Abstract
Decreased blood–brain barrier (BBB) efflux function of the P-glycoprotein (P-gp) transport system could facilitate the accumulation of toxic compounds in the brain, increasing the risk of neurodegenerative pathology such as Parkinson’s disease (PD). This study investigated in vivo BBB P-gp function in patients with parkinsonian neurodegenerative syndromes, using [11C]-verapamil PET in PD, PSP and MSA patients. Regional differences in distribution volume were studied using SPM with higher uptake interpreted as reduced P-gp function. Advanced PD patients and PSP patients had increased [11C]-verapamil uptake in frontal white matter regions compared to controls; while de novo PD patients showed lower uptake in midbrain and frontal regions. PSP and MSA patients had increased uptake in the basal ganglia. Decreased BBB P-gp function seems a late event in neurodegenerative disorders, and could enhance continuous neurodegeneration. Lower [11C]-verapamil uptake in midbrain and frontal regions of de novo PD patients could indicate a regional up-regulation of P-gp function.
Similar content being viewed by others
Introduction
The causes of neurodegenerative brain diseases are unknown. Also the factors that result in continuous neurodegeneration in these diseases are not understood. Genetic susceptibility and exposure to neurotoxins are contributors to brain tissue malfunction and neuronal cell loss. Environmental toxins influence PD onset (Rajput 2001) and are also suggested to be involved in atypical parkinsonian syndromes (Caparros-Lefebvre and Lees 2005) and progressive supranuclear palsy (PSP) (Davis et al. 1988). Furthermore, the age-related neurodegenerative disorders are commonly characterised by the accumulation of insoluble neurotoxic ubiquinated proteins (Johnson 2000). The neurotoxin hypothesis states that detoxification enzymes can influence susceptibility to PD, but recently another mechanism has also been recognised as important for detoxification of the brain. Proteins that are involved in cellular efflux prevent penetration into the brain by various potentially toxic compounds or their accumulation. They include P-glycoprotein (P-gp) (Cordon-Cardo et al. 1989) and multidrug resistance associated protein (MRP). At the blood–brain barrier (BBB), P-gp is expressed in a high concentration at the luminal side of the brain vascular endothelium (Demeule et al. 2001) and functions as an efflux pump by translocating a substrate to the extracellular compartment. P-gp in the endothelial cells of the choroid plexus has a transport direction towards the CSF (de Lange 2004). P-gp could thus play a role in brain detoxification via different routes.
The P-gp transporter is associated with the multidrug resistance gene (MDR1). Interestingly, a significant association was found between parkinsonian patients exposed to pesticides and C3435T polymorphism of the MDR1 gene, related to lower P-gp function (Drozdzik et al. 2003; Furuno et al. 2002). Thus the mutation of the MDR1 gene with diminished P-gp function increases the vulnerability to the damaging effects of pesticides. It is assumed that neurotoxic substances such as certain pesticides are substrates of P-gp (Bain and LeBlanc 1996) and CNS exposure to such agents may continue to cause neurodegenerative diseases.
In a pilot study (Kortekaas et al. 2005), impaired BBB P-gp transport was found in the midbrain of five PD patients compared to five healthy control subjects, measured with [11C]-verapamil PET, pointing to a role of P-gp in the brain to prevent accumulation of toxic substances causing PD neurodegeneration. This finding, however, could not be replicated in a study that measured P-gp function with [11C]-(R)-verapamil PET in ten early stage PD patients compared to healthy controls (Bartels et al. 2007).
Decreased expression of P-gp in BBB vasculature has been found in other neurodegenerative diseases, like Alzheimer’s disease (AD) (Vogelgesang et al. 2001) and Creutzfeldt–Jakob disease (CJD) (Vogelgesang et al. 2006a). In AD, P-gp up-regulation in early pathogenesis was suggested as a compensatory mechanism to increase the clearance of harmful proteins, while at later disease stages P-gp expression was lost (Vogelgesang et al. 2001).
We hypothesize that P-gp-mediated transport out of the brain is involved in clearance of harmful substances and dysfunction of this system also occurs in late stage parkinsonian neurodegeneration. In the present study, we performed [11C]-verapamil-PET brain imaging of new groups of de novo PD patients, PD patients in more advanced disease stages, progressive supranuclear palsy (PSP), and multisystem atrophy (MSA) patients and a healthy control group, to study regional BBB P-gp function in patients with different parkinsonian pathology. PET with [11C]-verapamil has been shown to be an appropriate methodology for the in vivo assessment of the functional P-gp status in human BBB (Hendrikse et al. 1999). The distribution volume (DV) of the P-gp substrate verapamil can be taken as a measure of P-gp efflux function, higher [11C]-verapamil uptake meaning less P-gp efflux function. The effect of the MDR1 gene polymorphism was additionally investigated.
