Abstract
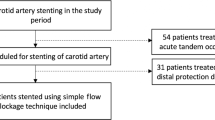
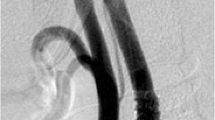
A variety of distal emboli protection systems are in development for carotid angioplasty and stenting, each of which may be associated with its own unique capability to capture emboli. This retrospective study was undertaken to compare the incidence and type of peri-procedural (1-month) neurological events using a variety of microembolization protection strategies. This is a retrospective review of 127 consecutive procedures performed over a period of 4 years solely by vascular surgeons. This analysis was restricted to outcomes associated with the treatment of carotid bifurcation lesions. Overall, angioplasty and stenting was performed without distal protection in 32 patients. Of the remaining 95 patients, protection devices included a distal occlusion balloon (n = 18), a Filterwire (n = 54), an Accunet filter (n = 22), and a Sci-pro device (n = l). Patients were considered at high risk for open surgery due to prior endarterectomy (n = 43), radiation (n = 9), high lesion (n = 3), or cardiopulmonary comorbididity (n = 37). A majority of patients (n = 92; 73%) had an asymptomatic >80% stenosis. All procedures were done without sedation and with continuous neurological monitoring. Periprocedural neurological events were classified as a transient ischemic attack (TIA), minor or major stroke, or seizure. In the absence of distal protection, TIAs lasting fewer than 10 min were observed in four patients with an additional patient suffering a minor stroke. Seizure-like activity was observed in two patients during balloon inflation. Among those in whom a filter-based embolization protection device was utilized, TIAs were noted in three patients and none developed either a minor or major stroke. Periprocedural events were not observed with the use of distal balloon protection, although one patient had a TIA 3 weeks after intervention. All neurological events occurred during post-stent dilatation and only among patients with prior neurological symptoms and de novo lesion. Intra-operative neurological events were significantly more common in the absence of protected stenting (n = 7, 21.8%), when compared to filter protection (n = 3, 4%) or complete distal occlusion (n = 0, 0%) (p = 0.0025). However, the majority of these events were transient without permanent neurological deficit. The overall incidence of major stroke/mortality rate was 0.8%. Carotid angioplasty and stenting is a safe and effective procedure when undertaken with adequate distal protection. Adverse neurological events can be minimized by avoiding aggressive post-stent dilatation.



Similar content being viewed by others
References
Yadav JS, Wholey MH, Kuntz RE, Fayad P, Katzen BT, Mishkel GL, et al. (2004) Protected carotid-artery stenting versus endarterectomy in high-risk patients. N Engl J Med 351:1493–501
Kasirajan K, Schneider PA, Kent KC (2003) Emboli protection filters for cerebral protection during carotid angioplasty and stenting. J Endovasc Ther 10:21–27
Crawley F, Stygall J, Lunn S, et al. (2000) Comparison of micro embolism detected by transcranial Doppler and neuropsychological sequel of carotid surgery and percutaneous transluminal angioplasty. Stroke 31:1329–1334
Kasirajan K Carotid angioplasty and stenting: how I do it? In: Schneider, Bohannon, Siiva (eds). Carotid interventions, 1st edn. Marcel Dekker Inc.:New York, pp 149–164
Britt PM, Heiserman JE, Snider RM, et al. (2000) incidence of post angiographic abnormalities revealed by diffusion-weighted MR imaging. AJNR Am J Neuroradiol 21:55–59
Bendszus M, Koltzenberg M, Burger R, et al. (1999) Silent embolism in diagnostic cerebral angiography and neurointerventional procedures: a prospective study. Lancet 354:1594–1597
Flach HZ, Ouhlous M, Hendricks JM, van Sambeek MR, Veenland JF, Koudstall PJ, et al. (2004) Cerebral ischemia after carotid intervention. J Endovasc Ther 11:251–257
Johansen O, Brekke M, Stromme JH, et al. (1998) Myocardial damage during percutaneous transluminal coronary angioplasty as evidenced by troponin T measurements. Eur Heart J 19:112–117
CARESS Steering Committee (2003) Carotid revascularization using endarterectomy or stenting systems (CARESS): phase I clinical trial. J Endovasc Ther 10:1021–1030
Ohki T, Roubin GS, Veith FJ, et al. (1999) Efficacy of a filter device in the prevention of embolic events during carotid angioplasty and stenting: an ex vivo analysis. J Vase Surg 30:1034–1044
Dion JE, Gates PC, Fox AJ, et al. (1987) Clinical events following neuroangiography: a prospective study. Stroke 18:997–1004
Hobson RW, Howard VJ, Roubin GS, Ferguson RD, Brott TG, Howard G, et al. (2004) Credentialing of surgeons as interventionists for carotid artery stenting: experience from the lead-in phase of CREST. J Vas Surg 40:952–957
Macdonald S, Cleveland TJ, Gaines P, et al. (2004) Neuropsychometric outcomes of unprotected and protected carotid stenting (EmboShield): a randomized trail (abstract). J Vas Interv Radiol 15(suppl 1):S184–S185
Mathias K. Results of European trials. Presented at the Society of Interventional Radiology 29th Annual Scientific Meeting, Phoenix, 25–30 March 2004
Wholey MH, Al-Mubarek N, Wholey MH. (2003) Updated review of the global carotid artery stent registry. Cathet Cardiovasc Interv 60:259–66
Mas JL, Chatellier G, Branchereau A, Becquemin JP, Bonneville JF, Crochet D, et al. (2004) Carotid angioplasty and stenting with and without cerebral protection: clinical alert from15 the Endarterectomy Versus Angioplasty in Patients with Severe Carotid Stenosis (EVA-38) trial. Stroke 35:E18–21
Vermeer SE, Prins ND, den Heijer T, et al. (2003) Silent brain infarcts and risk of dementia and cognitive decline. N Engl J Med 348:1215–1222
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Kasirajan, K., Milner, R., Dodson, T.F. et al. Neuroprotection During Carotid Angioplasty and Stenting: Comparison of No Protection, Occlusion, or Filters. Int J Angiol 15, 20–24 (2006). https://doi.org/10.1007/s00547-006-2067-9
Issue Date:
DOI: https://doi.org/10.1007/s00547-006-2067-9