Abstract
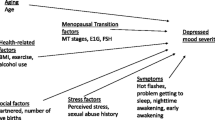
Perimenopause has long been associated with psychological distress, both anecdotally and clinically. Research has identified this time as a period of increased risk for both first-episode depression and for depression reoccurrence. However, we know that the majority of women do not experience these difficulties during perimenopause. This review examines the current research literature looking at the factors associated with depression during perimenopause, with a view to identifying those factors which are protective and those factors which predict increased risk. From the literature, it is evident that some women have a hormonal vulnerability to mood disorders. However, this does not account for the phenomenon of perimenopausal depression in and of itself. Rather, there appears to be a complex interplay between hormonal vulnerability, the psychosocial resources one has (coping skills and social support), their overall well-being (exercise and other lifestyle factors) and the demands on their coping resources (stressful life events). The complexity of the relationship between perimenopause and depression means that there is a need to look beyond either as a sole explanation of mood during midlife. Education is required for both general practitioners and for women regarding the individual risks of psychological distress during perimenopause, as well as the knowledge of the life factors which we know to be protective.
Similar content being viewed by others
References
ABS (2009) Home and away: the living arrangements of young people. Aust Soc Trends 4102:25–30
AIHW (2003) Perinatal statistics series: Australia’s mothers and babies 2000. N. P. S. Unit. Perinatal Statistics Series no. 12. Australian Institute of Health and Welfare, Canberra
Almeida OP (1999) Sex playing with the mind. Effects of oestrogen and testosterone on mood and cognition. Arquivos de Neuro-Psiquiatria 57(3A):701–706
Arpels JC (1996) The female brain hypoestrogenic continuum from the premenstrual syndrome to menopause. A hypothesis and review of supporting data. J Reprod Med 41(9):633–639
Avis NE, Brambilla D et al (1994) A longitudinal analysis of the association between menopause and depression: results from the Massachusetts Women’s Health Study. Ann Epidemiol 1994(14):214–220
Avis NE, Crawford S et al (1997) Psychosocial, behavioural, and health factors related to menopause symptomatology. Womens Health 3:103–120
Avis NE, McKinlay SM (1991) A longitudinal analysis of women’s attitudes toward the menopause: results from the Massachusetts Women’s Health Study. Maturitas 13(1):65–79
Ayubi-Moak I, Parry BL (2002) Psychiatric aspects of menopause. In: Kornstein SG, Clayton AH (eds) Women’s mental health: a comprehensive textbook. Guilford, New York, pp 132–143
Ballinger S (1985) Psychosocial stress and symptoms of menopause: a comparative study of menopause clinic patients and non-patients. Maturitas 7:315–327
Barber CE (1989) Transition to the empty nest. Ageing and the family. Health and Company, Lexington, pp 15–32
Binfa L, Castelo-Branco C et al (2004) Influence of psycho-social factors on climacteric symptoms. Maturitas 48:425–431
Bloch M, Schmidt PJ et al (2000) Differential behavioural effects of gonadal steroids in women with a history of postpartum depression. Am J Psychiatry 157:924–930
Boyce P, Parker G et al (1991) Personality as a vulnerability factor to depression. Br J Psychiatry 159:106–114
Bromberger JT (2004) A psychosocial understanding of depression in women: for the primary care physician. J Am Med Wom Assoc 59:198–206
Bromberger JT, Assman SF et al (2003) Persistent mood symptoms in a multiethnic community cohort of pre- and peri-menopausal women. Am J Epidemiol 158:347–356
Bromberger JT, Kravitz HM et al (2008) Predictors of first lifetime episodes of major depression in midlife women. Psychol Med 39:55–64
Bromberger JT, Matthews K et al (2007) Depressive symptoms during the menopausal transition: the study of women’s health across the nation. J Affect Disord 103(1–3):267–272
Bromberger JT, Meyer PM et al (2001) Psychological distress and natural menopause: a multiethnic community study. Am J Public Health 91(9):1435–1442
Bromberger JT, Schott LL et al (2010) Longitudinal change in reproductive hormones and depressive symptoms across the menopausal transition. Arch Gen Psychiatry 67(6):598–607