Materials and methods
Patients were selected from the Movement Disorders Clinic of the University Medical Centre Groningen; healthy volunteers were asked to participate by advertisement. The study was approved by the Medical Ethics Committee of the University Medical Centre Groningen and all subjects gave their informed consent. PD was diagnosed according to the criteria of Gelb et al. (1999). Ten de novo PD patients (diagnosed in the past year and without PD medication), and ten PD patients in more advanced disease stage (Hoehn and Yahr stages 2–3) participated in the study (Table 1). Furthermore, five patients with PSP and four patients with MSA, compliant with the criteria for PSP or MSA according to the NINDS-SPSP international workshop (Litvan et al. 1996) and the consensus statement for the diagnosis of MSA (Gilman et al, 1999) were included. Nine healthy age-matched subjects, who did not use medication, participated as controls. Patients did not use known P-gp modulating agents [(cardiovascular drugs, antimalarial drugs, cyclosporine A, phenothiazines, hormones (e.g., tamoxifen)] and certain antibiotics such as cefoperazone, ceftriaxone, and erythromycine [see for a detailed list (Hendrikse et al. 2001)]. T1 weighted MRI scans were performed on all subjects and did not show abnormalities or significant atrophy of cortical regions.
[11C]-verapamil was synthesised as described before (Wegman et al. 2002). PET scans were performed with an ECAT EXACT HR + positron camera (Siemens/CTI, Knoxville, TN). After cannulation of the radial artery, all subjects underwent 1 h dynamic PET scanning consisting of 21 frames after injection of [11C]-verapamil (200–400 MBq). Serial arterial blood sampling to define the input function for 11[C]-verapamil was done using a computerised sampling programme; six remaining samples were drawn manually. These samples (collected at intervals of 10 min) were processed by high liquid chromatography to measure the fraction of unmetabolised parent compound. In this way the contribution to the total signal can be calculated. PET data were reconstructed to a 128 × 128 × 63 matrix with a plane separation of 2.425 and a bin size of 2.250 mm.
For anatomical demarcation, the frames 12–21 of the dynamic [11C]-verapamil scans were summated using Clinical Application Programming Package (CAPP; Siemens, Erlangen, Germany). On this summated image, CAPP regions of interest (ROIs) were manually drawn over the midbrain and whole brain to calculate distribution volume (DV) in the ROIs. Using Matlab (The Mathworks Inc., Natick, USA) and a linearization according to Logan (2000), starting at t = 5 min, DV images were constructed from the 11[C]-verapamil scans, which was done for the whole brain ROI as well as pixelwise to obtain parametric DV images. Logan analysis is a graphical method of analysis, applicable to ligands that bind reversibly to receptors or enzymes, calculating the DV for dynamic PET data before steady state is actually reached. For comparison of regional differences between the groups, parametric DV images were analysed using statistical Parametric Mapping (Friston et al. 1991) (SPM99, Wellcome Department of Cognitive Neurology, London, UK). SPM99 instead of the latest SPM version was used to compare the results with those of the pilot study (Kortekaas et al. 2005). Individual DV images were spatially normalised to the [11C]-verapamil DV template that was constructed in the pilot study. After spatial smoothing by convolution with a Gaussian kernel of 20 mm, a two-sample t test was done. To visualize the statistical parametric maps, the threshold was set to P < 0.001 uncorrected. Because higher variation in DV between individuals may render smaller differences between the groups statistically insignificant in SPM, t tests were repeated after global calculation of the DV images to 100 in SPM. We also used this SPM analysis method to compare our results with the previous pilot study (Kortekaas et al. 2005).
From each subject 10 ml blood was collected in an EDTA coated vial for determination of MDR1 C3435T polymorphism on exon 26. A polymerase chain reaction (PCR)-based restriction fragment length polymorphism assay was performed with the primers MDR1F 5′-TGCTGGTCCTGAAGTTGATCTGTAAC-3′ and MDR1R 5′-ACATTAGGCAGTGACTCGATGAAGGCA-3′. PCR was carried out with an initial denaturation of 12 min at 95°C followed by 30 cycles of denaturation at 94°C for 1 min, primer annealing for 1 min at 60°C, and 1 min extension at 70°C. When the mutation was present (3435T), digesting of the 248 bp PCR-product produced the 172-, 60 bp and 16-bp fragments. The digested PCR products were analysed on a 2% agarose gel with ethidium bromide staining. Whole brain verapamil DV of all subjects was plotted against the C3435T polymorphism (CC, CT and TT genotypes), and correlation coefficient of genotype with DV was calculated in all subjects and in the separate groups.
