Abstract
Objectives
The aim of this study was to conduct a comparative qualitative and quantitative assessment of the interfacial soft and hard tissues investing implants and natural teeth.
Materials and methods
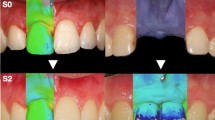
The test sample consisted of six adult healthy male Macaca fascicularis with three-unit splinted crowns, each crown supported by an Ankylos screw-shaped titanium implant. These implants were placed in the mandibular premolar-second molar region, one side by an immediate-loading (IL) and the other by delayed-loading (DL) protocol. The animals were sacrificed after 3 months of functional loading. Another two monkeys with natural dentition served as controls. Nondecalcified sections were prepared for assessment of optical intensities (OI) under a confocal laser scanning microscope.
Results
In both the test (IL and DL) and control, the soft tissue complexes demonstrated a highly fluorescent keratinized layer and diminished cytoplasmic and enhanced membranous fluorescence in the remaining epithelium. Peri-implant mucosa was further characterized by an intense fluorescence at the junctional epithelium-implant interface and in the stromal mononuclear infiltrate. Connective tissue contact and periodontal ligament were weakly fluorescent. In hard tissues, a high fluorescence was observed in peri-implant woven bone and along the implant-bone interface. Mean OI was significantly higher in peri-implant woven bone than around teeth (P < 0.05). In the remaining soft and hard tissue complexes, no significant differences in mean OI between the test and control were observed (P > 0.05).
Conclusions
Present findings suggest that peri-implant woven bone is highly mineralized, while the peri-implant and gingival mucosa share structural similarities.
Clinical relevance
Optical intensities of interfacial tissues investing implants and teeth are related to their biological properties.






Similar content being viewed by others
References
Berglundh T, Abrahamsson I, Welander M, Lang NP, Lindhe J (2007) Morphogenesis of the peri-implant mucosa: an experimental study in dogs. Clin Oral Implants Res 18:1–8
Hermann JS, Buser D, Schenk RK, Higginbottom FL, Cochran DL (2000) Biologic width around titanium implants. A physiologically formed and stable dimension over time. Clin Oral Implants Res 11:1–11
Yeung SCH (2008) Biological basis for soft tissue management in implant dentistry. Aust Dent J 53(Suppl 1):S39–S42
Abrahamsson I, Berglundh T, Glantz T, Lindhe J (1998) The mucosal attachment at different abutments. An experimental study in dogs. J Clin Periodontol 25:721–727
Abrahamsson I, Berglundh T, Moon IS, Lindhe J (1999) Peri-implant tissues at submerged and non-submerged titanium implants. J Clin Periodontol 26:600–607
Abrahamsson I, Zitzmann NU, Berglundh T, Linder E, Wennerberg A, Lindhe J (2002) The mucosal attachment to titanium implants with different surface characteristics: an experimental study in dog. J Clin Periodontol 29:448–455
Albrektsson T (2008) Hard tissue implant interface. Aust Dent J 53(Suppl 1):S34–S38
Marco F, Giavaresi G, Vittoria O (2005) Peri-implant osteogenesis in health and osteoporosis. Micron 36:630–644
Chang P-C, Lang NP, Giannobile WV (2010) Evaluation of functional dynamics during osseointegration and regeneration associated with oral implants. Clin Oral Implants Res 21:1–12
Rozé J, Babu S, Safarzadah A, Gayet-Delacroix M, Hoornaert A, Layrolle P (2009) Correlating implant stability to bone structure. Clin Oral Implants Res 20:1140–1145
O’ Sullivan D, Sennerby L, Meredith N (2004) Influence of implant taper on primary and secondary stability of osseointegrated titanium implants. Clin Oral Implants Res 15:474–480
Bacchelli B, Giavaresi G, Franchi M, Martini D, De Pasquale V, Trirè A, Fini M, Giardino R, Ruggeri A (2009) Influence of a zirconia sandblasting treated surface on peri-implant bone healing: An experimental study in sheep. Acta Biomater 5:2246–2257
Scarano A, Orsini G, Pecora G, Iezzi G, Perrotti V, Piattelli A (2007) Peri-implant bone regeneration with calcium sulfate: a light and transmission electron microscopy case report. Implant Dent 16:195–203
Liu S, Broucek J, Virdi AS, Sumner DR (2012) Limitations of using micro-computer tomography to predict bone-implant contact and mechanistic fixation. J Microsc 245:34–42
Bahat O, Sullivan RM (2010) Parameters for successful implant integration revisited part II: Algorithm for immediately loading diagnostic factors. Clin Implant Dent Relat Res 12(Suppl 1):e13–22
Baschong W, Suetterlin R, Hefti A, Schiel H (2001) Confocal laser scanning microscopy and scanning electron microscopy of tissue Ti-implant interfaces. Micron 32:33–41
Al-Nawas B, Götz H (2003) Three-dimensional topographic and metrologic evaluation of dental implants by confocal laser scanning microscopy. Clin Implant Dent Relat Res 5:176–183
Traini T, Degidi M, Murmura G, Piatelli A, Caputi S (2007) Bone microstructure evaluation near unloaded dental implants combining confocal scanning laser microscopy, circularly polarized light microscopy, and SEM backscattered electrons imaging. Int J Immunopathol Pharmacol 20(1 Suppl 1):37–41
