Abstract
Background
There are no evidence on the effects of low-intensity pulsed ultrasound (LIPUS) on surgically managed fresh fractures. We therefore performed a multicenter retrospective cohort study to investigate the effects of LIPUS on surgically managed fresh fractures.
Methods
This study included patients surgically treated for diaphyseal fractures of the femur or tibia between August 2009 and July 2010 at 14 institutions. Outcome was the union period. We performed an overall comparison of the LIPUS group (78 cases) with the control group (63 cases), as well as subgroup analyses comparing outcomes for fracture sites, fracture types, soft tissue conditions, and fixation methods between the groups.
Results
There was no significant difference between the groups in terms of distribution of cases by fracture site, fracture type, soft tissue condition, fixation method. Analyses comparing subgroups, however, showed significant differences between the two groups, particularly in relation to type C fractures, regardless of whether all cases or only closed-fracture cases were analyzed: there was an approximately 30 % reduction in the union period for type C fractures in the LIPUS group. There were also cases requiring reoperation due to lack of stability, even among the type C fractures.
Conclusions
LIPUS is effective for surgically managed, fresh, type C comminuted diaphyseal fractures of the lower limbs when there is appropriate stability at the fracture site.
Similar content being viewed by others
Introduction
The conditions needed for ultrasound-promoted bone union in an animal fracture model were first published by Duarte in 1983 [1]. The effects of low-intensity pulsed ultrasound (LIPUS) on bone union in fracture repair were subsequently confirmed in a range of basic studies. The clinical effects of LIPUS on both conservatively treated fresh fractures and surgically managed fractures with delayed union or nonunion have since been confirmed.
In 1998, Japanese health insurance began to cover LIPUS as a treatment for delayed union and nonunion. In 2008, it was also made available for fresh, postoperative, open, or comminuted fractures. However, substantiated evidence for the effects of LIPUS on surgically managed fresh fractures is still lacking. Accordingly, we investigated the effects of LIPUS on this type of fracture by performing a multicenter retrospective cohort study at Okayama University, in collaboration with Okayama University’s associated hospitals.
Materials and methods
We performed our study in collaboration with 14 hospitals associated with the author’s university, and divided the hospitals into those that actively use LIPUS (“active hospitals”) and those that do not use LIPUS (“nonactive hospitals”). We prospectively gathered information on cases involving the use of LIPUS from active hospitals according to the criteria and protocol given below. In addition, we based our control group on cases that did not involve the use of LIPUS, which we gathered retrospectively during the same period and according to the same criteria from both the active and nonactive hospitals. Subjects were patients who received surgery for diaphyseal fractures of the femur or tibia between August 2009 and July 2010. Patients in the LIPUS group received therapy with the SAFHS2000J (Teijin, Tokyo, Japan). We used the same follow-up protocol for both control and LIPUS cases. Approval was obtained from the institutional review board, and informed consent was provided by all subjects. Differences between groups were analyzed using the Mann–Whitney U test and Pearson’s chi-square test where appropriate. Results were considered statistically significant when P <0.05.
Criteria and protocol
Criteria for inclusion in the study were: ≥16 years of age, spoke Japanese, consented to participate in the follow-up, and had a fresh femoral or tibial diaphyseal fracture—either open (Gustilo type I, II, or IIIa) [2, 3] or closed—for which LIPUS was available within 3 weeks of injury. We excluded patients who were <16 years of age, had fractures in bones other than the femur or tibia, had a metaphyseal or pathological fracture or a refracture, had a Gustilo type IIIb or IIIc open fracture or periprosthetic fracture, or did not consent to participate in the follow-up.
Outcome was the time until union (union period). Two experimental orthopedic surgeons, the attending surgeons, and the surgeons from the other hospitals associated with our university determined the point of bone union, defined as the point when cortical bony continuity was found at three sites or more using bidirectional X-rays, while also taking into consideration the clinical findings and course. We considered bony continuity to be the point at which the callus matured. Follow-up consisted of monthly radiography until union was confirmed and then follow-up surveys until rehabilitation was confirmed. We performed LIPUS for at least 3 months until union was achieved. Although treatment during recovery was subject to the protocol of each hospital, partial weight bearing began from an average of 1 month postoperatively, with subsequent progression to full weight bearing dependent on the level of callus formation.
