Abstract
Background
Corrective craniosynostosis surgery is often associated with a large amount of blood loss and metabolic disturbances. In the present study, we investigated the severity, duration of metabolic disturbances, and causal risk factors in infants.
Methods
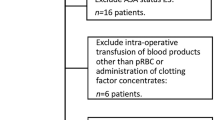
A retrospective analysis was performed of 36 infants who underwent craniosynostosis surgery. We analyzed the following: demographics, duration of surgery, intraoperative blood loss, RBC, FFP and fluids transfused, urine output, hemodynamic parameters, and electrolyte and base deficit (BD) values. The lowest intraoperative BD value and time required (period I: <6 h; period II: 6–12 h; period III: >12 h) for BD values to return to normal (-4 to +2) in the postoperative period were determined. In addition, we recorded the postoperative length of stay in the ICU and hospital, postoperative blood loss, and early complications.
Results
We detected that 88 % of the patients had subnormal BD levels and 22 % had metabolic acidosis. The lowest average BD measured during the operation was -8.4 ± 2.6 mmol/l. We carried out a multiple regression analysis, which revealed that lower BD values were associated with a longer duration of hypotension (p = 0.002, R2 = 0.453) and greater intraoperative blood loss (p = 0.002, R2 = 0.674). We examined the amount of intraoperative blood loss and found that that there were fewer blood product transfusions in period I patients and longer hypotensive episodes in period III patients. Also, a negative correlation was detected between the lowest intraoperative BD value with ICU duration (p = 0.004, r = -0.466) and hospital stay (p < 0.001, r = -0.764).
Conclusion
Almost all patients developed intraoperative negative BD, which was prolonged in the postoperative period. The most important risk factors for developing negative BD are the amount of blood loss and duration of hypotension.



Similar content being viewed by others
References
Aviv RI, Rodger E, Hall CM (2002) Craniosynostosis. Clin Radiol 57:93–102
Choi AY, Ahmad NS, de Beer DA (2010) Metabolic changes during major craniofacial surgery. Paediatr Anaesth 20:851–855
Goobie SM, Meier PM, Pereira LM, McGowan FX, Prescilla RP, Scharp LA, Rogers GF, Proctor MR, Meara JG, Soriano SG, Zurakowski D, Sethna NF (2011) Efficacy of tranexamic acid in pediatric craniosynostosis surgery: a double-blind, placebo-controlled trial. Anesthesiology 114:862–871
Hughes C, Thomas K, Johnson D, Das S (2013) Anesthesia for surgery related to craniosynostosis: a review. Part 2. Paediatr Anaesth 23:22–27
Kearney RA, Rosales JK, Howes WJ (1989) Craniosynostosis: an assessment of blood loss and transfusion practices. Can J Anaesth 36:473–477
Lee HQ, Hutson JM, Wray AC, Lo PA, Chong DK, Holmes AD, Greensmith AL (2012) Analysis of morbidity and mortality in surgical management of craniosynostosis. J Craniofac Surg 23:1256–1261
Persing JA (2008) MOC-PS(SM) CME article: management considerations in the treatment of craniosynostosis. Plast Reconstr Surg 121(4 Suppl):1–11
Stricker PA, Shaw TL, Desouza DG, Hernandez SV, Bartlett SP, Friedman DF, Sesok-Pizzini DA, Jobes DR (2010) Blood loss, replacement, and associated morbidity in infants and children undergoing craniofacial surgery. Paediatr Anaesth 20:150–159
Soldin J, Brugnara C, Hicks J (1999) Pediatric Reference Ranges, 3rd edn. AACC Press, Washington, DC
Thomas K, Hughes C, Johnson D, Das S (2012) Anesthesia for surgery related to craniosynostosis: a review. Part 1. Pediatr Anesth 22:1033–1041
Tuncbilek G, Vargel I, Erdem A, Mavili ME, Benli K, Erk Y (2005) Blood loss and transfusion rates during repair of craniofacial deformities. J Craniofac Surg 16:59–62
van Uitert A, Megens JH, Breugem CC, Stubenitsky BM, Han KS, de Graaff JC (2011) Factors influencing blood loss and allogeneic blood transfusion practice in craniosynostosis surgery. Paediatr Anaesth 21:1192–1197
Acknowledgments
The authors are grateful to Mr. David F. Chapman, who edited the language of this study.
