Abstract
Background
We have previously proposed that pineal cysts (PCs) may result in crowding of the pineal recess, causing symptoms due to compression of the internal cerebral veins and central venous hypertension. In the present study, we compared clinical outcome of different treatment modalities in symptomatic individuals with non-hydrocephalic PCs.
Methods
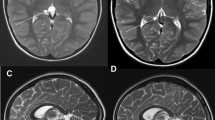
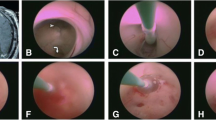
The study included all patients managed surgically for non-hydrocephalic PCs in our Department of Neurosurgery over a 10-year period. We applied a questionnaire to determine occurrence of symptoms before and after surgery, which allowed the use of a grading scale for symptom severity. Magnetic resonance imaging (MRI) biomarkers indicative of central venous hypertension were assessed before and after surgery.
Results
Relief of symptoms after surgery was most efficiently obtained by complete microsurgical cyst removal [n = 15; no (0/15), some (1/15) or marked (14/15) improvement], and to a lesser extent by microsurgical cyst fenestration [n = 6; no (2/6), some (4/6) or marked (0/6) improvement]. Shunt surgery was not successful [n = 6; no (5/6), some (1/6) or marked (0/6) improvement]. In all patients, the proposed MRI biomarkers gave evidence of central venous hypertension (PC grades 2–4).
Conclusions
Microsurgical cyst removal provided marked symptom relief in symptomatic individuals with non-hydrocephalic PCs and MRI biomarkers of central venous hypertension. The hypothesis that PC-induced crowding of the pineal recess may compromise venous run-off and induce a central venous hypertension syndrome deserves further study.




Similar content being viewed by others
References
Al-Holou WN, Garton HJ, Muraszko KM, Ibrahim M, Maher CO (2009) Prevalence of pineal cysts in children and young adults. Clinical article. J Neurosurg Pediatr 4:230–236
Al-Holou WN, Maher CO, Muraszko KM, Garton HJ (2010) The natural history of pineal cysts in children and young adults. J Neurosurg Pediatr 5:162–166
Al-Holou WN, Terman SW, Kilburg C, Garton HJ, Muraszko KM, Chandler WF, Ibrahim M, Maher CO (2011) Prevalence and natural history of pineal cysts in adults. J Neurosurg 115:1106–1114
Berhouma M, Ni H, Vallee B (2013) The endoscopic intraventricular management of pineal cysts: a minimally invasive modus operandi. Acta Neurochir (Wien) 155:1901–1905
Ducreux D, Oppenheim C, Vandamme X, Dormont D, Samson Y, Rancurel G, Cosnard G, Marsault C (2001) Diffusion-weighted imaging patterns of brain damage associated with cerebral venous thrombosis. AJNR Am J Neuroradiol 22:261–268
Eide PK (2006) A new method for processing of continuous intracranial pressure signals. Med Eng Phys 28:579–587
Eide PK, Eidsvaag VA, Nagelhus EA, Hansson HA (2016) Cortical astrogliosis and increased perivascular aquaporin-4 in idiopathic intracranial hypertension. Brain Res 1644:161–175
Eide PK, Kerty E (2011) Static and pulsatile intracranial pressure in idiopathic intracranial hypertension. Clin Neurol Neurosurg 113:123–128
Eide PK, Pripp AH, Ringstad GA (2016) Magnetic resonance imaging biomarkers indicate a central venous hypertension syndrome in patients with symptomatic pineal cysts. J Neurol Sci 363:207–216
Eide PK, Ringstad G (2016) Increased pulsatile intracranial pressure in patients with symptomatic pineal cysts and magnetic resonance imaging biomarkers indicative of central venous hypertension. J Neurol Sci 367:247–255
Eide PK, Sorteberg W (2008) Changes in intracranial pulse pressure amplitudes after shunt implantation and adjustment of shunt valve opening pressure in normal pressure hydrocephalus. Acta Neurochir (Wein) 150:1141–1147, discussion 1147