Results
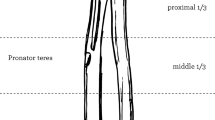
Ninety cases were registered in the LIPUS group, but 12 were excluded because of a lack of adequate follow-up data. There were 88 cases from the same period in the control group, with 25 excluded because of a lack of proper follow-up. We had 78 cases in the LIPUS group (51 males and 27 females, mean age 48.7 years) and 63 cases in the control group (38 males and 25 females, mean age 46.9 years). In the LIPUS group, therapy was started within 3 weeks after the injury. We found no significant difference between the groups in terms of the distribution of cases by fracture site, fracture type (AO classification A/B/C) [4] (Fig. 1), soft tissue condition, and fixation. With regard to final outcome, there were four cases requiring revision surgery in the LIPUS group and one in the control group (Table 1).
We performed an overall statistical analysis as well as subgroup analyses of union period by fracture site, fracture type, soft tissue condition, and fixation for both the LIPUS and control groups. The overall comparison of the groups did not find any significant differences, with overall mean union periods of 4.2 and 4.8 months observed for the LIPUS and control groups, respectively. A subgroup analysis of fracture site showed a significant difference between the groups for “tibia,” and a subgroup analysis of fracture type found a significant difference between the groups for “type C” fractures (Table 2; Figs. 2, 3, 4, 5, 6). We performed additional subgroup analyses of the combinations “fracture site/fracture type” and “soft tissue condition/fracture type” because of the marked difference in outcome for type C fractures between the groups. These analyses showed significant differences in outcome for femur/type C, tibia/type C, and closed/type C fractures, with the union period being approximately 30 % shorter in the LIPUS group for these fracture site/type combinations (Table 3; Figs. 7, 8, 9, 10).
Although the reoperation rate was high in the LIPUS group, there was no statistically significant difference in reoperation rate between the two groups. We analyzed the five cases that required revision surgery. One case originally had a large (5 cm) bony defect, but union was achieved outside of the defect area. In the other four cases, the smaller nails used in the first operation were insufficient, resulting in nonunion due to a lack of stability. Bone union was achieved with a bone graft in the first case and via exchange nailing [5, 6] in the other four cases (Table 4).
We performed separate subgroup analyses of the open and closed fracture groups. However, we could not perform reliable statistical analysis on the open fracture group (LIPUS 21 cases, control 22 cases) because there were too few cases and large differences. On the other hand, the closed fracture group (LIPUS 53 cases, control 42 cases) was analyzed using the same method as employed for the overall analysis (Tables 5, 6), although the number of cases with closed type A tibial fractures was too small, so this combination could not be analyzed statistically. The closed fracture group analysis showed significant differences in outcome between the groups for type C fractures, tibial fractures, and tibia/type C fractures, and there was a tendency (P = 0.067) for the union period to be shorter in the LIPUS group than in the control group for femur/type C fractures (Figs. 10, 11).
Discussion
Basic research, including in vitro [7] and animal studies [8–10], has shown that LIPUS accelerates the repair reactions involved in bone union at the cellular level. Busse [11] published a systematic review of clinical studies on LIPUS therapy in 2009. In conservatively treated fresh fractures, an analysis of 67 cases of diaphyseal fracture of the tibia [12], 61 cases of distal radius fracture [13], and 30 cases of scaphoid fracture [14] found LIPUS therapy to be effective. Union periods in the LIPUS group were 30–40 % shorter than those in the control group. Multicenter analysis [15, 16] also showed that LIPUS is effective in cases of delayed union and nonunion. The effects of LIPUS in surgically treated fresh fractures are not, however, as clear. One study demonstrated no effect of LIPUS in 32 cases of diaphyseal fracture of the tibia with intramedullary nailing [17]. Another study showed that LIPUS shortened the period of cortical bridging, with callus formation in 11 cases of diaphyseal fracture of the tibia with intramedullary nailing and in 19 cases with external fixation [18]. However, we did not find any other studies demonstrating the effects of LIPUS on surgically managed fresh fractures.