Brownson RC, Eyler AA et al (2000) Patterns and correlates of physical activity among US women 40 years and older. Am J Public Health 90:264–270
Brugge KL, Kripke DF et al (1989) The association of menopausal status and age with sleep disorders. Sleep Res 18:208
Burger H, Dudley E et al (1999) Prospectively measured levels of serum follicle-stimulating hormone, estradiol, and the dimeric inhibins during the menopausal transition in a population-based cohort of women. J Clin Endocrinol Metab 84:4025–4030
Burleson MH, Todd M et al (2010) Daily vasomotor symptoms, sleep problems, and mood: using daily data to evaluate the domino hypothesis in middle-aged women. Menopause 17(1):87–95
Carver CS, Scheier MF et al (1989) Assessing coping strategies: a theoretically based approach. J Personal Soc Psychol 56(2):267–283
Choi H, Lee D et al (2004) A structural model of menopausal depression in Korean women. Arch Psychiatr Nurs 18(6):235–242
Cohen LS, Soares CN et al (2006) Risk for new onset of depression during the menopausal transition: the Harvard study of moods and cycles. Arch Gen Psychiatry 63(4):385–390
Cohen S (1987) Social factors and depressive symptoms. PsycCRITIQUES 32:360–362. DOI: Electronic Collection: 2006-06447-039. http://dx.doi.org/10.1037/027006
Cooke DJ (1985) Social support and stressful life events during mid-life. Maturitas 7:303–313
Cooke DJ, Greene J (1981) Types of life events in relation to symptoms at the climacterium. J Psychosom Res 25(1):5–11
Daley A (2008) Exercise and depression: a review of reviews. Journal of Clinical Psychology in Medical Settings 15(2):140–147
Deeks AA, McCabe MP (2004) Well-being and menopause: an investigation of purpose in life, self-acceptance and social role in premenopausal, perimenopausal and postmenopausal women. Qual Life Res 13:389–398
Dennerstein L, Dudley E et al (2002) Empty nest or revolving door? A prospective study of women’s quality of life in midlife during the phase of children leaving and re-entering the home. Psychol Med 32(3):545–550
Dennerstein L, Lehert P et al (1999) Mood and the menopausal transition. J Nerv Ment Dis 187(11):685–691
Dennerstein L, Lehert P et al (2001) Factors contributing to positive mood during the menopausal transition. J Nerv Ment Dis 189(2):84–89
Dennerstein L, Smith A et al (1994) Psychological well-being, mid-life and the menopause. Maturitas 20:1–11
Dennerstein L, Smith AMA et al (1993) Menopausal symptoms in Australian women. Med J Aust 159:232–236
Elavsky S, McAuley E (2005) Physical activity, symptoms, esteem, and life satisfaction during menopause. Maturitas 52:374–385
Freeman EW, Sammel MD et al (2006a) Associations of hormones and menopausal status with depressed mood in women with no history of depression. Arch Gen Psychiatry 63(4):375–382
Freeman EW, Sammel MD et al (2004a) Hormones and menopausal status as predictors of depression in women in transition to menopause. Arch Gen Psychiatry 61:62–70
Freeman EW, Sammel MD et al (2004b) Premenstrual syndrome as a predictor of menopausal symptoms. Obstet Gynecol 103(5 pt 1):960–966
Freeman MP, Hill R et al (2006b) Escitalopram for perimenopausal depression: an open-label pilot study. J Wom Health 15(7):857–861
Fuh J-L, Wang S-J et al (2006) A longitudinal study of cognition change during early menopausal transition in a rural community. Maturitas 53(4):447–453
Gold EB, Block G et al (2004) Lifestyle and demographic factors in relation to vasomotor symptoms: baseline results from the study of women’s health across the nation. Am J Epidemiol 159(12):1189–1199
Goldstat R, Briganti E et al (2003) Transdermal testosterone therapy improves wellbeing, mood, and sexual function in premenopausal women. Menopause 10(5):390–398
Greene JG, Cooke DJ (1980) Life stress and symptoms at the climacterium. Br J Psychiatry 136:486–491
Hardy R, Kuh D (2002) Change in psychological and vasomotor symptom reporting during the menopause. Soc Sci Med 55:1975–1988
Harlow BL, Cohen LS et al (1999) Prevalence and predictors of depressive symptoms in older premenopausal women. Arch Gen Psychiatry 56:418–424
Harlow SD, Gass M et al (2012) Executive summary of the Stages of Reproductive Aging Workshop +10: addressing the unfinished agenda of staging reproductive aging. Menopause 19(4):105–114.
