Abstract
Although surgical smoke contains potentially hazardous substances, such as cellular material, blood fragments, microorganisms, toxic gases and vapors, many operating rooms (ORs) do not provide protection from exposure to it. This article reviews the hazards of surgical smoke and the means of protecting OR personnel. Our objectives are to promote surgeons’ acceptance to adopt measures to minimize the hazards. Depending on its components, surgical smoke can increase the risk of acute and chronic pulmonary conditions, cause acute headaches; irritation and soreness of the eyes, nose and throat; dermatitis and colic. Transmission of infectious disease may occur if bacterial or viral fragments present in the smoke are inhaled. The presence of carcinogens in surgical smoke and their mutagenic effects are also of concern. This review summarizes previously published reports and data regarding the toxic components of surgical smoke, the possible adverse effects on the health of operating room personnel and measures that can be used to minimize exposure to prevent respiratory problems. To reduce the hazards, surgical smoke should be removed by an evacuation system. Surgeons should assess the potential dangers of surgical smoke and encourage the use of evacuation devices to minimize potential health hazards to both themselves and other OR personnel.

Similar content being viewed by others
References
Cushing H. Electro-surgery as an aid to the removal of intracranial tumors. With a preliminary note on a new surgical-current generator by W.T. Bovie, Ph.D., Chicago. Surg Gynecol Obstet. 1928;47:751–84.
NIOSH, Health Hazard Evaluation Report. HETA 85-126-1932, 1988. p. 2.
Hensman C, Baty D, Willis RG, Cuschieri A. Chemical composition of smoke produced by high-frequency electrosurgery in a closed gaseous environment: an in vitro study. Surg Endosc. 1998;12:1017–9.
Beebe DS, Swica H, Carlson N, Palahniuk RJ, Goodale RL. High levels of carbon monoxide are produced by electro-cautery of tissue during laparoscopic cholecystectomy. Anesth Analg. 1993;77:338–41.
Hensman C, Newman EL, Shimi SM, Cuschieri A. Cytotoxicity of electro-surgical smoke produced in an anoxic environment. Am J Surg. 1998;175:240–1.
Brüske-Hohlfeld I, Preissler G, Jauch KW, Pitz M, Nowak D, Peters A, et al. Surgical smoke and ultrafine particles. J Occup Med Toxicol. 2008;3.
Hill DS, O’Neill JK, Powell RJ, Oliver DW. Surgical smoke—a health hazard in the operating theatre: a study to quantify exposure and a survey of the use of smoke extractor systems in UK plastic surgery units. J Plast Reconstr Aesthet Surg. 2012;65:911–6.
Fletcher JN, Mew D, DesCoteaux JG. Dissemination of melanoma cells within electrocautery plume. Am J Surg. 1999;178:57–9.
Nduka CC, Poland N, Kennedy M, Dye J, Darzi A. Does the ultrasonically activated scalpel release viable airborne cancer cells? Surg Endosc. 1998;12:1031–4.
Ott DE, Moss E, Martinez K. Aerosol exposure from an ultrasonically activated (Harmonic) device. J Am Assoc Gynecol Laparosc. 1998;5:29–32.
Zhao C, Kim MK, Kim HJ, Lee SK, Chung YJ, Park JK. Comparative safety analysis of surgical smoke from transurethral resection of the bladder tumors and transurethral resection of the prostate. Urology. 2013;82(744):e9–14.
Takahashi H, Yamasaki M, Hirota M, Miyazaki Y, Moon JH, Souma Y, et al. Automatic smoke evacuation in laparoscopic surgery: a simplified method for objective evaluation. Surg Endosc. 2013;27:2980–7.
Al Sahaf OS, Vega-Carrascal I, Cunningham FO, McGrath JP, Bloomfield FJ. Chemical composition of smoke produced by high-frequency electrosurgery. Ir J Med Sci. 2007;176:229–32.
Lin YW, Fan SZ, Chang KH, Huang CS, Tang CS. A novel inspection protocol to detect volatile compounds in breast surgery electrocautery smoke. J Formos Med Assoc. 2010;109:511–6.
Gianella M, Hahnloser D, Rey JM, Sigrist MW. Quantitative Chemical analysis of surgical smoke generated during laparoscopic surgery with a vessel-sealing device. Surg Innov. 2013. doi:10.1177/1553350613492025.
Gatti JE, Bryant CJ, Noone RB, Murphy JB. The mutagenicity of electrocautery smoke. Plast Reconstr Surg. 1992;89:781–4.
Tomita Y, Mihashi S, Nagata K, Ueda S, Fujiki M, Hirano M, et al. Mutagenicity of smoke condensates induced by CO2-laser irradiation and electrocauterization. Mutat Res. 1981;89:145–9.
McKinley IB Jr, Ludlow MO. Hazards of laser smoke during endodontic therapy. J Endod. 1994;20:558–9.
Capizzi PJ, Clay RP, Battey MJ. Microbiologic activity in laser resurfacing plume and debris. Lasers Surg Med. 1998;23:172–4.
Ferenczy A, Bergeron C, Richart RM. Human papillomavirus DNA in CO2 laser-generated plume of smoke and its consequences to the surgeon. Obstet Gynecol. 1990;75:114–8.
