Summary
Purpose
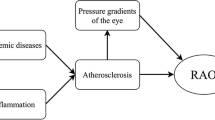
Retinal artery occlusions (RAO) cause sudden vision deterioration and visual field defects. While Albrecht von Graefe was the first to describe RAO in 1859, Hollenhorst reported about yellow plaques in the retinal arteries in 1961. Embolism from cardiac valves or plaques of the carotid artery are a common reason for RAO. Transesophageal echocardiography (TEE) has the potential to diagnose thrombotic material at the cardiac valves or plaques of the aortic arch with more precision than transthoracic echocardiography (TTE). Furthermore associations of RAO with arteriosclerosis is discussed.
Methods
117 patients with RAO, that had undergone TEE, were included in our retrospective study.
Results
Around 4.3 % of patients had thrombotic material at the cardiac valves, 10 % persistent foramen ovale, 54.7 % insufficient cardiac valves and 18.8 % plaques in the aortic arch. A total of 88 % of patients had at least one arteriosclerotic risk factor, 68 % arterial hypertension, 59.8 % hypercholesterolemia and 23.1 % diabetes mellitus. Moreover, 36.8 % had antithrombotic therapy and 67.3 % plaques in the internal carotid artery.
Conclusion
Alltogether, 40.2 % of patients had higher risk for thromboembolic complications, diagnosed with TEE.
Zusammenfassung
Hintergrund
Retinale arterielle Verschlüsse (RAO) verursachen plötzliche Visusverschlechterungen und Gesichtsfeldveränderungen. Die Erstbeschreibung der RAO erfolgte duch Albrecht von Graefe im Jahr 1859, Hollenhorst konnte 1961 über gelbe Plaques in den retinalen Gefäßen berichten. Embolisches Material von den Herzklappen oder Carotisplaques wird allgemein als Ursache für die RAO postuliert. Die Transösophageale Echokardiographie (TEE) hat das Potential solche Thromben besser als die Transthorakale Echokardiographie (TTE) aufzuzeigen. Unabhängig davon werden Assoziationen der RAO mit Arteriosklerose diskutiert.
Methode
117 Patienten/innen mit RAO, die eine TEE bei der Durchuntersuchung erhalten hatten, wurden in diese retrospektive Studie inkludiert.
Resultate
4,3 % der Patienten/innen hatten Vegetationen auf den Herzklappen, 10 % ein persistierendes Foramen ovale, 54,7 % Herzklappeninsuffizienzen und 18,8 % Plaques im Aortenbogen. 88 % der Patienten/innen hatten zumindest einen arteriosklerotischen Risikofaktor, 68 % arterielle Hypertension, 59,8 % Hypercholesterinämie und 23.1 % Diabetes mellitus. 36.8 % der Patienten/innen hatten thromboseprophylaktische Therapie und 67,3 % Plaques der Carotis Interna.
Schlussfolgerung
Zusammenfassend hatten 40,2 % der Patienten/innen ein höheres Risiko für eine thromboembolische Komplikation, entsprechend der in der TEE festgestellten Pathologien.

Similar content being viewed by others
References
Hollenhorst RW. Significance of bright plaques in the retinal arterioles. JAMA. 1961;178:23–9.
Hayreh SS, Podhajsky PA, Zimmerman MB. Retinal artery occlusion: associated systemic and ophthalmic abnormalities. Ophthalmology. 2009;116(10):1928–36.
Schmidt D, Hetzel A, Geibel-Zehender A, Schulte-Mönting J. Systemic diseases in non-inflammatory branch and central retinal artery occlusion—an overview of 416 patients. Eur J Med Res. 2007;12(12):595–603.
Leisser C. Hyperlipidaemia and increased systemic blood pressure—is there a connection to retinal artery occlusion? Spektrum Augenheilkd. 2010;24(3):154–6.
Leisser C. Risk factors of retinal artery occlusion. Spektrum Augenheilkd. 2012;26(4):202–4.
Weger M, Stanger O, Deutschmann H, et al. The role of hyperhomocysteinemia and methylenetetrahydrofolate reductase (MTHFR) C677T mutation in patients with retinal artery occlusion. Am J Ophthalmol. 2002;134:57–61.
Dunlap AB, Kosmorsky GS, Kashyap VS. The fate of patients with retinal artery occlusion and Hollenhorst plaque. J Vasc Surg. 2007;46(6):1125–9.
Wong TY, Larsen EK, Klein R et al. Cardiovascular risk factors for retinal vein occlusions and arteriolar emboli: the atherosclerosis risk in communities and cardiovascular health studies. Ophthalmology. 2005;112(4):540–7.
Blice JB, Brown GC. Diseases of the retina and vitreous. 1st ed. Philadelphia: WB Saunders; 1999. p. 109–27. (Retinal vascular occlusive disease).
Ross R. Atherosclerosis—an inflammatory disease. N Engl J Med. 1999;340:115–26.
Kramer M, Goldenberg-Cohen N, Shapira Y, et al. Role of transesophageal echocardiography in the evaluation of patients with retinal artery occlusion. Ophthalmology. 2001;108(8):1461–4.
Hunder GG, Bloch DA, Michel BA, et al. The American College of Rheumatology 1990 criteria for the classification of giant cell arteritis. Arthritis Rheum. 1990;33(8):1122–8.
Stöllberger C, Brainin M, Abzieher F, Slany J. Embolic stroke and transesophageal echocardiography: can clinical parameters predict the diagnostic yield? J Neurol. 1995;242(7):437–42.
Tunick PA, Perez JL, Kronzon I. Protruding atheromas in the thoracic aorta and systemic embolization. Ann Intern Med. 1991;115(6):423–7.
Tunick PA, Rosenzweig BP, Katz ES, Freedberg RS, Perez JL, Kronzon I. High risk for vascular events in patients with protruding aortic atheromas: a prospective study. J Am Coll Cardiol. 1994;23(5):1085–90.
Overell JR, Bone I, Lees KR. Intraatrial septal abnormalities and stroke. A meta-analysis of case-controll studies. Neurology. 2000;55:1172–9.
Wang JJ, Cugati S, Knudtson MD, et al. Retinal arteriolar emboli and long-term mortality: pooled data analysis from two older populations. Stroke. 2006;37(7):1833–6.
Chang YS, Jan RL, Weng SF, et al. Retinal artery occlusion and the 3-year risk of stroke in Taiwan: a nationwide population-based study. Am J Ophthalmol. 2012;154(4):645–52.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Leisser, C. Risk factor analysis in patients with retinal artery occlusion with respect to transesophageal echocardiography. Spektrum Augenheilkd. 28, 118–120 (2014). https://doi.org/10.1007/s00717-014-0218-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00717-014-0218-5
Keywords
- Retinal artery occlusion
- Transesophageal echocardiography
- Plaques of the carotid artery
- Arteriosclerosis