Abstract
Objectives
This randomized split-mouth clinical trial was designed to evaluate the efficacy of scaling and root planing associated to the high-intensity diode laser on periodontal therapy by means of clinical parameters and microbial reduction.
Materials and methods
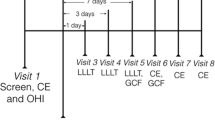
A total of 36 chronic periodontitis subjects, of both genders, were selected. One pair of contralateral single-rooted teeth with pocket depth >5 mm was chosen from each subject. All patients received non-surgical periodontal treatment, after which the experimental teeth were designated to either test or control groups. Both teeth received scaling, root planing and coronal polishing (SRP) and teeth assigned to the test group (SRP + DL) were irradiated with the 808 ± 5 nm diode laser, for 20 s, in two isolated appointments, 1 week apart. The laser was used in the continuous mode, with 1.5 W and power density of 1,193.7 W/cm2. Clinical and microbiological data were collected at baseline, 6 weeks and 6 months after therapy.
Results
There was a significant improvement of all the clinical parameters—clinical attachment level (CAL), probing depth (PD), plaque index (PI) and Bleeding on Probing (BOP)—for both groups (P < 0.001), with no statistical difference between them at the 6 weeks and the 6 months examinations. As for microbiological analysis, a significant reduction after 6 weeks (P > 0.05) was observed as far as colony forming units (CFU) is concerned, for both groups. As for black-pigmented bacteria, a significant reduction was observed in both groups after 6 months. However, the difference between test and control groups was not significant. There was no association between group and presence of Porphyromonas gingivalis, Prevotella intermedia and Aggregatibacter actinomycetemcomitans at any time of the study.
Conclusions
After 6 months of evaluation, the high-intensity diode laser has not shown any additional benefits to the conventional periodontal treatment.
Clinical relevance
The high intensity diode laser did not provide additional benefits to non-surgical periodontal treatment. More studies are necessary to prove the actual need of this type of laser in the periodontal clinical practice.

Similar content being viewed by others
References
Cugini MA, Haffajee AD, Smith C, Kent RL Jr, Socransky SS (2000) The effect of scaling and root planing on the clinical and microbiological parameters of periodontal diseases: 12-month results. J Clin Periodontol 27:30–36
Adriaens PA (2000) Adriaens LM (2004) Effects of nonsurgical periodontal therapy on hard and soft tissues. Periodontol 36:121–145
Mombelli A, Schmid B, Rutar A, Lang NP (2000) Persistence patterns of Porphyromonas gingivalis, Prevotella intermedia/nigrescens and Actinobacillus actinomyetemcomitans after mechanical therapy of periodontal disease. J Periodontol 71:14–21
Trombelli L, Rizzi A, Simonelli A, Scapoli C, Carrieri A, Farina R (2010) Age-related treatment response following non-surgical periodontal therapy. J Clin Periodontol 37:346–352
Berglundh T, Krok L, Liljenberg B, Westfelt E, Serino G, Lindhe J (1998) The use of metronidazole and amoxicillin in the treatment of advanced periodontal disease — a prospective, controlled clinical trial. J Clin Periodontol 25:354–362
Hersh EV (2000) Moore PA (2008) Adverse drug interactions in dentistry. Periodontol 46:109–142
Quirynen M, Teughels W, van Steenberghe D (2003) Microbial shifts after subgingival debridement and formation of bacterial resistance when combined with local or systemic antimicrobials. Oral Dis 1:30–37
Karlsson MR, Diogo Löfgren CI, Jansson HM (2008) The effect of laser therapy as an adjunct to non-surgical periodontal treatment in subjects with chronic periodontitis: a systematic review. J Periodontol 79:2021–2028