Hecht E, Mensh IN (1975) Life’s ups and downs may leave you down and out. PsycCRITIQUES 20: 639–640. DOI: Electronic Collection: 2006-06277-020. http://dx.doi.org/10.1037/0013564 Accessed 13 Aug 2010
Holte A, Mikkelsen A (1991) Psychosocial determinants of climacteric complaints. Maturitas 13:205–215
Hunter M (1992) The South-East England longitudinal study of the climacteric and postmenopause. Maturitas 14:117–126
Igarashi M, Saito H et al (2000) Stress vulnerability and climacteric symptoms: life events, coping behavior, and severity of symptoms. Gynecol Obstet Investig 49(3):170–178
Joffe H (2003) Assessment and treatment of hot flushes and menopausal mood disturbance. Psychiatr Clin N Am 26(3):563
Joffe H, Hall JE et al (2002) Vasomotor symptoms are associated with depression in perimenopausal women seeking primary care. Menopause 9(6):392–398
Kendler KS, Thornton LM et al (2000) Stressful life events and previous episodes in the etiology of major depressive symptoms and major depression in women: an evaluation of the “kindling” hypothesis. Am J Psychiatry 157:1243–1251
Kendler KS, Walters EE et al (1995) The structure of the genetic and environmental risk factors for six major psychiatric disorders in women: phobia, generalized anxiety disorder, panic disorder, bulimia, major depression, and alcoholism. Arch Gen Psychiatry 52(5):374–383
Kendler KS, Prescott CA et al (2000) Causal relationship between stressful life events and the onset of major depression: reply. Am J Psychiatry 157(8):1345
Kronenberg F (1990) Hot flashes: epidemiology and physiology. Ann New York Acad Sci 592:52–86
Kuh DL, Wadsworth M et al (1997) Women’s health in midlife: the influence of the menopause, social factors and health in earlier life. Br J Obstet Gynecol 104:923–933
McKinlay JB, Mckinlay SM et al (1987) The relative contribution of endocrine changes and social circumstances to depression in mid-aged women. Journal of Health and Social Behavior 4:345–363
Miech RA, Shanahan MJ (2000) Socioeconomic status and depression over the life course. J Heal Soc Behav 41(2):162–176
Mirzaiinjmabadi K, Anderson D et al (2006) The relationship between exercise, body mass index and menopausal symptoms in midlife Australian women. Int J Nurs Pract 12(1):28–34
Moline ML, Broch L et al (2003) Sleep in women across the life cycle from adulthood through menopause. Sleep Med Rev 7(2):155–177 [Review] [119 refs]
Morse CA, Dudley E et al (1998) Relationships between premenstrual complaints and perimenopausal experiences. J Psychosom Obstet Gynecol 19(4):182–191
Murrell SA, Himmelfarb S et al (1983) Prevalence of depression and its correlates in older adults. Am J Epidemiol 117(2):173–185
Neri I, Demyttenaere K et al (1997) Coping style and climacteric symptoms in a clinical sample of postmenopausal women. J Psychosom Obstet Gynecol 18:229–233
Noble RE (2005) Depression in women. Metabolism 54:49–52
Öztürk Ö, Eraslan D et al (2006) The risk factors and symptomatology of perimenopausal depression. Maturitas 55:180–186
Parry BL (2008) Perimenopausal depression. Am J Psychiatry 165(1):23–27
Parry BL (2010) Optimal management of perimenopausal depression. Int J Wom Health 2:143–151
Parry BL, Martinez LF et al (2006) Sleep, rhythms and women’s mood. Part II. Menopause. Sleep Med Rev 10:197–208
Raup JL, Myers JE (1989) The empty nest syndrome: myth or reality? J Couns Dev 68(2):180–183
