F Marks (1999) ArticleTitleRainfall characteristics of Hurricane Mitch Nature 399 316 Occurrence Handle10.1038/20577 Occurrence Handle10360570
TF Homer–Dixon (1994) ArticleTitleEnvironmental scarcities and violent conflict: evidence from cases Int Security 19 5–40
S Horiuchi (2000) ArticleTitleGreater lifetime expectations Nature 405 744–5 Occurrence Handle10.1038/35015642 Occurrence Handle10866180
T Jacobsen RM Adams (1958) ArticleTitleSalt and silt in ancient Mesopotamian agriculture Science 128 1251–8
CG Jones RS Ostfeld MP Richard EM Schauber JO Wolff (1998) ArticleTitleChain reactions linking acorns to gypsy moth outbreaks and Lyme disease risk Science 279 1023–6 Occurrence Handle10.1126/science.279.5353.1023 Occurrence Handle9461433
DA Joy X Feng J Mu T Furuya K Chotivanich AU Krettli M Ho A Wang NJ White E Suh P Beerli X Su (2003) ArticleTitleEarly origin and recent expansion of Plasmodium falciparum Science 300 318–21 Occurrence Handle10.1126/science.1081449 Occurrence Handle12690197
YS Li AC Sleigh AGP Ross GM Williams M Tanner DP McManus (2000) ArticleTitleEpidemiology of Schistosoma japonicum in China: Morbidity and strategies for control in the Dongting Lake region Int J Parasitol 30 273–81 Occurrence Handle10.1016/S0020-7519(99)00201-5 Occurrence Handle10719120
R May (1999) ArticleTitleHow the biosphere is organized Science 286 2091 Occurrence Handle10.1126/science.286.5447.2091
AJ McMichael (2001) Human Frontiers, Environments and Disease: Past Patterns, Uncertain Futures Cambridge University Press Cambridge
W McNeil (1976) Plagues and Peoples Anchor Press Garden City, NY
CG Mesquida NI Weiner (1996) ArticleTitleHuman collective aggression: a behavioral ecology perspective Ethol Sociobiol 17 247–62 Occurrence Handle10.1016/0162-3095(96)00035-0
ML Miranda P Mohai J Bus G Charnley EJ Dorward–King P Foster WR Munns (2002) Policy concepts and applications RT Di Giulio WH Benson (Eds) Interconnections Between Human Health and Ecological Integrity SETAC Pensacola, FL 15–41
MA Monteil (2002) ArticleTitleDust clouds and spread of infection Lancet 359 81–2 Occurrence Handle10.1016/S0140-6736(02)07303-8
Murray CL, Lopez AD. 1997. Alternative projections of mortality and disability by cause 1990–2020: Global Burden of Disease Study.349:148–54
SL O’Hara GFS Wiggs B Mamedov G Davidson RB Hubbard (2000) ArticleTitleExposure to airborne dust contaminated with pesticide in the Aral Sea region Lancet 355 627 Occurrence Handle10.1016/S0140-6736(99)04753-4 Occurrence Handle10696990
CM O’Reilly SR Alin P-D Plisnier AS Cohen BA McKee (2003) ArticleTitleClimate change decreases aquatic ecosystem productivity of Lake Tanganyika, Africa Nature 424 766–8 Occurrence Handle10.1038/nature01833 Occurrence Handle12917682
JS Oxford A Sefton R Jackson W Innes R Daniels N Johnson (2002) ArticleTitleWorld War I may have allowed the emergence of “Spanish” influenza Lancet Infect Dis 2 111–4 Occurrence Handle10.1016/S1473-3099(02)00185-8 Occurrence Handle11901642
M Pascual X Rodo SP Ellner R Colwell MJ Bouma (2000) ArticleTitleCholera dynamics and El Niño-Southern Oscillation Science 289 1766 Occurrence Handle10.1126/science.289.5485.1766 Occurrence Handle10976073
J Patz T Graczyk N Geller A Vittor (2000) ArticleTitleEffects of environmental change on emerging parasitic diseases Int J Parasitol 30 1395–405 Occurrence Handle10.1016/S0020-7519(00)00141-7 Occurrence Handle11113264
E Pennisi (2001) ArticleTitleMalaria’s beginnings: on the heels of hoes? Science 293 416–7 Occurrence Handle10.1126/science.293.5529.416 Occurrence Handle11463894
D Pimentel L Westra RF Noss (2000) Ecological Integrity: Integrating Environment, Conservation, and Health Island Press Washington DC