Schwarz F, Becker J, Sculean A, Berakdar M, Szathmari L, Georg T (2003) In vivo and in vitro effects of an Er:YAG laser, a GaAlAs diode laser, and scaling and root planing on periodontally diseased root surfaces: a comparative histologic study. Laser Surg Med 32:359–366
Theodoro LH, Haypek P, Bachmann L et al (2003) Effect of Er:YAG and diode laser irradiation on the root surface: morphological and thermal analysis. J Periodontol 74:838–843
Moritz A, Schoop U, Goharkhay K et al (1998) Treatment of periodontal pockets with a diode laser. Laser Surg Med 22:302–311
Caruso U, Nastri L, Piccolomini R, D’Ercole S, Mazza C, Guida L (2008) Use of diode laser 980 nm as adjunctive therapy in the treatment of chronic periodontitis. A randomized controlled clinical trial. New Microbiol 31:513–518
De Micheli G, Andrade AKP, Alves VT, Seto M, Pannuti CM, Cai S (2011) Efficacy of a high intensity diode laser as an adjunct to non-surgical periodontal treatment: a randomized controlled trial. Laser Med Sci 26:43–48
Borrajo JLL, Varela LG, Castro GL, Rodriguez-Nunez I, Torreira MG (2004) Diode laser (980 nm) as adjunct to scaling and root planing. Photomed Laser Surg 22:509–512
Cobb CM (2006) Lasers in periodontics: a review of the literature. J Periodontol 77:545–564
Kreisler M, Al Haj H, Daublander M, Gotz H, Duschner H, Willershausen B et al (2002) Effect of diode laser irradiation on root surfaces in vitro. J Clin Laser Med Surg 20:63–69
Haypek P, Zezell DM, Bachmann L, Marques MM (2006) Interaction between high-power diode laser and dental root surface. Thermal, morphological and biocompatibility analysis. J Oral Laser Appl 6:1–9
Tonetti MS, Claffey N (2005) Advances in the progression of periodontitis and proposal of definitions of a periodontitis case and disease progression for use in risk factor research. Group C consensus report of the 5th European Workshop in Periodontology. J Clin Periodontol 32:210–213
Tunkel J, Heinecke A, Flemmig TF (2002) A systematic review of efficacy of machine-driven and manual subgingivaldebridement in the treatment of chronic periodontitis. J Clin Periodontol 29:72–81
Kreisler M, Daublander M, Willershausen-Zonnchen B, D’Hoedt B (2001) Effect of diode laser irradiation on the survival rate of gingival fibroblast cell cultures. Laser Surg Med 28:445–450
Silness J, Löe H (1964) Periodontal disease in pregnancy II. Correlation between oral hygiene and periodontal condition. Acta Odontol Scand 22:121–135
Möller AJR (1966) Microbiological examination of root canals and periapical tissues of human teeth. Odontol Tidskr 74:1–380
Slots J, Reynolds HS (1982) Long wave UV light fluorescence for identification of black pigmented acteroids spp. J Clin Microbiol 16:1148–1151
Le Goff A, Brunetel L, Mouton C, Bonnaure-Mallet M (1997) Evaluation of root canal bacteria and their antimicrobial susceptibility in teeth with necrotic pulp. Oral Microbiol Immunol 12:318–322
Alcoforado GAP, Mckay TL, Slots J (1987) Rapid method for detection of lactose fermentation oral microorganisms. Oral Microbiol Immunol 59:35–38
Slots J (1987) Detection of colonies of bacteroides gingivalis by a rapid fluorescence assay for trypsin-like activity. Oral Microbiol Immunol 2:139–141
Schwarz F, Bieling K, Bonsmann M, Latz T, Becker J (2006) Nonsurgical treatment of moderate and advanced periimplantitis lesions: a controlled clinical study. Clin Oral Investig 10:279–288
He S, Wang Y, Li X, Hu D (2011) Effectiveness of laser therapy and topical desensitising agents in treating dentine hypersensitivity: a systematic review. J Oral Rehabil 38:348–358
Kreisler M, Al Haj H, D’Hoedt B (2005) Clinical efficacy of semiconductor laser application as an adjunct to conventional scaling and root planing. Laser Surg Med 37:350–355
Kamma JJ, Vasdekis VGS, Romanos GE (2009) The effect of diode laser (980 nm) treatment on aggressive periodontitis: evaluation of microbial and clinical parameters. Photomed Laser Surg 27:11–19