Richards M, Rubinow DR et al (2006) Premenstrual symptoms and perimenopausal depression. Am J Psychiatry 163(1):133–137
Santoro N, Torrens J et al (2005) Correlates of circulating androgens in mid-life women: the study of women’s health across the nation. J Clin Endocrinol Metab 90(8):4836–4845
Schmidt PJ, Haq N et al (2004a) A longitudinal evaluation of the relationship between reproductive status and mood in perimenopausal women. Am J Psychiatry 161(12):2238–2244
Schmidt PJ, Murphy J et al (2004b) Stressful life events, personal losses, and perimenopause-related depression. Arch Wom Ment Health 7(1):19-–26
Schmidt PJ, Nieman L et al (2000) Estrogen replacement in perimenopause-related depression: a preliminary report. Am J Obstet Gynecol 183(2):414–420
Schmidt PJ, Nieman LK et al (1998) Differential behavioral effects of gonadal steroids in women with and in those without premenstrual syndrome. Obstet Gynecol Surv 53(5):291–292
Schwingl PJ, Hulka BS et al (1994) Risk factors for menopausal hot flashes. Obstet Gynecol 84:29–34
Soares CN, Almeida OP et al (2001) Efficacy of estradiol for the treatment of depressive disorders in perimenopausal women: a double-blind, randomized, placebo-controlled trial. Arch Gen Psychiatry 58(6):529–534
Soules MR, Sherman S et al (2001) Executive summary: stages of reproductive aging workshop (STRAW). Climacteric 4(11770182):267–272
Sternfeld B, Quesenberry C et al (1999) Habitual physical activity and menopausal symptoms. J Wom Health 8:115–123
Stewart DE, Boydell KM (1993) Psychologic distress during menopause: associations across the reproductive life cycle. Int J Psychiatr Med 23:157–162
Thurston R, Joffe H et al (2006) Physical activity and risk of vasomotor symptoms in women with and without a history of depression: results from the Harvard Study of Moods and Cycles. Menopause 13:553–560
Veeninga AT, Kraaimaat FW (1989) Life stress and symptoms in menopause clinic patients and non-patients. J Psychosom Obstet Gynecol 10(3):269–277
Whiteman MK, Staropoli CA et al (2003) Risk factors for hot flashes in midlife women. J Wom Health 12:459–472
Wilbur J, Dan A et al (1990) The relationship among menopausal status, menopausal symptoms, and physical activity in midlife women. Fam Community Health 13:67–78
Woods NF, Mitchell ES (1996) Patterns of depressed mood in midlife women: observations from the Seattle Midlife Women’s Health Study. Res Nurs Heal 19:111–123
Woods NF, Mitchell ES (1997) Pathways to depressed mood for midlife women: observations from the Seattle Midlife Women’s Health Study. Res Nurs Heal 20:119–129
Woods NF, Smith-DiJulio K et al (2008) Depressed mood during the menopausal transition and early postmenopause: observations from the Seattle Midlife Women’s Health Study. Menopause: The Journal of The North American Menopause Society 15(3):223–232
Youngwhee L, Hwasoon K (2008) Relationships between menopausal symptoms, depression, and exercise in middle-aged women: a cross-sectional survey. Int J Nurs Stud 45:1816–1822
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Gibbs, Z., Lee, S. & Kulkarni, J. What factors determine whether a woman becomes depressed during the perimenopause?. Arch Womens Ment Health 15, 323–332 (2012). https://doi.org/10.1007/s00737-012-0304-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00737-012-0304-0