Nishikawa T, Masuno K, Mori M, Tajime Y, Kakudo K, Tanaka A (2006) Calcification at the interface between titanium implants and bone: Observation with confocal laser scanning microscopy. J Oral Implantol 32:211–217
Traini T, Degidi M, Iezzi G, Artese L, Piattelli A (2007) Comparative evaluation of the peri-implant bone tissue mineral density around unloaded titanium dental implants. J Dent 35:84–92
Piatelli A, Trisi P, Passi P, Piatelli M, Cordioli GP (1994) Histochemical and confocal laser scanning microscopy study of the bone-titanium interface: an experimental study in rabbits. Biomaterials 15:194–200
Lan J, Wang ZF, Shi B, Xia HB, Cheng R (2007) The influence of recombinant human BMP-2 on bone-implant osseointegration: biomechanical testing and histomorphometric analysis. Int J Oral Maxillofac Surg 36:345–349
Abuduwali N, Lossdörfer S, Winter J, Wolf M, Götz W, Jäger A (2013) Autofluorescent characteristics of human periodontal ligament cells in vitro. Ann Anat 195:449–454
Pearce AL, Richards RG, Milz S, Schneider E, Pearce SG (2007) Animal models for implant biomaterial research in bone: a review. Eur Cells Mater 13:1–10
Stadlinger B, Pourmand P, Locher MC, Schulz MC (2012) Systemic review of animal models for the study of implant integration, assessing the influence of material, surface and design. J Clin Periodontol 39(Suppl 12):28–36
Emilson CG, Bowen WH (1981) Microbial analyses of dental plaque of monkeys (Macaca fascicularis) using fluorescent antibody techniques. Scand J Dent Res 89:458–462
Siar CH, Toh CG, Romanos G, Swaminathan D, Ong AH, Yaacob H, Nentwig G-H (2003) Peri-implant soft tissues integration of immediately loaded implants in the posterior macaque mandible: a histomorphometric study. J Periodontol 74:571–578
Romanos G, Toh GC, Siar CH, Swaminathan D, Ong AH, Yaacob H, Nentwig G-H (2001) Peri-implant bone reactions to immediately loaded implants. An experimental study in monkeys. J Periodontol 72:506–511
Moure SP, Carrard VC, Lauxen IS, Manso PPA, Oliveira MG, Martins MD, Sant Ana Filho M (2011) Collagen and elastic fibers in odontogenic entities: analysis using light and confocal laser microscopic methods. Open Dent J 5:116–21
Pavlova I, Williams M, El-Naggar A, Richards-Kortum R, Gillenwater A (2008) Understanding the biological basis of autofluorescence imaging for oral cancer detection: high resolution fluorescence microscopy in viable tissue. Clin Cancer Res 14:2396–2404
Ganeles J, Listgarten MA, Evian CI (1986) Ultrastructure of durapatite-periodontal tissue interface in human intrabony defects. J Periodontol 57:133–139
De Lange GL, Donath K (1989) Interface between bone tissue and implants of solid hydroxyapatite or hydroxyapatite-coated titanium implants. Biogeosciences 10:121–125
De Lange GL, de Putter C, de Wijs FLJA (1990) Histological and ultrastructural appearance of the hydroxyapatite-bone interface. J Biomed Mater Res 24:829–845
LeGeros RZ, Orly I, Gregoire M, Daculsi G (1991) Substrate surface dissolution and interfacial biological mineralization. In: Davies J (ed) Bone Biomaterial Interface. Toronto Univ Press, Toronto, p 76
Palmquist A, Grandfield K, Norlindh B, Mattsson T, Brånemark R, Thomsen P (2012) Bone-titanium oxide interface in humans revealed by transmission electron microscopy and electron tomography. J R Soc Interface 9:396–400
Favia G, Pilolli GP, Maiorano E (2009) Histologic and histomorphometric features of bisphosphonate-related osteonecrosis of the jaws: an analysis of 31 cases with confocal laser scanning microscopy. Bone 45:406–413
Wu Y, Qu JY (2006) Combined depth- and time-resolved autofluorescence spectroscopy of epithelial tissue. Opt Lett 31:1833–1835
Hashimoto M, Akagawa Y, Nikai H, Tsuru H (1989) Ultrastructure of the peri-implant junctional epithelium on single-crystal sapphire endosseous dental implant loaded with functional stress. J Oral Rehabil 16:261–270
Bauman GR, Rapley JW, Hallmon WW, Mills M (1993) The peri-implant sulcus. Int J Oral Maxillofac Implants 8:273–280
Marchetti C, Farina A, Cornaglia AI (2002) Microscopic, immunocytochemical, and ultrastructural properties of peri-implant mucosa in humans. J Periodontol 73:555–563
Moon IS, Berglundh T, Abrahamsson I, Linder E, Lindhe J (1999) The barrier between the keratinized mucosa and the dental implant. An experimental study in the dog. J Clin Periodontol 26:658–663
Buser D, Weber HP, Donath K, Fiorellini JP, Paquette DW, Williams RC (1992) Soft tissue reactions to non-submerged unloaded titanium implants in beagle dogs. J Periodontol 63:225–235
Acknowledgments
This research was partially supported by Dentsply Friadent GmbH Germany (Vote No. 40-02-03-2002), and the Ministry of Education, Malaysia, Fundamental Research Grant Scheme (FRGS) FP038-2013A. We gratefully acknowledge the excellent technical assistance of Ms. Lynn Kang and Ms. Joceyn Tai (confocal laser scanning microscopy) and Ms. Khoo Guat Sim (Image-Pro Express microscopy).
Conflict of Interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Siar, C.H., Toh, C.G., Romanos, G.E. et al. Comparative assessment of the interfacial soft and hard tissues investing implants and natural teeth in the macaque mandible. Clin Oral Invest 19, 1353–1362 (2015). https://doi.org/10.1007/s00784-014-1362-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-014-1362-7