Abstract
Objectives
The aim was to compile the current knowledge about the efficacy of different soft tissue correction methods around osseointegrated, already uncovered and/or loaded (OU/L) implants with insufficient soft tissue conditions. Procedures to increase peri-implant keratinized mucosa (KM) width and/or soft tissue volume were considered.
Materials and methods
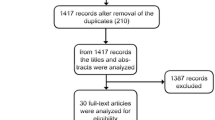
Screening of two databases: MEDLINE (PubMed) and EMBASE (OVID), and manual search of articles were performed. Human studies reporting on soft tissue augmentation/correction methods around OU/L implants up to June 30, 2016, were considered. Quality assessment of selected full-text articles to weight risk of bias was performed using the Cochrane collaboration’s tool.
Results
Overall, four randomized controlled trials (risk of bias = high/low) and five prospective studies (risk of bias = high) were included. Depending on the surgical techniques and graft materials, the enlargement of keratinized tissue (KT) ranged between 1.15 ± 0.81 and 2.57 ± 0.50 mm. The apically positioned partial thickness flap (APPTF), in combination with a free gingival graft (FGG), a subepithelial connective tissue graft (SCTG), or a xenogeneic graft material (XCM) were most effective. A coronally advanced flap (CAF) combined with SCTG in three, combined with allogenic graft materials (AMDA) in one, and a split thickness flap (STF) combined with SCTG in another study showed mean soft tissue recession coverage rates from 28 to 96.3 %. STF combined with XCM failed to improve peri-implant soft tissue coverage.
Conclusions
The three APPTF-techniques combined with FGG, SCTG, or XCM achieved comparable enlargements of peri-implant KT. Further, both STF and CAF, both in combination with SCTG, are equivalent regarding recession coverage rates. STF + XCM and CAF + AMDA did not reach significant coverage.
Clinical relevance
In case of soft tissue deficiency around OU/L dental implants, the selection of both an appropriate surgical technique and a suitable soft tissue graft material is of utmost clinical relevance.




Similar content being viewed by others
References
Agudio G, Nieri M, Rotundo R et al (2008) Free gingival grafts to increase keratinized tissue: a retrospective long-term evaluation (10 to 25 years) of outcomes. J Periodontol 79:587–594
Lang NP, Loe H (1972) The relationship between the width of keratinized gingiva and gingival health. J Periodontol 43:623–627
Miyasato M, Crigger M, Egelberg J (1977) Gingival condition in areas of minimal and appreciable width of keratinized gingiva. J Clin Periodontol 4:200–209
Kennedy JE, Bird WC, Palcanis KG et al (1985) A longitudinal evaluation of varying widths of attached gingiva. J Clin Periodontol 12:667–675
Wennstrom J (1983) Regeneration of gingiva following surgical excision. A clinical study 10:287–297
Wennstrom JL (1987) Lack of association between width of attached gingiva and development of soft tissue recession. A 5-year longitudinal study. J Clin Periodontol 14:181–184
Valderhaug J, Birkeland JM (1976) Periodontal conditions in patients 5 years following insertion of fixed prostheses. Pocket depth and loss of attachment. J Oral Rehabil 3:237–243
Bassetti M, Kaufmann R, Salvi GE et al (2015) Soft tissue grafting to improve the attached mucosa at dental implants: a review of the literature and proposal of a decision tree. Quintessence Int 46:499–510
Berglundh T, Lindhe J, Jonsson K et al (1994) The topography of the vascular systems in the periodontal and peri-implant tissues in the dog. J Clin Periodontol 21:189–193
Berglundh T, Lindhe J, Ericsson I et al (1991) The soft tissue barrier at implants and teeth. Clin Oral Implants Res 2:81–90
Listgarten MA, Lang NP, Schroeder HE et al (1991) Periodontal tissues and their counterparts around endosseous implants [corrected and republished with original paging, article orginally printed in Clin Oral Implants Res 1991 Jan-mar;2(1):1-19]. Clin Oral Implants Res 2:1–19
Moon IS, Berglundh T, Abrahamsson I et al (1999) The barrier between the keratinized mucosa and the dental implant. An experimental study in the dog. J Clin Periodontol 26:658–663