Results
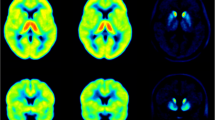
[11C]-verapamil uptake was high in the pituitary, ventricles and skin, moderate in grey matter and low in white matter and bone. Visual inspection of the scans revealed no obvious differences between the groups. The Logan analysis provides the DV of a tracer, and is defined by a ratio between the influx of the tracer K1 and the efflux out of the brain K2, of which the latter reflects the efflux function of P-gp. The influx K1 of [11C]-verapamil was of the same magnitude in all groups, which confirms that differences in DV reflect differences in P-gp efflux function. Mean DV in the more advanced PD group was 0.56 (SD 0,12), de novo PD showed 0.50 (SD 0,08), PSP 0.66 (SD 0,05), MSA 0.66 (SD 0,07) and controls 0.59 (SD 0,13). K1 in the PD group gave 0.037 (SD 0,013), PSP 0.038 (SD 0,005), MSA 0.036 (SD 0,006) and controls 0.036 (SD 0,006). Differences in DV between the groups were not statistically significant.
Pixel by pixel t test (P < 0.001 uncorrected) in SPM did not show increased midbrain [11C]-verapamil uptake in either of the PD groups as compared to the control group. The advanced PD group showed significantly increased 11[C]-verapamil uptake in frontal white matter regions compared to controls (SPM coordinates 34, 30, 26 and −16, 48, 12, near grey matter Brodmann areas 9 and 10, P corrected at cluster level 0.000, Fig. 1); a cluster with decreased uptake was seen in the cerebellar tonsils (maximum effect at coordinates 40, −54, −46). The de novo PD group had lower uptake in brainstem and cerebellar tonsils (brainstem coordinates 2, −26, −26 with P corrected at cluster level 0.000, Fig. 2) compared to the control group and did not show clusters with higher uptake. Plots of the local SPM responses showed a considerable separation of the groups, although there are some overlapping cases, where the PD groups show larger variation in local response values. Comparison of de novo and advanced PD groups revealed a cluster of pixels reflecting higher uptake in the advanced PD group in the anterior cingulate cortex (coordinates 4, 28, −6) and in the caudate head (coordinates 14, 14, 2 with P corrected at cluster level 0.01).
a SPM t test on MRI overlay showing P < 0.001. Increased [11C]-verapamil uptake in the frontal lobe in advanced PD patients compared to healthy controls; SPM coordinates 34, 30, 26 and −16, 48, 12 (Brodmann areas 9 and 10) with P corrected at cluster level 0.000. b Plot of the frontal effect (PD patients scan number 1–10 and controls 11–20) shows little overlap
a de novo PD patients showed lower brainstem [11C]-verapamil uptake in the brainstem compared to controls, P < 0.001; SPM coordinates 2, −26, −26 with P corrected at cluster level 0.000. b Plot of the brainstem effect shows more variation in PD de novo values (scan number 1–10) with some overlap with the control group (scan number 11–20)
In the PSP group, significantly increased uptake was seen in basal ganglia regions (maximum effect in lentiform nucleus, coordinates 26, −10, 6 with P corrected at cluster level 0.06, Fig. 3). When plotting the effect, one PSP patient did not show higher uptake compared to the healthy controls (Fig. 3). Notably, this was also the patient with shortest disease duration (<1 year) and only mild parkinsonian symptoms (UPDRS motor part score 12). The PSP group had also increased uptake in frontal regions compared both to controls and the advanced PD group, but this did not reach significance and plotting the effect showed high variance between the PSP patients. MSA patients did not show significant differences compared to controls, however after lowering the threshold to P < 0.01, also increased uptake in basal ganglia regions was seen with P corrected at cluster level 0.98 and uncorrected P at 0.056 in putamen (28, −6, −2). Plot of the SPM effect showed more variance between the MSA patients with one patient in the control range. This patient had lower disease severity compared to the other MSA patients, with 2 years disease duration and UPDRS motor score 24.
a PSP patients showed higher [11C]-verapamil uptake in lentiform nucleus and putamen compared to controls, P < 0.001; SPM coordinates 26, −10, 6 with P corrected at cluster level 0.06. b Plot of the basal ganglia effect shows higher values in four of the five PSP patients (scan number 1–5). PSP patient number 5 had shortest disease duration (<1 year)
All results did not remain statistically significant after correction for multiple comparisons in SPM (FDR correction with level of significance set at P < 0. 05) possibly due to the higher inter-subject variation. T-tests in SPM were repeated after global calculation of the DV images to 100, which showed comparable results and did not reveal additional foci with relative DV differences between the groups.