M Potts (1999) ArticleTitleThe population policy pendulum. Needs to settle near the middle and acknowledge the importance of numbers BMJ 319 933–93 Occurrence Handle10514138
S Pyne (2002) ArticleTitleSmall particles add up to big disease risk Science 295 1994 Occurrence Handle10.1126/science.295.5562.1994a
P Raskin (2005) ArticleTitleGlobal scenarios: Background Review for the Millennium Ecosystem Assessment Ecosystems 8 XXX–XXX
JC Riley (2001) Rising Life Expectancy: A Global History Cambridge University Press Cambridge
RI Rotberg (2002) ArticleTitleThe new nature of nation–state failure Wash Qu 25 85–96 Occurrence Handle10.1162/01636600260046253
A Sen (2000) Development as Freedom Oxford University Press New Delhi
V Shkolnikov M McKee DA Leon (2001) ArticleTitleChanges in life expectancy in Russia in the 1990s Lancet 357 917–21 Occurrence Handle10.1016/S0140-6736(00)04212-4 Occurrence Handle11289348
S Szreter (1999) ArticleTitleRapid economic growth and the four Ds of disruption, deprivation, disease and death: public health lessons from 19th-century Britain for 21st-century China? Trop Med Int Health 4 146–52 Occurrence Handle10.1046/j.1365-3156.1999.00369.x Occurrence Handle10206269
JH Tanne (1999) ArticleTitleDrug resistant TB is spreading worldwide BMJ 319 1220
S Tuljapurkar N Li C Boe (2000) ArticleTitleA universal pattern of mortality decline in the G7 countries Nature 405 789–92 Occurrence Handle10.1038/35015561 Occurrence Handle10866199
United Nations Population Division Department of Economic and Social Affairs. 1999. World Population Prospects: The 1998 Revision. The Demographic Impact of HIV/AIDS. New York: United Nations
P Uvin (1996) ArticleTitleTragedy in Rwanda: The political ecology of conflict Environment 38 7–15
D Verschuren (2003) ArticleTitleGlobal change: the heat on Lake Tanganyika Nature 424 731–2 Occurrence Handle10.1038/424731a Occurrence Handle12917665
MM Waldrop (1992) Complexity. The Emerging Science at the Edge of Order and Chaos Viking London
D Waltner–Toews T Lang (2000) ArticleTitleA new conceptual base for food and agricultural policy: the emerging model of links between agriculture, food, health, environ ment and society Global Change Hum Health 1 116–30 Occurrence Handle10.1023/A:1010025021186
H Weiss RS Bradley (2001) ArticleTitleWhat drives societal collapse? Science 291 609–10 Occurrence Handle10.1126/science.1058775 Occurrence Handle11158667
M Wilson (1995) ArticleTitleInfectious disease: an ecological perspective BMJ 311 1881–4
InstitutionalAuthorNameWorld Health Organization (2002) The World Health Report 2002 World Health Organization Geneva
P Zhang G Shao G Zhao DCL Master GR Parker JBD Dunning SuffixJr Q Li (2000) ArticleTitleChina’s forest policy for the 21st century Science 288 2135–6 Occurrence Handle10.1126/science.288.5474.2135 Occurrence Handle10896587
Acknowledgements
We thank the Millennium Ecosystem Assessment for providing many opportunities to discuss the main ideas expressed in this article with colleagues. We also thank Professor D. Crawford–Brown and two anonymous reviewers for their comments and suggestions.
Author information
Authors and Affiliations
Corresponding author
Additional information
Disclaimer:
The views expressed in this article are those of the authors and do not necessarily reflect the position of the World Health Organization. This article has been subjected to EPA review and approved for publication but does not necessarily reflect EPA policy.
Rights and permissions
About this article
Cite this article
Butler, C.D., Corvalan, C.F. & Koren, H.S. Human Health, Well-Being, and Global Ecological Scenarios. Ecosystems 8, 153–162 (2005). https://doi.org/10.1007/s10021-004-0076-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10021-004-0076-0