Ikeda H, Shiraiwa M, Yamaza T et al (2002) Difference in penetration of horseradish peroxidase tracer as a foreign substance into the peri-implant or junctional epithelium of rat gingivae. Clin Oral Implants Res 13:243–251
Karring T, Ostergaard E, Loe H (1971) Conservation of tissue specificity after heterotopic transplantation of gingiva and alveolar mucosa. J Periodontal Res 6:282–293
Zuhr O, Hürzeler M, editors (2011) Plastisch-ästhetische Parodontal- und Implantatchirurgie. Berlin: Quintessenz Verlag
Adell R, Lekholm U, Rockler B et al (1986) Marginal tissue reactions at osseointegrated titanium fixtures (I). A 3-year longitudinal prospective study. Int J Oral Maxillofac Surg 15:39–52
Bengazi F, Wennstrom JL, Lekholm U (1996) Recession of the soft tissue margin at oral implants. A 2-year longitudinal prospective study. Clin Oral Implants Res 7:303–310
Block MS, Gardiner D, Kent JN et al (1996) Hydroxyapatite-coated cylindrical implants in the posterior mandible: 10-year observations. Int J Oral Maxillofac Implants 11:626–633
Esposito M, Grusovin MG, Maghaireh H et al. (2007) Interventions for replacing missing teeth: management of soft tissues for dental implants. Cochrane Database Syst Rev:CD006697
Heitz-Mayfield LJ (2008) Peri-implant diseases: diagnosis and risk indicators. J Clin Periodontol 35:292–304
Lekholm U, Adell R, Lindhe J et al (1986) Marginal tissue reactions at osseointegrated titanium fixtures. (II) a cross-sectional retrospective study. Int J Oral Maxillofac Surg 15:53–61
Roos-Jansaker AM, Renvert H, Lindahl C et al (2006) Nine- to fourteen-year follow-up of implant treatment. Part III: factors associated with peri-implant lesions. J Clin Periodontol 33:296–301
Schou S, Holmstrup P, Hjorting-Hansen E et al (1992) Plaque-induced marginal tissue reactions of osseointegrated oral implants: a review of the literature. Clin Oral Implants Res 3:149–161
Strub JR, Gaberthuel TW, Grunder U (1991) The role of attached gingiva in the health of peri-implant tissue in dogs. 1. Clinical findings. Int J Periodontics Restorative Dent 11:317–333
Warrer K, Buser D, Lang NP et al (1995) Plaque-induced peri-implantitis in the presence or absence of keratinized mucosa. An experimental study in monkeys. Clin Oral Implants Res 6:131–138
Wennström JL, Bengazi F, Lekholm U (1994) The influence of the masticatory mucosa on the peri-implant soft tissue condition. Clin Oral Implants Res 5:1–8
Wennström JL, Derks J (2012) Is there a need for keratinized mucosa around implants to maintain health and tissue stability? Clin Oral Implants Res 23(Suppl 6):136–146
Zarb GA, Schmitt A (1990) The longitudinal clinical effectiveness of osseointegrated dental implants: the Toronto study. Part III: problems and complications encountered. J Prosthet Dent 64:185–194
Adibrad M, Shahabuei M, Sahabi M (2009) Significance of the width of keratinized mucosa on the health status of the supporting tissue around implants supporting overdentures. J Oral Implantol 35:232–237
Artzi Z, Carmeli G, Kozlovsky A (2006) A distinguishable observation between survival and success rate outcome of hydroxyapatite-coated implants in 5-10 years in function. Clin Oral Implants Res 17:85–93
Chung DM, Oh TJ, Shotwell JL et al (2006) Significance of keratinized mucosa in maintenance of dental implants with different surfaces. J Periodontol 77:1410–1420
Crespi R, Cappare P, Gherlone E (2010) A 4-year evaluation of the peri-implant parameters of immediately loaded implants placed in fresh extraction sockets. J Periodontol 81:1629–1634
Schrott AR, Jimenez M, Hwang JW et al (2009) Five-year evaluation of the influence of keratinized mucosa on peri-implant soft-tissue health and stability around implants supporting full-arch mandibular fixed prostheses. Clin Oral Implants Res 20:1170–1177
Bouri A Jr, Bissada N, Al-Zahrani MS et al (2008) Width of keratinized gingiva and the health status of the supporting tissues around dental implants. Int J Oral Maxillofac Implants 23:323–326
Boynuegri D, Nemli SK, Kasko YA (2013) Significance of keratinized mucosa around dental implants: a prospective comparative study. Clin Oral Implants Res 24:928–933
