Abstract
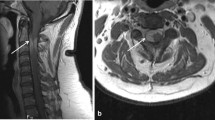
Idiopathic spinal cord herniation (ISCH) is a rare spinal disease, in which chronic cerebrospinal fluid pulsations push the arachnoid and adjacent thoracic spinal cord region through an antero-lateral dural defect of congenital, post-traumatic, or inflammatory/erosive origin. Symptomatic patients commonly present around the 5th decade of life with slowly progressive myelopathy. Diagnosis relies on high-resolution magnetic resonance imaging. Stable mild cases may be observed, whereas in progressive symptomatic situations, surgical spinal cord reposition and dural defect repair with a dural patch is the preferred treatment. We present a case of ISCH at T5/6 and a review the literature.




Similar content being viewed by others
References
Barrenechea IJ, Lesser JB, Gidekel AL, Turjanski L, Perin NI (2006) Diagnosis and treatment of spinal cord herniation: a combined experience. J Neurosurg Spine 5(4):294–302
Batzdorf U, Holly LT (2012) Idiopathic thoracic spinal cord herniation: report of 10 patients and description of surgical approach. J Spinal Disord Tech 25(3):157–162
Hawasli AH, Ray WZ, Wright NM (2014) Symptomatic thoracic spinal cord herniation: case series and technical report. Neurosurgery 10(Suppl 3):E498–E504
Martinez-Del-Campo E, Moon K, Kalb S, Soriano-Baron H, Theodore N (2015) Surgical management of a patient with thoracic spinal cord herniation: technical case report and review. Neurosurgery 77:E492–E499
Prada F, Saladino A, Giombini S, Erbetta A, Saini M, DiMeco F, Lodrini S (2012) Spinal cord herniation: management and outcome in a series of 12 consecutive patients and review of the literature. Acta Neurochir (Wein) 154(4):723–730
Najjar MW, Baeesa SS, Lingawi SS (2004) Idiopathic spinal cord herniation: a new theory of pathogenesis. Surg Neurol 62(2):161–170
Maira G, Denaro L, Doglietto F, Mangiola A, Colosimo C (2006) Idiopathic spinal cord herniation: diagnostic, surgical, and follow-up data obtained in five cases. J Neurosurg Spine 4(1):10–19
Imagama S, Matsuyama Y, Sakai Y, Nakamura H, Katayama Y, Ito Z, Wakao N, Sato K, Kamiya M, Kato F, Yukawa Y, Miura Y, Yoshihara H, Suzuki K, Ando K, Hirano K, Tauchi R, Muramoto A, Ishiguro N (2009) Image classification of idiopathic spinal cord herniation based on symptom severity and surgical outcome: a multicenter study. J Neurosurg Spine 11(3):310–319
Samuel N, Goldstein CL, Santaguida C, Fehlings MG (2015) Spontaneous resolution of idiopathic thoracic spinal cord herniation: case report. J Neurosurg Spine 23(3):306–308
Novak K, Widhalm G, de Camargo AB, Perin N, Jallo G, Knosp E, Deletis V (2012) The value of intraoperative motor evoked potential monitoring during surgical intervention for thoracic idiopathic spinal cord herniation. J Neurosurg Spine 16(2):114–126
Nakamura M, Fujiyoshi K, Tsuji O, Watanabe K, Tsuji T, Ishii K, Matsumoto M, Toyama Y, Chiba K (2011) Long-term surgical outcomes of idiopathic spinal cord herniation. J Orthop Sci 16(4):347–351
Selviaridis P, Balogiannis I, Foroglou N, Hatzisotiriou A, Patsalas I (2009) Spontaneous spinal cord herniation: recurrence after 10 years. Spine J 9(3):e17–e19
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Informed patient consent
The patient has consented to the submission of the case report for submission to the journal.
Additional information
Comment
Herniation of the spinal cord is a rarely encountered cause of myelopathy. The most common manifestation at thoracic level is the Brown-Sequard syndrome from an anterior cord herniation, occurring spontaneously or after trauma. Dorsally directed cord herniation characteristically also occurs, as a result of previous surgery, at cervical levels and may include radicular symptoms. A delay of several years to decades between the clinical presentation and any antecedent trauma or spinal surgery should be taken into account. Deficits are progressive and, with surgical intervention, recovery is often excellent. Imaging studies show typical, even though often overlooked signs suggestive of transdural spinal cord herniation, including: a small rotated portion of the spinal cord displaced ventrally or dorsally at the thoracolumbar levels, or displaced dorsally at the cervical level, and a perilesional communicating, apparently dilated, CSF space.
The authors here present a case successfully treated and thoroughly review the pertinent literature. This manuscript also provides interesting illustrations and practical suggestions on the management of this rare condition.
Alfredo Conti
Messina, Italy
Rights and permissions
About this article
Cite this article
Payer, M., Zumsteg, D., De Tribolet, N. et al. Surgical management of thoracic idiopathic spinal cord herniation. Technical case report and review. Acta Neurochir 158, 1579–1582 (2016). https://doi.org/10.1007/s00701-016-2840-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-016-2840-2