Nicola JH, Nicola EM, Vieira R, Braile DM, Tanabe MM, Baldin DH. Speed of particles ejected from animal skin by CO2 laser pulses, measured by laser Doppler velocimetry. Phys Med Biol. 2002;47:847–56.
Gloster HM Jr, Roenigk RK. Risk of acquiring human papillomavirus from the plume produced by the carbon dioxide laser in the treatment of warts. J Am Acad Dermatol. 1995;32:436–41.
Taravella MJ, Weinberg A, May M, Stepp P. Live virus survives excimer laser ablation. Ophthalmology. 1999;106:1498–9.
Choi SH, Kwon TG, Chung SK, Kim TH. Surgical smoke may be a biohazard to surgeons performing laparoscopic surgery. Surg Endosc. 2014. doi:10.1007/s00464-014-3472-3.
Fan JKM, Chan FSY, Chu KM. Surgical smoke. Asian J Surg. 2009;32:253–7.
Garden JM, O’Banion MK, Shelnitz LS, Pinski KS, Bakus AD, Reichmann ME, et al. Papillomavirus in the vapor of carbon dioxide laser-treated verrucae. JAMA. 1988;259:1199–202.
Baggish MS, Poiesz BJ, Joret D, Williamson P, Refai A. Presence of human immunodeficiency virus DNA in laser smoke. Lasers Surg Med. 1991;11:197–203.
Fitzgerald JE, Malik M, Ahmed I. A single-blind controlled study of electrocautery and ultrasonic scalpel smoke plumes in laparoscopic surgery. Surg Endosc. 2012;26:337–42.
Baggish MS, Elbakry M. The effects of laser smoke on the lungs of rats. Am J Obstet Gynecol. 1987;156:1260–5.
Ball K. Update for nurse anesthetists. Part 1. The hazards of surgical smoke. AANA J. 2001;69:125–32.
Ulmer BC. The hazards of surgical smoke. AORN J. 2008;87:721–34.
Edwards BE, Reiman RE. Comparison of current and past surgical smoke control practices. AORN J. 2012;95:337–50.
Laser/electrosurgery plume. (The Occupational Safety and Health Administration (OSHA) web site) https://www.osha.gov/SLTC/laserelectrosurgeryplume/. Accessed 16 Oct 2014.
Diathermy and surgical smoke. (The Health and Safety Executive (HSE) web site) http://www.hse.gov.uk/healthservices/diathermy-emissions.htm. Accessed 16 Oct 2014.
Surgical Smoke. (British Occupational Hygiene Society web site) http://www.bohs.org/uploadedFiles/Groups/Pages/Surgical_smoke.pdf. Accessed 16 Oct 2014.
Kubo H. Medical engineering, electrical instruments and medical gas, guideline for surgical practice (in Japanese). Nihon Shujutsu Igaku Kaishi. 2013;34:s98–113.
Alp E, Bijl D, Bleichrodt RP, Hansson B, Voss A. Surgical smoke and infection control. J Hosp Infect. 2006;62:1–5.
American College of Chest Physicians. Aerosol consensus statement. Consensus conference on aerosol delivery. Chest. 1991;100:1106–9.
Gates MA, Feskanich D, Speizer FE, Hankinson SE. Operating room nursing and lung cancer risk in a cohort of female registered nurses. Scand J Work Environ Health. 2007;33:140–7.
Pukkala E, Martinsen JI, Lynge E, Gunnarsdottir HK, Sparen P, Tryggvadottir L, et al. Occupation and cancer—follow-up of 15 million people in five Nordic countries. Acta Oncol. 2009;48:646–790.
Navarro-Meza MC, Gonzalez-Baltazar R, Aldrete-Rodriguez MG, Carmona-Navarro DE, Lopez-Cardona MG. Respiratory symptoms caused by the use of electrocautery in physicians being trained in surgery in a Mexican hospital. Rev Peru Med Exp Salud Publica. 2013;30:41–4.
Ball K. Compliance with surgical smoke evacuation guidelines: implications for practice. AORN J. 2010;92:142–9.
Ball K. Surgical smoke evacuation guidelines: Compliance among perioperative nurses. AORN J. 2010;92:e1–23.
Le Moual N, Varraso R, Zock JP, Henneberger P, Speizer FE, Kauffmann F, et al. Are operating room nurses at higher risk of severe persistent asthma? The nurses’ health study. J Occup Environ Med. 2013;55:973–7.
Hallmo P, Naess O. Laryngeal papillomatosis with human papillomavirus DNA contracted by a laser surgeon. Eur Arch Otorhinolaryngol. 1991;248:425–7.
Weld KJ, Dryer S, Ames CD, Cho K, Hogan C, Lee M, et al. Analysis of surgical smoke produced by various energy-based instruments and effect on laparoscopic visibility. J Endourol. 2007;21:347–51.
Heinsohn PA, Jewett DL, Balzer L, Bennett CH, Seipel P, Rosen A. Aerosols created by some surgical power tools: particle size distribution and qualitative hemoglobin content. Appl Occup Environ Hyg. 1991;6:773–6.