Eide PK, Sorteberg W (2010) Diagnostic intracranial pressure monitoring and surgical management in idiopathic normal pressure hydrocephalus: a 6-year review of 214 patients. Neurosurgery 66:80–91
Jakola AS, Bartek J Jr, Mathiesen T (2013) Venous complications in supracerebellar infratentorial approach. Acta Neurochir (Wien) 155:477–478
Kalani MY, Wilson DA, Koechlin NO, Abuhusain HJ, Dlouhy BJ, Gunawardena MP, Nozue-Okada K, Teo C (2015) Pineal cyst resection in the absence of ventriculomegaly or Parinaud’s syndrome: clinical outcomes and implications for patient selection. J Neurosurg 123:352–356
Karadas O, Ipekdal IH, Ulas UH, Odabasi Z (2012) Nocturnal headache associated with melatonin deficiency due to a pineal gland cyst. J Clin Neurosci 19:330–332
Klein P, Rubinstein LJ (1989) Benign symptomatic glial cysts of the pineal gland: a report of seven cases and review of the literature. J Neurol Neurosurg Psychiatry 52:991–995
Krause F (1926) Operative freilegung der vierhiigel, nebst Beobachtungen tiber hirndruck und dekompression. Zbl Chir 53:2812–2819
Le Bihan D (2013) Apparent diffusion coefficient and beyond: what diffusion MR imaging can tell us about tissue structure. Radiology 268:318–322
Lindroos AC, Niiya T, Randell T, Romani R, Hernesniemi J, Niemi T (2010) Sitting position for removal of pineal region lesions: the Helsinki experience. World Neurosurg 74:505–513
Majovsky M, Netuka D, Benes V (2016) Clinical management of pineal cysts: a worldwide online survey. Acta Neurochir (Wien) 158:663–669
Mandera M, Marcol W, Bierzynska-Macyszyn G, Kluczewska E (2003) Pineal cysts in childhood. Childs Nerv Syst 19:750–755
Menovsky T, De Ridder D, Grotenhuis JA (2011) Non-specific symptoms related to pineal cysts. Minim Invasive Neurosurg 54:50
Meyer S, Oberkircher N, Boing A, Larsen A, Eymann R, Kutschke G (2013) Disturbance in melatonin metabolism as a causative factor for recurrent headaches in a girl with a pineal cyst? Acta Paediatr 102:e51–e52
Michielsen G, Benoit Y, Baert E, Meire F, Caemaert J (2002) Symptomatic pineal cysts: clinical manifestations and management. Acta Neurochir (Wien) 144:233–242, discussion 242
Peres MF, Zukerman E, Porto PP, Brandt RA (2004) Headaches and pineal cyst: a (more than) coincidental relationship? Headache 44:929–930
Pu Y, Mahankali S, Hou J, Li J, Lancaster JL, Gao JH, Appelbaum DE, Fox PT (2007) High prevalence of pineal cysts in healthy adults demonstrated by high-resolution, noncontrast brain MR imaging. AJNR Am J Neuroradiol 28:1706–1709
Stam J (2005) Thrombosis of the cerebral veins and sinuses. N Engl J Med 352:1791–1798
Stein BM (1971) The infratentorial supracerebellar approach to pineal lesions. J Neurosurg 35:197–202
Acknowledgments
The authors thank Are Hugo Pripp, PhD, Department of Biostatistics, Epidemiology and Health Economics, Oslo University Hospital, Oslo, for statistical help during preparation of this paper.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
No funding was received for this research.
Conflicts of interest
P.K.E. has a financial interest in the software company (dPCom AS, Oslo) manufacturing the software (Sensometrics Software) used for analysis of the ICP recordings. G.R. reports no disclosures.
Ethical approval
The current patient cohort was retrieved from a larger study of PC management within the department, approved by The Regional Ethics Committee, REK South-East (2014/636) and Oslo University Hospital (2014/8138).
Informed consent
For this study formal consent was not required.
Rights and permissions
About this article
Cite this article
Eide, P.K., Ringstad, G. Results of surgery in symptomatic non-hydrocephalic pineal cysts: role of magnetic resonance imaging biomarkers indicative of central venous hypertension. Acta Neurochir 159, 349–361 (2017). https://doi.org/10.1007/s00701-016-3029-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-016-3029-4