Although there was no significant difference in the union period between the LIPUS and control groups overall (i.e., for all cases) in this study, we found significant differences between these groups when we performed subgroup analyses—mainly when we focused on type C fractures. It is difficult to precisely irradiate the fracture site in the femur, as the irradiation site is not easy to determine [19]. However, the target for irradiation in a type C fracture, with its wide fracture area, is larger than the targets in type A and B fractures, so targeting is easier for type C fractures, even in the femur. In addition, early weight bearing is possible in types A and B if the main segments are stabilized by bony contact after fixation. In these fracture types, stimulation through early and appropriate weight bearing [20] may already lead to the maximum potential for union at the fracture site, in which case LIPUS would have no additional stimulatory effect on the fracture. On the other hand, the fact that there was a significant difference between the two groups for type C fractures (in which contact cannot be achieved between the main fragments) suggests that the stimulatory effect of LIPUS is equivalent to that of an appropriate weight-bearing stimulus. LIPUS may be particularly useful for this fracture type, because type C fractures cannot tolerate early weight-bearing stimulus between the segments, even with surgery.
Soft tissue condition was found to influence the union period. However, when we focused on each soft-tissue condition, we did not find a significant difference in outcome between the groups, except for closed type C fractures (Figs. 5, 9, 10). Because Gustilo type IIIb and IIIc fractures were excluded from this study, there is the possibility that the vascular conditions around the fracture site in open fractures were almost the same as those in closed fractures. This may have led to almost the same outcome results in the analysis of all cases as in the analysis of the closed fractures only.
Since the treatment was administered by a variety of surgeons in this multi-center study, we focused on diaphyseal fractures of the femur and tibia in order to minimize bias due to differences in surgical technique, because the operative method was standardized for these fracture sites and because determination of bone union is easier at these sites than at others. We attempted to minimize the bias still further by ensuring that the surgeons were the members of the trauma group of our university, that they had been licensed for over 10 years, that each was the chief director of the orthopedic trauma service at one of the hospitals included in the study, and that they had completed the AOTrauma advance course.
The assignment of cases could not be randomized in this study design. Because LIPUS treatment for fresh postoperative fractures is covered by Japanese health insurance, it would have been ethically problematic to establish a control group, so we were compelled to perform a retrospective cohort study. However, we consider this study to have the same significance as a prospective case series investigating the effects of LIPUS therapy on fresh fractures.
LIPUS does not compensate for a lack of stability. Thus, even in type C fractures (for which LIPUS was found to be effective in this study), revision surgery was still necessary when the fracture was unstable. For any fracture that may lack stability and in which union has still not occurred 3 months postoperatively, reoperation (changing the fixation or adding a bone graft) should be considered instead of continuing LIPUS, which is ineffective in this situation.
Conclusion
We investigated the effect of LIPUS on surgically managed fresh fracture cases involving the shaft of the femur or tibia by performing a multi-center retrospective cohort study. We analyzed the outcomes (i.e., union periods) of 78 cases in our LIPUS group and 63 cases in our control group. Although there was no significant difference in outcome between the two groups overall, LIPUS appeared to be highly effective, with significant differences observed in a subgroup analysis of type C fractures in particular; for type C fractures, LIPUS facilitated an approximately 30 % decrease in the union period. However, there were cases requiring revision surgery due to a lack of stability, even among the type C fractures. Therefore, LIPUS is effective for type C fractures that are sufficiently stable at the fracture site.
References
Duarte LR. The stimulation of bone growth by ultrasound. Arch Orthop Trauma Surg. 1983;101:153–9.
Gustilo RB, Anderson JT. Prevention of infection in the treatment of one thousand and twenty-five open fractures of long bones: retrospective and prospective analyses. J Bone Jt Surg Am 1976;58:453–8.
Gustilo RB, Mendoza RM, Williams DN. Problems in the management of type III (severe) open fractures: a new classification of type III open fractures. J Trauma. 1984;24:742–6.
Muller ME, Nazarian S, Koch P, Schatzker J. Comprehensive classification of fractures of long bones. Heidelberg: Springer; 1990.
Giannoudis PV, Matthews SJ, Smith RM. Exchange nailing for femoral nonunion. J Orthop Trauma. 2000;14:522–3.
Zelle BA, Gruen GS, Klatt B. Exchange reamed nailing for aseptic nonunion of the tibia. J Trauma. 2004;57:1053–9.
Yang KH, Parvizi J, Wang SJ. Exposure to low-intensity ultrasound increases aggrecan gene expression in a rat femur fracture model. J Orthop Res. 1996;14:802–9.
Azuma Y, Ito M, Harada Y, Takagi H, Ohta T, Jingushi S. Low-intensity-pulsed ultrasound accelerates rat femoral fracture healing by acting on the various cellular reactions in the fracture callus. J Bone Miner Res. 2001;16:671–80.