Declaration of interest and funding
All authors certify that they have NO affiliations with or involvement in any organization or entity with any financial interest (such as honoraria; educational grants; participation in speakers’ bureaus; membership, employment, consultancies, stock ownership, or other equity interest; and expert testimony or patent-licensing arrangements), or non-financial interest (such as personal or professional relationships, affiliations, knowledge or beliefs) in the subject matter or materials discussed in this manuscript.
Details of author contributions
Achmet Ali: Design methods, data collection, data analysis, administration of study for the ethics committee and local authority, statistical analysis, and drafting the article.
Burcu Basaran: Data collection and analysis.
Gamze Tanirgan: Data analysis.
Aydin Aydoseli: Data collection.
Pulat Akin Sabanci: Data collection.
Altay Sencer: Data collection and analysis.
Lutfu Telci: Method design, critical revision, and approval of the final version to be published.
Ibrahim Ozkan Akinci: Design methods, data analysis, and drafting the article.
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Additional information
Comments
The management of prolonged anesthesia and blood loss associated with complex surgical treatments in infants with craniosynostosis remains an extraordinary challenge for the multidisciplinary team involved in the care of these patients. The metabolic disturbances that occur during the perioperative period for pediatric craniofacial surgery including acid-base and electrolyte derangement seem to be primarily related to blood loss and the resulting infusion of crystalloids and blood products. Notably, it has been demonstrated that, in the perioperative period, an increase in plasma potassium often occurs in patients in whom blood is transfused as a result of the potassium contained in packed cells stored for longer than 2 weeks [2]. Metabolic acidosis is a common complication, and there is a statistically significant relationship between the maximum base deficit and total volume of blood and colloid or crystalloid solutions administered intraoperatively. An interesting finding was that in 25 % of patients, the initial base deficit before surgery was significant and could be explained by ketoacidosis developing as a consequence of preoperative starvation [1].
The present study corroborates previous observations confirming that perioperative metabolic monitoring is as important as hemodynamic monitoring. Almost all patients develop intraoperative metabolic acidosis, and this condition is long lasting in the postoperative period. The most important risk factors are the amount of blood loss, hypotension, as well as excessive and inadequate fluid replacement and blood transfusion. A comprehensive recognition and management of metabolic disturbances and a multimodal patient blood management strategy are crucial to safely managing the anemia and coagulopathy associated with intraoperative blood loss during pediatric craniotomies and craniofacial surgery [3].
References
1. Choi AY, Ahmad NS, de Beer DA (2010) Metabolic changes during major craniofacial surgery. Paediatr Anaesth 20:851-855
2. Goobie SM, Haas T (2014) Bleeding management for pediatric craniotomies and craniofacial surgery. Paediatr Anaesth 24:678-689
3. Hughes C, Thomas K, Johnson D, Das S (2013) Anesthesia for surgery related to craniosynostosis: a review. Part 2. Paediatr Anaesth 23:22-27
Alfredo Conti
Messina, Italy
Ali and colleague retrospectively assessed metabolic changes and factors influencing base deficit (BD) in 36 infants undergoing craniosynostosis surgery. They found that almost all patients developed BD intraoperatively, continuing also postoperatively. The most important risk factors were a large amount of blood loss and the duration of arterial hypotension.
Even though these results are not surprising, and BD is only one parameter in intra- and postoperative monitoring, the results highlight the importance of adequate perioperative hemodynamic and metabolic monitoring, especially when performing surgery in infants with the potential to loose significant amounts of blood within a short period of time. We fully agree with the authors that the reduction of blood loss, the prevention of arterial hypotension, and an adequate regimen of substituting red blood cells as well as fresh frozen plasma are essential to reduce the risk of 22 intra- and postoperative complications. The same is true for the maintenance of normothermia and normoglycemia and for avoiding electrolyte disturbances.
Marcus Reinges and Jan-Falco Wilbrand
Giessen, Germany
Rights and permissions
About this article
Cite this article
Ali, A., Basaran, B., Tanirgan, G. et al. Metabolic changes and factors influencing base deficit in infants undergoing craniosynostosis surgery: a retrospective study. Acta Neurochir 157, 1197–1204 (2015). https://doi.org/10.1007/s00701-015-2441-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-015-2441-5