Armitage GC (2004) The complete periodontal examination. Periodontol 2000(34):22–33
Greenstein G, Caton J, Polson AM (1981) Histologic characteristics associated with bleeding after probing and visual signs of inflammation. J Periodontol 52:420–425
Lang NP, Joss A, Orsanic T, Gusberti FA, Siegrist BE (1986) Bleeding on probing—a predictor for the progression of periodontal-disease. J Clin Periodontol 13:590–596
Socransky SS, Smith C, Haffajee AD (2002) Subgingival microbial profiles in refractory periodontal disease. J Clin Periodontol 29:260–268
Socransky SS (2000) Haffajee AD (2005) Periodontal microbial ecology. Periodontology 38:135–187
Jervøe-Storm P-M, Koltzscher M, Falk W, Dörfler A, Jepsen S (2005) Comparison of cultureand real-time PCR for detection and quantification of five putative periodontopathogenic bacteria in subgingival plaque samples. J Clin Periodontol 32:778–783
Atieh MA (2008) Accuracy of real-time polymerase chain reaction versus anaerobic culture in detection of Actinobacillus actinomycetemcomitans and Porphyromonas gingivalis: a meta-analysis. J Periodontol 79:1620–1629
López NJ (2000) Occurrence of Actinobacillus actinomycetemcomitans, Porphyromonas gingivalis, and Prevotella intermedia in progressive adult periodontitis. J Periodontol 71:948–954
Offenbacher S (1996) Periodontal diseases: pathogenesis. Ann Periodontol 1:821–878
Coluzzi DJ (2000) An overview of laser wavelengths used in dentistry. Dent Clin North Am 44:753–765
Harris DM, Yessik M (2004) Therapeutic ratio quantifies laser antisepsis: ablation of Porphyromonas gingivalis with dental lasers. Laser Surg Med 35:206–213
Okamoto K, Nakayama K, Kadowaki T, Abe N, Ratnayake DB, Yamamoto K (1998) Involvement of a lysine-specific cysteine proteinase in hemoglobin adsorption and heme accumulation by Porphyromonas gingivalis. J Biol Chem 273:21225–21231
Smalley JW, Silver J, Marsh PJ, Birss AJ (1998) The periodontopathogen Porphyromonas gingivalis binds iron protoporphyrin IX in the mu-oxo dimeric form: an oxidative buffer and possible pathogenic mechanism. Biochem J 331:681–685
Smalley JW, Silver J, Birss AJ, Withnall R, Titler PJ (2003) The haem pigment of the oral anaerobes Prevotella nigrescens and Prevotella intermedia is composed of iron (III) protoporphyrin IX in the monomeric form. Microbiology 149:1711–1718
Meló TB (1987) Uptake of protoporphyrin and violet light photodestruction of Propionibacterium acnes. Z Naturforsch C 42:123–128
Soukos NS, Som S, Abernethy AD et al (2005) Phototargeting oral black-pigmented bacteria. Antimicrob Agents Chemother 49:1391–1396
Asikainen S, Chen C, Slots J (1995) Actinobacillus-actinomycetemcomitans genotypes in relation to serotypes and periodontal status. Oral Microbiol Immunol 10:65–68
Roman-Torres CVG, Aquino DR, Cortelli SC et al (2010) Prevalence and distribution of serotype-specific genotypes of Aggregatibacter actinomycetemcomitans in chronic periodontitis Brazilian subjects. Arch Oral Biol 55:242–248
Kamma JJ, Vasdekis VGS, Romanos GE (2006) The short-term effect of diode laser (980 nm) Treatment on aggressive periodontitis: evaluation of clinical and microbiological parameters. J Oral Laser Appl 6:111–1121
Acknowledgments
The authors would like to thank São Paulo Research Foundation—FAPESP, research grants 2005/56965–8. Research grants: São Paulo Research Foundation (FAPESP, São Paulo, SP, Brazil) # 05/5695-8 and Coordination for the Improvement of Higher Educated Personnel (CAPES, Brasilia, DF, Brazil).
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Euzebio Alves, V.T., de Andrade, A.K.P., Toaliar, J.M. et al. Clinical and microbiological evaluation of high intensity diode laser adjutant to non-surgical periodontal treatment: a 6-month clinical trial. Clin Oral Invest 17, 87–95 (2013). https://doi.org/10.1007/s00784-012-0703-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-012-0703-7