The frequencies of the determined MDR1 polymorphism in our study group did not differ from the frequencies seen in the general population (Tan et al. 2004). Furthermore, C3435T genotypes did not significantly correlate with the differences in [11C]-verapamil DV in the brain in all groups.
We compared [11C]-verapamil PET data of the present study with data of the previously published pilot study that was performed by our group. All subjects showed comparable K1 and DV values. Mean injected dose was lower in the pilot study with 111 MBq given as lowest dose; for a better signal-to-noise ratio, the cut-off dose for the current study was set at 200 MBq. The previous pilot control group showed relatively lower midbrain uptake compared to the nine control subjects of this study, which, however, only was shown in SPM after global calculation of the mean DV to 100. Neither group used medication nor was there a significant age difference between both the control groups, although the pilot group had one outlier of 86 years. We could not demonstrate a definite methodological explanation for the midbrain effect in the pilot control subjects. However in our opinion, global calculation of the mean may have affected the results in the midbrain area, which is a small region with a low uptake signal and is thereby prone to artefacts. Finally, because of the lower injected tracer dose, data of the previous pilot study were not further used for the present study.
Discussion
The results of this study do not support the idea of a primary dysfunctional BBB P-glycoprotein efflux system in the pathogenesis of Parkinson’s disease, but finds decreased P-gp function at later disease stages. This is in line with a most recent study that measured BBB P-gp function in mostly early stage PD patients using [11C]-(R)-verapamil, where higher variance in tracer uptake was seen in several regions in the PD group, but no significant decreased P-gp function was found (Bartels et al. 2007).
More advanced PD patients showed frontal regions with diminished P-gp function relative to normal controls and de novo PD patients. Regional frontal decreases in both advanced PD and advanced PSP possibly reflects the affected frontostriatal neuronal projections with frontal dysfunction in these disease stages (Green et al. 2002). The increased uptake lies in the white matter regions rather than the cortex. In general, white matter shows similar [11C]-verapamil uptake as grey matter. Involvement of white matter regions and vasculature in neurodegenerative disorders that can be seen as “proteinopathies”, involving accumulation of misfolded proteins, is a topic of important discussion. It was shown in vitro that β-amyloid is transported by P-gp (Kuhnke et al. 2007; Lam et al. 2001; Vogelgesang et al. 2006b). Interestingly, the deposition of Aβ1–40 in cerebral amyloid angiopathy (CAA), which is found in around 90% of AD patients, is predominantly found in the penetrating arterioles that supply the periventricular white matter (Lee and Markus 2006). Another study associated the failure of interstitial fluid drainage from the white matter in AD with the deposition of Aβ in the perivascular fluid drainage pathways (Roher et al. 2003). Thus, decreased P-gp function in white matter regions may influence protein removal and accumulation at sites more distant from the white matter. Furthermore, it is suggested that Lewy Body-related pathology initially involves the neuronal perikarya, dendrites, and axons, with abundantly present “Lewy axons” in the limbic subcortical white matter (Saito et al. 2003). These authors also find that impairment of axonal transport and synaptic transmission leads to the formation of Lewy Bodies, a hallmark of functional disturbance long before neuronal cell death. White matter P-gp dysfunction might also influence removal of toxic substances such as pesticides, which could cause harm to distant sites of the white matter after alterations of axonal transport, leading to “dying-back” patterns of neurodegeneration (Morfini et al. 2007).
In PD, greater disease severity and a more rapid neurodegenerative process have been associated with white matter hyperintensities (Piccini et al. 1995). However, although specific methodology or rating scales were not used to assess white matter pathology on the MRI’s in this study, we could not detect any visually apparent white matter hyperintensities in any subject.
Both de novo and more advanced PD patients showed lower [11C]-verapamil uptake in the cerebellum. The cerebellum is closely linked to midbrain nuclei, but is by itself not affected with progression of PD pathology (Braak and Braak 2000). Possibly, P-gp function in these regions is increased in PD, but does not deteriorate in later stages, as these regions are not vulnerable to PD pathology. On the other hand, in MSA cerebellar degeneration can be part of the disease spectrum. We did not find changed P-gp function in the cerebellum in the MSA patients. However, the MSA patients in this study did not show symptoms of cerebellar dysfunction and MRI scans did not show cerebellar atrophy.