Malo P, Rigolizzo M, Nobre M et al (2013) Clinical outcomes in the presence and absence of keratinized mucosa in mandibular guided implant surgeries: a pilot study with a proposal for the modification of the technique. Quintessence Int 44:149–157
Zigdon H, Machtei EE (2008) The dimensions of keratinized mucosa around implants affect clinical and immunological parameters. Clin Oral Implants Res 19:387–392
Brito C, Tenenbaum HC, Wong BK et al (2014) Is keratinized mucosa indispensable to maintain peri-implant health? A systematic review of the literature. J Biomed Mater Res B Appl Biomater 102:643–650
Gobbato L, Avila-Ortiz G, Sohrabi K et al (2013) The effect of keratinized mucosa width on peri-implant health: a systematic review. Int J Oral Maxillofac Implants 28:1536–1545
Lin GH, Chan HL, Wang HL (2013) The significance of keratinized mucosa on implant health: a systematic review. J Periodontol 84(12):1755–1767
Zitzmann NU, Berglundh T, Marinello CP et al (2001) Experimental peri-implant mucositis in man. J Clin Periodontol 28:517–523
Hürzeler MB, Weng D (1996) Periimplant tissue management: optimal timing for an aesthetic result. Pract Periodontics Aesthet Dent 8:857–869 quiz 869
Shibli JA, d’avila S, Marcantonio E Jr (2004) Connective tissue graft to correct peri-implant soft tissue margin: a clinical report. J Prosthet Dent 91:119–122
Yan JJ, Tsai AY, Wong MY et al (2006) Comparison of acellular dermal graft and palatal autograft in the reconstruction of keratinized gingiva around dental implants: a case report. Int J Periodontics Restorative Dent 26:287–292
Bassetti RG, Stahli A, Bassetti MA et al (2016) Soft tissue augmentation procedures at second-stage surgery: a systematic review. Clin Oral Investig 20(7):1369–1387
Needleman IG (2002) A guide to systematic reviews. J Clin Periodontol 29(Suppl 3):6–9 discussion 37-38
Higgins JP, Altman DG, Gotzsche PC et al (2011) The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. Br Med J 343:d5928
Urban IA, Lozada JL, Nagy K et al (2015) Treatment of severe mucogingival defects with a combination of strip gingival grafts and a xenogeneic collagen matrix: a prospective case series study. Int J Periodontics Restorative Dent 35:345–353
Happe A, Stimmelmayr M, Schlee M et al (2013) Surgical management of peri-implant soft tissue color mismatch caused by shine-through effects of restorative materials: one-year follow-up. Int J Periodontics Restorative Dent 33:81–88
Issarayangkul C, Schoenbaum TR, McLaren EA (2013) Prosthetic soft tissue management following two periimplant graft failures: a clinical report. J Prosthet Dent 110:155–160
Zucchelli G, Mazzotti C, Mounssif I et al (2013) Esthetic treatment of peri-implant soft tissue defects: a case report of a modified surgical-prosthetic approach. The International journal of periodontics & restorative dentistry 33:327–335
Ponzoni D, Jardim EC, de Carvalho PS (2013) Vestibuloplasty by modified Kazanjian technique in treatment with dental implants. J Craniofac Surg 24:1373–1375
Froum SJ, Froum SH, Rosen PS (2012) Successful management of peri-implantitis with a regenerative approach: a consecutive series of 51 treated implants with 3- to 7.5-year follow-up. The International journal of periodontics & restorative dentistry 32:11–20
Mareque-Bueno S (2011) A novel surgical procedure for coronally repositioning of the buccal implant mucosa using acellular dermal matrix: a case report. J Periodontol 82:151–156
Lai YL, Chen HL, Chang LY et al (2010) Resubmergence technique for the management of soft tissue recession around an implant: case report. Int J Oral Maxillofac Implants 25:201–204
Sanz M, Lorenzo R, Aranda JJ et al (2009) Clinical evaluation of a new collagen matrix (Mucograft prototype) to enhance the width of keratinized tissue in patients with fixed prosthetic restorations: a randomized prospective clinical trial. J Clin Periodontol 36:868–876
Karl M, Fenner M, Amann K et al (2009) Interforaminal implant therapy using a split skin graft—treatment outcome after 13 years. Quintessence Int 40:191–194