Nezhat C, Winer WK, Nezhat F, Nezhat C, Forrest D, Reeves WG. Smoke from laser surgery: is there a health hazard? Lasers Surg Med. 1987;7:376–82.
Wisniewski PM, Warhol MJ, Rando RF, Sedlacek TV, Kemp JE, Fisher JC. Studies on the transmission of viral disease via the CO2 laser plume and ejecta. J Reprod Med. 1990;35:1117–23.
Barrett WL, Garber SM. Surgical smoke—a review of the literature. Is this just a lot of hot air? Surg Endosc. 2003;17:979–87.
Pierce JS, Lacey SE, Lippert JF, Lopez R, Franke JE. Laser-generated air contaminants from medical laser applications: a state-of-the-science review of exposure characterization, health effects, and control. J Occup Environ Hyg. 2011;8:447–66.
Agents classified by the IARC monographs, vol. 1–109. (The International Agency for Research on Cancer (IARC) web site) http://monographs.iarc.fr/ENG/Classification/. Accessed 16 Oct 2014.
EH40/2005 Workplace Exposure Limits. (Health and Safety Executive web site) http://books.hse.gov.uk/hse/public/saleproduct.jsf?catalogueCode=9780717664467. Accessed 16 Oct 2014.
Wu JS, Luttmann DR, Meininger TA, Soper NJ. Production and systemic absorption of toxic byproducts of tissue combustion during laparoscopic surgery. Surg Endosc. 1997;11:1075–9.
Sagar PM, Meagher A, Sobczak S, Wolff BG. Chemical composition and potential hazards of electrocautery smoke. Br J Surg. 1996;83:1792.
Tseng HS, Liu SP, Uang SN, Yang LR, Lee SC, Liu YJ, et al. Cancer risk of incremental exposure to polycyclic aromatic hydrocarbons in electrocautery smoke for mastectomy personnel. World J Surg Oncol. 2014;12:31.
Agency for Toxic Substances and Disease Registry. Toxicological Profile for Toluene (Department of Health and Human Services web site) http://www.atsdr.cdc.gov/ToxProfiles/TP.asp?id=161&tid=29. Accessed 16 Oct 2014.
Ferenczy A, Bergeron C, Richart RM. Carbon dioxide laser energy disperses human papillomavirus deoxyribonucleic acid onto treatment fields. Am J Obstet Gynecol. 1990;163:1271–4.
Ikramuddin S, Lucus J, Ellison EC, Schirmer WJ, Melvin WS. Detection of aerosolized cells during carbon dioxide laparoscopy. J Gastrointest Surg. 1998;2:580–83; discussion 84.
Reymond MA, Schneider C, Kastl S, Hohenberger W, Kockerling F. The pathogenesis of port-site recurrences. J Gastrointest Surg. 1998;2:406–14.
Sawchuk WS, Weber PJ, Lowy DR, Dzubow LM. Infectious papillomavirus in the vapor of warts treated with carbon dioxide laser or electrocoagulation: detection and protection. J Am Acad Dermatol. 1989;21:41–9.
Armstrong DN, Ambroze WL, Schertzer ME, Orangio GR. Harmonic Scalpel vs. electrocautery hemorrhoidectomy: a prospective evaluation. Dis Colon Rectum. 2001;44:558–64.
Amaral JF. The experimental development of an ultrasonically activated scalpel for laparoscopic use. Surg Laparosc Endosc. 1994;4:92–9.
Kokosa JM, Eugene J. Chemical composition of laser-tissue interaction smoke plume. J Laser Appl. 1989;3:59–63.
Brandon HJ, Young VL. Characterization and removal of electrosurgical smoke. Surg Serv Manag. 1997;3:14–6.
Hirata S. Building equipment of surgical room, guideline for surgical practice (in Japanese). Nihon Shujutsu Igaku Kaishi. 2013;34:s131–6.
Schultz L. An analysis of surgical smoke plume components, capture, and evacuation. AORN J. 2014;99:289–98.
Coia JE, Ritchie L, Adisesh A, Makison Booth C, Bradley C, Bunyan D, et al. Guidance on the use of respiratory and facial protection equipment. J Hosp Infect. 2013;85:170–82.
Benson SM, Novak DA, Ogg MJ. Proper use of surgical n95 respirators and surgical masks in the OR. AORN J. 2013;97:457–67.
Chemical Sampling Information (The Occupational Safety and Health Administration (OSHA) web site). https://www.osha.gov/dts/chemicalsampling/toc/toc_chemsamp.html. Accessed 16 Oct 2014.
Acknowledgments
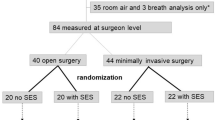
We thank Naoto Aihara for his assistance in producing the figure.
Conflict of interest
Kae Okoshi and co-authors have no conflicts of interest to declare.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Okoshi, K., Kobayashi, K., Kinoshita, K. et al. Health risks associated with exposure to surgical smoke for surgeons and operation room personnel. Surg Today 45, 957–965 (2015). https://doi.org/10.1007/s00595-014-1085-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00595-014-1085-z