PSP and MSA patients showed basal ganglia regions with increased [11C]-verapamil uptake, pointing at decreased P-gp function in regions with neuropathological features in these disorders. Brain atrophic changes are not likely to play a role in these results, because MRI scans did not show overt atrophy in these regions. Moreover, tissue loss would lead to decreased [11C]-verapamil uptake in these regions. PSP patients also showed decreased P-gp function in frontal regions. Although this result was not significant, plotting this effect showed higher variation between the PSP patients with one PSP patient in early disease stage who showed values overlapping with the controls (Fig. 3). These results may possibly point at regionally decreased P-gp function with advancing disease stage.
Regionally decreased P-gp function could thus occur not only in more advanced PD, but may also play a role in other neurodegenerative diseases with parkinsonism, and likely plays a role in advancing neurodegenerative processes in general. It has been argued that decreased cerebrovascular P-gp impairs the ability of the brain to expel excess proteins, and that the resulting accumulation of protein in cells could overwhelm cellular ubiquitin-proteasomal degradation (Vogelgesang et al. 2006a). P-gp was even found to interact actively with the proteasome complex, and a role for P-gp in the transport of proteasome-derived peptides was suggested (Begley et al. 2005). Loss of P-gp function may possibly also lead to increased accumulation of insoluble α-synuclein with ongoing neurodegeneration in PD. P-gp dysfunction in late disease stage may also contribute to neuronal damage due to increased accumulation of toxins. It is known that environmental factors causing damage, such as pesticides, are closely linked to mechanisms underlying the formation of α-synuclein pathology and PD-like neurodegeneration (Norris et al. 2007). Furthermore, it is recognised that the prevalence of dementia is higher in PD patients than in age-matched controls, which often is found to be defined by AD pathology in conjunction to the Lewy bodies (Burn 2006). Decreased P-gp function to expel proteins in advanced PD could also play a role in the co-existence of α-synuclein and β-amyloid in PD with dementia (PDD), a patient group that was not investigated in the present study.
In the study presented here, de novo PD patients showed lower [11C]-verapamil uptake compared to normal controls in the brainstem, which may indicate a regional up-regulation of P-gp function in early stage PD. The brainstem regions lies posterior to the pons, comprising the locus coeruleus and lying slightly superior to the dorsal motor vagal nucleus, a region that is affected early in PD pathology (Del et al. 2002), containing projection neurons of the intermediate reticular zone, coeruleus–subcoeruleus complex and caudal raphe nuclei.
A limitation of the methods, using [11C]-verapamil uptake as a measure of P-gp efflux function, is the low uptake signals of this tracer in the normal condition, as it is removed by P-gp. Intersubject variation in tracer uptake can be substantial, whereby small regional effects may be overlooked in the statistical comparison. On the other hand, global calculation can be applied to investigate regional patterns within disease groups rather than absolute P-gp measures. This should be applied with care, as small regions with low uptake signals may be prone to artefactual changes. In the case of the present study, the brainstem effect was also seen without proportional scaling in SPM, and is therefore more likely a significant result.
Initial up-regulation of P-gp expression or increase of P-gp function in reaction to neuronal damage may be associated with a neuroinflammatory process in Parkinson’s disease. In PD as well as in other neurodegenerative diseases, extensive microglia activation, the key event in neuroinflammation, is seen (Gerhard et al. 2001; Mcgeer and Mcgeer 1998, 2004). Microglia themselves express P-gp, which increases upon microglia activation (Langford et al. 2004). Several factors that are involved in inflammatory processes, like TNF-α, IL-6 and nitric oxide (NO) may increase P-gp function (Fernandez et al. 2004; Mcrae et al. 2003). Furthermore, Tan et al. (2002) showed that exposure of BBB endothelial cells to activated T-lymphocytes induced endothelial cell death, whereas P-gp expression and function was increased in surviving cells. The authors conclude that P-gp could play a regulatory role in promoting survival of cerebral endothelial cells and maintenance of BBB function. In conclusion, neuronal damage with a subsequent neuroinflammatory reaction could, by activating the P-gp system promote the clearance of the brain of potentially toxic compounds.