Shibli JA, d’Avila S (2006) Restoration of the soft-tissue margin in single-tooth implant in the anterior maxilla. J Oral Implantol 32:286–290
Deppe H, Horch HH, Kolk A (2004) Microstructured dental implants and palatal mucosal grafts in cleft patients: a retrospective analysis. J Craniomaxillofac Surg 32:211–215
Maksoud MA (2003) Manipulation of the peri-implant tissue for better maintenance: a periodontal perspective. J Oral Implantol 29:120–123
El-Askary AS (2002) Use of connective tissue grafts to enhance the esthetic outcome of implant treatment: a clinical report of 2 patients. J Prosthet Dent 87:129–132
Mathews DP (2002) The pediculated connective tissue graft: a technique for improving unaesthetic implant restorations. Pract Proced Aesthet Dent 14:719–724 quiz 726
Deeb GR, Le BT, Ueeck BA et al (2001) Use of upper-lid blepharoplasty full-thickness skin for peri-implant keratinized tissue grafting: a report of 2 cases. J Oral Maxillofac Surg 59:1232–1235
Silverstein LH, Lefkove MD (1994b) The use of the subepithelial connective tissue graft to enhance both the aesthetics and periodontal contours surrounding dental implants. J Oral Implantol 20:135–138
Yilmaz S, Efeoglu E, Biskin T et al (1994) Widening the zone of peri-implant attached gingiva. J Marmara Univ Dent Fac 2:383–388
Campbell Z, Simons AM, Giordano JR (1993) Soft tissue grafting and vestibuloplasty technique in association with endosseous implants. J Mich Dent Assoc 75:26–29
Simons AM, Darany DG, Giordano JR (1993) The use of free gingival grafts in the treatment of peri-implant soft tissue complications: clinical report. Implant Dent 2:27–30
Buser D (1987) Vestibuloplasty with free mucosal grafts in implants in the edentulous mandible. Surgical method and preliminary results. Schweiz Monatsschr Zahnmed 97:766–772
Anderson LE, Inglehart MR, El-Kholy K et al (2014) Implant associated soft tissue defects in the anterior maxilla: a randomized control trial comparing subepithelial connective tissue graft and acellular dermal matrix allograft. Implant Dent 23:416–425
Basegmez C, Karabuda ZC, Demirel K et al (2013) The comparison of acellular dermal matrix allografts with free gingival grafts in the augmentation of peri-implant attached mucosa: a randomised controlled trial. European journal of oral implantology 6:145–152
Basegmez C, Ersanli S, Demirel K et al (2012) The comparison of two techniques to increase the amount of peri-implant attached mucosa: free gingival grafts versus vestibuloplasty. One-year results from a randomised controlled trial. Eur J Oral Implantol 5:139–145
Lorenzo R, Garcia V, Orsini M et al (2012) Clinical efficacy of a xenogeneic collagen matrix in augmenting keratinized mucosa around implants: a randomized controlled prospective clinical trial. Clin Oral Implants Res 23:316–324
Schallhorn RA, McClain PK, Charles A et al (2015) Evaluation of a porcine collagen matrix used to augment keratinized tissue and increase soft tissue thickness around existing dental implants. The International journal of periodontics & restorative dentistry 35:99–103
Roccuzzo M, Gaudioso L, Bunino M et al (2014) Surgical treatment of buccal soft tissue recessions around single implants: 1-year results from a prospective pilot study. Clin Oral Implants Res 25:641–646
Zucchelli G, Mazzotti C, Mounssif I et al (2013) A novel surgical-prosthetic approach for soft tissue dehiscence coverage around single implant. Clin Oral Implants Res 24:957–962
Burkhardt R, Joss A, Lang NP (2008) Soft tissue dehiscence coverage around endosseous implants: a prospective cohort study. Clin Oral Implants Res 19:451–457
Park JB (2006) Increasing the width of keratinized mucosa around endosseous implant using acellular dermal matrix allograft. Implant Dent 15:275–281
Karring T, Lang NP, Loe H (1975) The role of gingival connective tissue in determining epithelial differentiation. J Periodontal Res 10:1–11
Sculean A, Gruber R, Bosshardt DD (2014) Soft tissue wound healing around teeth and dental implants. J Clin Periodontol 41(Suppl 15):S6–22
Souza AB, Tormena M, Matarazzo F et al (2015) The influence of peri-implant keratinized mucosa on brushing discomfort and peri-implant tissue health. Clin Oral Implants Res 27(6):650–655