Rawool NM, Goldberg BB, Forsberg F, Winder AA, Hume E. Power Doppler assessment of vascular changes during fracture treatment with low-intensity ultrasound. J Ultrasound Med. 2003;22:145–53.
Takikawa S, Matsui N, Kokubu T, Tsunoda M, Fujioka H, Mizuno K, Azuma Y. Low-intensity pulsed ultrasound initiates bone healing in rat nonunion fracture model. J Ultrasound Med. 2001;20:197–205.
Busse JW, Kaur J, Mollon B, Bhandari M, Tornetta P 3rd, Schünemann HJ, Guyatt GH. Low intensity pulsed ultrasonography for fractures: systematic review of randomised controlled trials. BMJ. 2009;27: 338–b351.
Heckman JD, Ryaby JP, McCabe J, Frey JJ, Kilcoyne RF. Acceleration of tibial fracture-healing by non-invasive, low-intensity pulsed ultrasound. J Bone Jt Surg Am. 1994;76:26–34.
Kristiansen, Ryaby JP, McCabe J, Frey JJ, Roe LR. Accelerated healing of distal radial fractures with the use of specific, low-intensity ultrasound. A multicenter, prospective, randomized, double-blind, placebo-controlled study. J Bone Jt Surg Am. 1997;79:961–73.
Mayr E, Rudzki MM, Rudzki M, Borchardt B, Häusser H, Rüter A. Does low intensity, pulsed ultrasound speed healing of scaphoid fractures? Handchir Mikrochir Plast Chir. 2000;32:115–22 (in German).
Frankel VH, Mizuho K. Management of nonunion with pulsed low-intensity ultrasound therapy—international results. Surgical Technol Int. 2002;10:195–200.
Mizuno K, Yamano Y, Itoman M. Multi-center clinical trial on low-intensity pulse ultrasound for delayed union and pseudarthrosis. J Orthopaed Traumatol. 2003;46:757–216.
Emami A, Petrén-Mallmin M, Larsson S. No effect of low-intensity ultrasound on healing time of intramedullary fixed tibial fractures. J Orthop Trauma. 1999;13:252–7.
Leung KS, Lee WS, Tsui HF, Liu PP, Cheung WH. Complex tibial fracture outcomes following treatment with low-intensity pulsed ultrasound. Ultrasound Med Biol. 2004;30:389–95.
Arai M, Takenaka N, Yoshino A, Katoh N, Nishizawa M, Hirose H, Watanabe Y, Matsushita T. Clinical results of the treatment for nonunion or delayed union using low-intensity pulsed ultrasound (LIPUS) and targeting device. Fractures. 2005;27:21–6.
Wolff J. The classic: on the theory of fracture healing. Clin Orthop Relat Res. 2010;468:1052–5.
Acknowledgments
We would like to express our heartfelt gratitude to the following hospitals and doctors for their cooperation with this study: Okayama Saiseikai General Hospital (Dr. Yukio Kawakami), Okayama Citizens’ Hospital (Dr. Masaaki Usui), Okayama Red Cross General Hospital (Dr. Shinshichirou Higashihara, Dr. Takeshi Doi), Okayama Rosai Hospital (Dr. Chuji Terada), Okayama Medical Center (Dr. Toru Sato, Dr. Naofumi Shiota), Tsuyama Chuo Hospital (Dr. Yasushi Takagi), Akou Central Hospital (Dr. Kingo Takahashi), Fukuyama City Hospital (Dr. Kenichi Ogawa), Nippon Kokan Fukuyama Hospital (Dr. Yoichiro Uchida), Onomichi Municipal Hospital (Dr. Takahiko Hirooka), Kure Kyosai Hospital (Dr. Hidefumi Teramoto), Iwakuni Clinical Center (Dr. Masaharu Yasumitsu), Kagawa Rousai Hospital (Dr. Takashi Maehara), and Chikamori Hospital (Dr. Kiyoto Kinugasa).
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Kinami, Y., Noda, T. & Ozaki, T. Efficacy of low-intensity pulsed ultrasound treatment for surgically managed fresh diaphyseal fractures of the lower extremity: multi-center retrospective cohort study. J Orthop Sci 18, 410–418 (2013). https://doi.org/10.1007/s00776-013-0358-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00776-013-0358-5