An initially compensatory mechanism with up-regulation of P-gp expression has also been suggested in the early pathogenesis of Alzheimer’s disease (AD). At later disease stages, P-gp expression in the capillaries was lost. P-gp in the brain could thus form a compensatory mechanism to increase clearance of neurotoxic substances that play a role in neurodegenerative diseases. A similar role for P-gp was also suggested in Creutzfeldt–Jakob Disease (CJD), where decreased P-gp expression was suggested to facilitate the accumulation of PrPSc prions (Vogelgesang et al. 2006a). Whether P-gp also transports α-synuclein, a major constituent of Lewy bodies that causes neurodegeneration in PD when aggregated, has so far not been investigated. Furthermore, it is known that P-gp contributes to the cellular efflux of some pesticides (Bain and LeBlanc 1996) and environmental toxins influence PD onset (Rajput, 2001). However, decreased P-gp function was not seen in de novo PD patients, indicating that impaired BBB P-gp efflux function does not play a primary role in the initiation of pathology in idiopathic PD.
The findings of our study could have implications in the therapeutic options in PD and other proteopathies. P-gp activity can be modulated by a variety of substances, but most studies focus on P-gp inhibition, e.g., in the prevention of multidrug resistance in oncological treatments (Tan et al. 2000). However, P-gp activity can also be up regulated, for example by St Johns worth or rifampicin (Fromm 2000; Hennessy et al. 2002). Selectively increasing P-gp mediated BBB efflux function would provide a possible novel therapeutic means to prevent further accumulation of insoluble toxic compounds or proteins leading to ongoing neurodegeneration.
We conclude that cerebrovascular P-gp function is regionally decreased with advanced stages in several parkinsonian neurodegenerative diseases, implying decreased regulatory and protective function of the BBB with ongoing neurodegeneration.
References
Bain LJ, LeBlanc GA (1996) Interaction of structurally diverse pesticides with the human MDR1 gene product P-glycoprotein. Toxicol Appl Pharmacol 141:288–298
Bartels AL, van Berckel BNM, Lubberink M, Luurtsema G, Lammertsma AA, Leenders KL (2007) Blood–brain barrier P-glycoprotein function is not impaired in early Parkinson’s disease. Final stage of review ed
Begley GS, Horvath AR, Taylor JC, Higgins CF (2005) Cytoplasmic domains of the transporter associated with antigen processing and P-glycoprotein interact with subunits of the proteasome. Mol Immunol 42:137–141
Braak H, Braak E (2000) Pathoanatomy of Parkinson’s disease. J Neurol 247:3–10
Burn DJ (2006) Parkinson’s disease dementia: what’s in a Lewy body? J Neural Transm Suppl 361–365
Caparros-Lefebvre D, Lees AJ (2005) Atypical unclassifiable parkinsonism on Guadeloupe: an environmental toxic hypothesis. Mov Disord 20(Suppl 12):S114–S118
Cordon-Cardo C, O’Brien JP, Casals D, Rittman-Grauer L, Biedler JL, Melamed MR, Bertino JR (1989) Multidrug-resistance gene (P-glycoprotein) is expressed by endothelial cells at blood–brain barrier sides. Proc Natl Acad Sci USA 86:695–698
Davis PH, Golbe LI, Duvoisin RC, Schoenberg BS (1988) Risk factors for progressive supranuclear palsy. Neurology 38:1546–1552
de Lange ECM (2004) Potential role of ABC transporters as a detoxification system at the blood-CSF barrier. Adv Drug Deliv Rev 56:1793–1809
Del TK, Rub U, de Vos RA, Bohl JR Braak H (2002) Where does parkinson disease pathology begin in the brain? J Neuropathol Exp Neurol 61:413–426
Demeule M, Labelle M, Regina A, Berthelet F, Beliveau R (2001) Isolation of endothelial cells from brain, lung, and kidney: Expression of the multidrug resistance P-glycoprotein isoforms. Biochem Biophys Res Commun 281:827–834
Drozdzik M, Bialecka M, Mysliwiec K, Honczarenko K, Stankiewicz J, Sych Z (2003) Polymorphism in the P-glycoprotein drug transporter MDR1 gene: a possible link between environmental and genetic factors in Parkinson’s disease. Pharmacogenetics 13:259–263