Puisys A, Linkevicius T (2015) The influence of mucosal tissue thickening on crestal bone stability around bone-level implants. A prospective controlled clinical trial. Clin Oral Implants Res 26:123–129
Linkevicius T, Puisys A, Linkeviciene L et al (2015) Crestal bone stability around implants with horizontally matching connection after soft tissue thickening: a prospective clinical trial. Clin Implant Dent Relat Res 17:497–508
Buyukozdemir Askin S, Berker E, Akincibay H et al (2015) Necessity of keratinized tissues for dental implants: a clinical, immunological, and radiographic study. Clin Implant Dent Relat Res 17:1–12
Costa FO, Takenaka-Martinez S, Cota LO et al (2012) Peri-implant disease in subjects with and without preventive maintenance: a 5-year follow-up. J Clin Periodontol 39:173–181
Linkevicius T, Apse P, Grybauskas S et al (2009) The influence of soft tissue thickness on crestal bone changes around implants: a 1-year prospective controlled clinical trial. Int J Oral Maxillofac Implants 24:712–719
Griffin TJ, Cheung WS, Zavras AI et al (2006) Postoperative complications following gingival augmentation procedures. J Periodontol 77:2070–2079
Schmitt CM, Moest T, Lutz R et al (2015) Long-term outcomes after vestibuloplasty with a porcine collagen matrix (Mucograft) versus the free gingival graft: a comparative prospective clinical trial. Clin Oral Implants Res 27(11):e125–e133
Mombelli A, van Oosten MA, Schurch E Jr et al (1987) The microbiota associated with successful or failing osseointegrated titanium implants. Oral Microbiol Immunol 2:145–151
Schmitt CM, Tudor C, Kiener K et al (2013) Vestibuloplasty: porcine collagen matrix versus free gingival graft: a clinical and histologic study. J Periodontol 84:914–923
Hürzeler MB, Weng D (1999) A single-incision technique to harvest subepithelial connective tissue grafts from the palate. The International journal of periodontics & restorative dentistry 19:279–287
Aroca S, Molnar B, Windisch P et al (2013) Treatment of multiple adjacent Miller class I and II gingival recessions with a modified coronally advanced tunnel (MCAT) technique and a collagen matrix or palatal connective tissue graft: a randomized, controlled clinical trial. J Clin Periodontol 40:713–720
Jung RE, Sailer I, Hammerle CH et al (2007) In vitro color changes of soft tissues caused by restorative materials. The International journal of periodontics & restorative dentistry 27:251–257
Jung RE, Holderegger C, Sailer I et al (2008) The effect of all-ceramic and porcelain-fused-to-metal restorations on marginal peri-implant soft tissue color: a randomized controlled clinical trial. Int J Periodontics Restorative Dent 28:357–365
Jung RE, Holderegger C, Sailer I et al (2008) The effect of all-ceramic and porcelain-fused-to-metal restorations on marginal peri-implant soft tissue color: a randomized controlled clinical trial. The International journal of periodontics & restorative dentistry 28:357–365
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Renzo Bassetti declares that he has no conflict of interest. Alexandra Stähli declares that she has no conflict of interest. Mario Bassetti declares that he has no conflict of interest. Anton Sculean declares that he has no conflict of interest.
Funding
This review article was supported by the authors’ own institutions (Department of Oral and Maxillofacial Surgery of the Lucerne Cantonal Hospital and Department of Periodontology of the University of Bern, Switzerland.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Informed consent
For this type of study, formal consent is not required.
Additional information
Renzo G. Bassetti and Alexandra Stähli contributed equally to the manuscript (split first)
Rights and permissions
About this article
Cite this article
Bassetti, R.G., Stähli, A., Bassetti, M.A. et al. Soft tissue augmentation around osseointegrated and uncovered dental implants: a systematic review. Clin Oral Invest 21, 53–70 (2017). https://doi.org/10.1007/s00784-016-2007-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-016-2007-9