Fernandez C, Buyse M, German-Fattal M, Gimenez F (2004) Influence of the pro-inflammatory cytokines on P-glycoprotein expression and functionality. J Pharm Pharm Sci 7:359–371
Friston KJ, Frith CD, Liddle PF, Frackowiak RSJ (1991) Comparing functional (pet) images—the assessment of significant change. J Cereb Blood Flow Metab 11:690–699
Fromm MF (2000) P-glycoprotein: a defense mechanism limiting oral bioavailability and CNS accumulation of drugs. Int J Clin Pharmacol Ther 38:69–74
Furuno T, Landi MT, Ceroni M, Caporaso N, Bernucci I, Nappi G, Martignoni E, Schaeffeler E, Eichelbaum M, Schwab M, Zanger UM (2002) Expression polymorphism of the blood–brain barrier component P-glycoprotein (MDR1) in relation to Parkinson’s disease. Pharmacogenetics 12:529–534
Gelb DJ, Oliver E, Gilman S (1999) Diagnostic criteria for Parkinson disease. Arch Neurol 56:33–39
Gerhard A, Banati RB, Cagnin A, Brooks DJ (2001) In vivo imaging of activated microglia with [C-11]PK11195 positron emission tomography (PET) in idiopathic and atypical Parkinson’s disease. Neurology 56:A270
Gilman S, Low P, Quinn N, Albanese A, Ben-Shlomo Y, Fowler C, Kaufmann H, Klockgether T, Lang A, Lantos P, Litvan I, Mathias C, Oliver E, Robertson D, Schatz I, Wenning G (1999) Consensus on the diagnosis of multi-system atrophy. Neurologia 14:425–428
Green J, McDonald WM, Vitek JL, Evatt M, Freeman A, Haber M, Bakay RA, Triche S, Sirockman B, DeLong MR (2002) Cognitive impairments in advanced PD without dementia. Neurology 59:1320–1324
Hendrikse NH, Vaalburg W, De Vries EG, Van der Graaf WT, Willemsen AT (1999) Quantification of in-vivo P-glycoprotein facilitated transport in the blood–brain barrier. J Nucl Med 40:261P–262P
Hendrikse NH, Bart J, De Vries EGE, Groen HJM, Van der Graaf WTA, Vaalburg W (2001) P-glycoprotein at the blood–brain barrier and analysis of drug transport with positron-emission tomography. J Clin Pharmacol 48S–54S
Hennessy M, Kelleher D, Spiers JP, Barry M, Kavanagh P, Back D, Mulcahy F, Feely J (2002) St Johns wort increases expression of P-glycoprotein: implications for drug interactions. Br J Clin Pharmacol 53:75–82
Johnson WG (2000) Late-onset neurodegenerative diseases–the role of protein insolubility. J Anat 196(Pt 4):609–616
Kortekaas R, Leenders KL, van Oostrom JCH, Vaalburg W, Bart J, Willemsen ATM, Hendrikse NH (2005) Blood–brain barrier dysfunction in Parkinsonian midbrain in vivo. Ann Neurol 57:176–179
Kuhnke D, Jedlitschky G, Grube M, Krohn M, Jucker M, Mosyagin I, Cascorbi I, Walker LC, Kroemer HK, Warzok RW, Vogelgesang S (2007) MDR1-P-Glycoprotein (ABCB1) mediates transport of Alzheimer’s amyloid-beta peptides-implications for the mechanisms of Abeta clearance at the blood–brain Barrier. Brain Pathol (4):347-353
Lam FC, Liu R, Lu P, Shapiro AB, Renoir JM, Sharom FJ, Reiner PB (2001) beta-Amyloid efflux mediated by p-glycoprotein. J Neurochem 76:1121–1128
Langford D, Grigorian A, Hurford R, Adame A, Ellis RJ, Hansen L, Masliah E (2004) Altered P-glycoprotein expression in AIDS patients with HIV encephalitis. J Neuropathol Exp Neurol 63:1038–1047
Lee JM, Markus HS (2006) Does the white matter matter in Alzheimer disease and cerebral amyloid angiopathy? Neurology 66:6–7
Litvan I, Agid Y, Calne D, Campbell G, Dubois B, Duvoisin RC, Goetz CG, Golbe LI, Grafman J, Growdon JH, Hallett M, Jankovic J, Quinn NP, Tolosa E, Zee DS, Chase TN, FitzGibbon EJ, Hall Z, Juncos J, Nelson KB, Oliver E, Pramstaller P, Reich SG, Verny M (1996) Clinical research criteria for the diagnosis of progressive supranuclear palsy (Steele–Richardson–Olszewski syndrome): report of the NINDS-SPSP International Workshop. Neurology 47:1–9
Logan J (2000) Graphical analysis of PET data applied to reversible and irreversible tracers. Nucl Med Biol 27:661–670
Mcgeer PL, Mcgeer EG (1998) Glial cell reactions in neurodegenerative diseases: pathophysiology and therapeutic interventions. Alzheimer Dis Assoc Disord 12:S1–S6
Mcgeer PL, Mcgeer EG (2004) Inflammation and neurodegeneration in Parkinson’s disease. Parkinsonism Relat Disord 10:S3–S7
Mcrae MP, Brouwer KLR, Kashuba ADM (2003) Cytokine regulation of P-glycoprotein. Drug Metab Rev 35:19–33
Morfini G, Pigino G, Opalach K, Serulle Y, Moreira JE, Sugimori M, Llinas RR, Brady ST (2007) 1-Methyl-4-phenylpyridinium affects fast axonal transport by activation of caspase and protein kinase C. Proc Natl Acad Sci USA 104:2442–2447
Norris EH, Uryu K, Leight S, Giasson BI, Trojanowski JQ, Lee VM (2007) Pesticide exposure exacerbates alpha-synucleinopathy in an A53T transgenic mouse model. Am J Pathol 170:658–666
Piccini P, Pavese N, Canapicchi R, Paoli C, Del DP, Puglioli M, Rossi G, Bonuccelli U (1995) White matter hyperintensities in Parkinson’s disease. Clin Correlat Arch Neurol 52:191–194
Rajput AH (2001) Environmental toxins accelerate Parkinson’s disease onset. Neurology 56:4–5
Roher AE, Kuo YM, Esh C, Knebel C, Weiss N, Kalback W, Luehrs DC, Childress JL, Beach TG, Weller RO, Kokjohn TA (2003) Cortical and leptomeningeal cerebrovascular amyloid and white matter pathology in Alzheimer’s disease. Mol Med 9:112–122
Saito Y, Kawashima A, Ruberu NN, Fujiwara H, Koyama S, Sawabe M, Arai T, Nagura H, Yamanouchi H, Hasegawa M, Iwatsubo T, Murayama S (2003) Accumulation of phosphorylated alpha-synuclein in aging human brain. J Neuropathol Exp Neurol 62:644–654
Tan EK, Drozdzik M, Bialecka M, Honczarenko K, Klodowska-Duda G, Teo Y, Tang K, Wong LP, Chong SS, Tan C, Yew K, Zhao Y, Lee CGL (2004) Analysis of MDR1 haplotypes in Parkinson’s disease in a white population. Neurosci Lett 372:240–244
Tan B, Piwnica-Worms D, Ratner L (2000) Multidrug resistance transporters and modulation. Curr Opin Oncol 12:450–458
Tan KH, Purcell WM, Heales SJR, Mcleod JD, Hurst RD (2002) Activated T cells modulate P-glycoprotein expression in an in vitro model of the blood–brain barrier. J Physiol (London) 539:89P
Vogelgesang S, Cascorbi I, Kroemer HK, Schroeder E, Pahnke J, Siegmund W, Keil C, Warzok RW, Walker LC (2001) Deposition of amyloid is inversely correlated with the expression of p-glycoprotein—implications on the possibility of prevention of Alzheimer’s disease. Acta Neuropathol 102:545
Vogelgesang S, Glatzel M, Walker LC, Kroemer HK, Aguzzi A, Warzok RW (2006a) Cerebrovascular P-glycoprotein expression is decreased in Creutzfeldt–Jakob disease. Acta Neuropathol (Berl) 111:436–443
Vogelgesang S, Kuhnke D, Jedlitschky G, Jucker M, Mosyagin I, Pahnke J, Cascorbi I, Kroemer HK, Walker LC, Warzok RW (2006b) P-glycoprotein (ABCB1) mediates transport of Alzheimer’s beta-amyloid peptides. Acta Neuropathol 112:365–367
Wegman TD, Maas B, Elsinga PH, Vaalburg W (2002) An improved method for the preparation of [C-11]verapamil. Appl Radiat Isot 57:505–507
Acknowledgments
The Michael J Fox Foundation for Parkinson’s research, USA and the International Parkinson Foundation, the Netherlands are gratefully acknowledged for their financial support of this study. Staff of the central laboratory of the University Medical Centre Groningen is thanked for determination of the MDR1 C3435T genotype.
Conflict of interest statement
The authors report no conflicts of interest. The study was approved by the Medical Ethics Committee of the University Medical Centre Groningen and all subjects gave written informed consent.
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This is an open access article distributed under the terms of the Creative Commons Attribution Noncommercial License (https://creativecommons.org/licenses/by-nc/2.0), which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
About this article
Cite this article
Bartels, A.L., Willemsen, A.T.M., Kortekaas, R. et al. Decreased blood–brain barrier P-glycoprotein function in the progression of Parkinson’s disease, PSP and MSA. J Neural Transm 115, 1001–1009 (2008). https://doi.org/10.1007/s00702-008-0030-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00702-008-0030-y